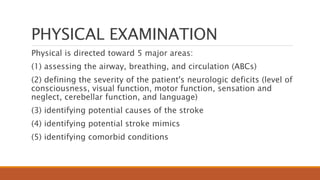
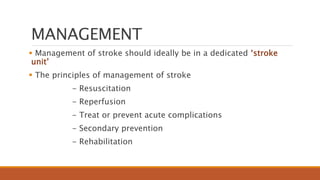
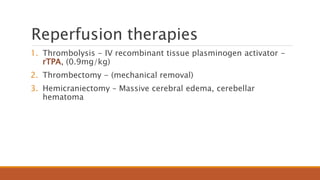
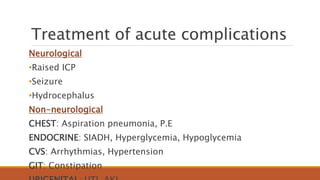
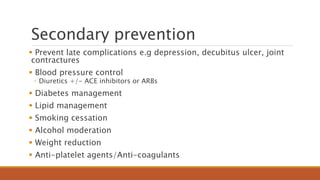
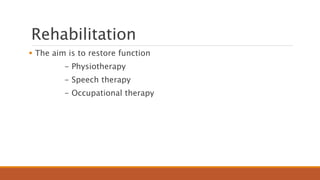
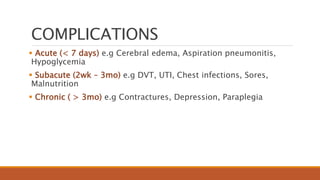
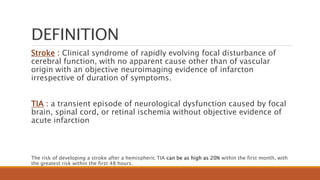
This document provides an overview of the management of acute stroke. It defines stroke and transient ischemic attack, and discusses the epidemiology, classification, risk factors, pathophysiology, clinical presentation, diagnosis, management, complications and prognosis of stroke. The management involves resuscitation, reperfusion therapies like thrombolysis and thrombectomy, treating complications, secondary prevention including blood pressure and diabetes control, and rehabilitation. The document emphasizes the importance of specialized stroke units and timely management to improve outcomes for patients with acute stroke.
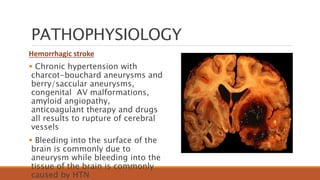
![EPIDEMIOLOGY
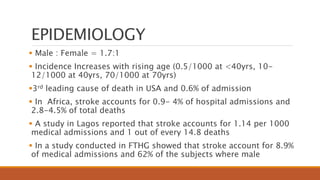
Common neurological emergency associated with morbidity and
mortality
Stroke is the 4th most common neurological disorder after
headache, epilepsy and neuropathy
Someone suffers a stroke every 53 seconds and someone dies
from stroke every 3.3 minutes
Second leading cause of preventable deaths in adults worldwide.
15 million cases annually [WHO]
- 5 million deaths
- 5 million left with disability
- 5 million recover](https://image.slidesharecdn.com/strokebyadamu2-230201141925-5369218d/85/Stroke-pptx-6-320.jpg)