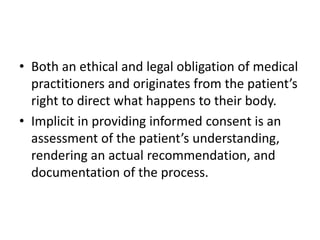
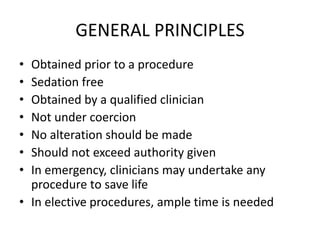
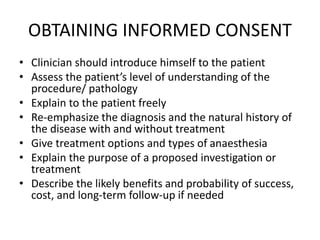
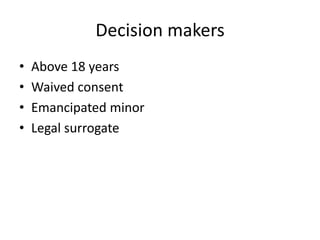
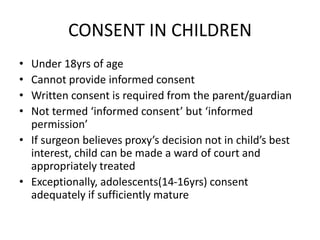
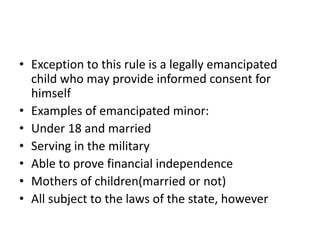
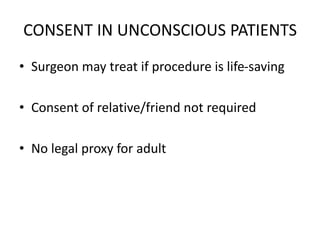
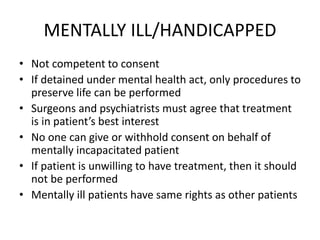
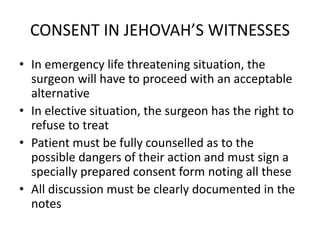
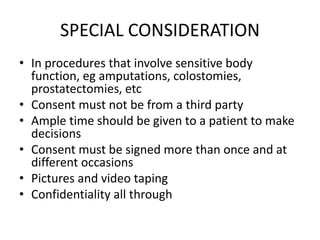
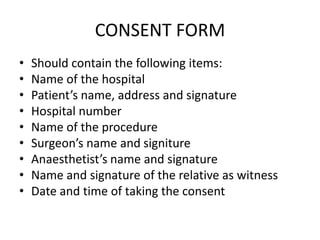
This document discusses informed consent in surgery. It outlines the general principles of informed consent, including that consent must be given voluntarily by a competent patient who understands the risks and benefits of the proposed treatment. The document also covers the different types of consent and how consent is obtained, including providing full disclosure of the procedure to the patient. Special considerations for obtaining consent from children, unconscious patients, and those with mental illnesses are also reviewed.


![References
• Slim K, Bazin JE. From informed consent to
shared decision-making in surgery. J Visc Surg.
2019 Jun;156(3).181-184
• Shah P, Thornton I, Turrin D, et al. Informed
consent. [Updated 2022 June 11]
• Bashir Bin Yunus. Compendium for surgery
tutorials.](https://image.slidesharecdn.com/informedconsentinsurgery-230629172149-c4394083/85/INFORMED-CONSENT-IN-SURGERY-pptx-24-320.jpg)