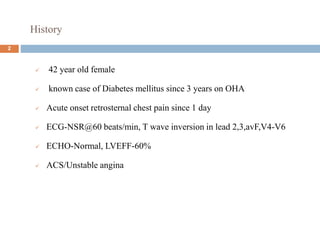
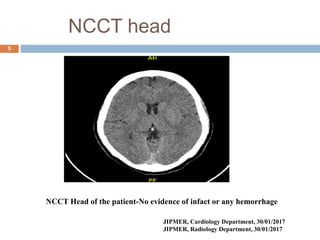
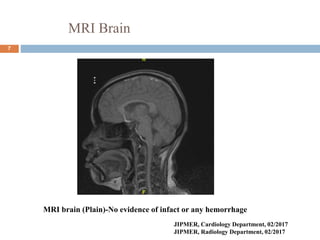
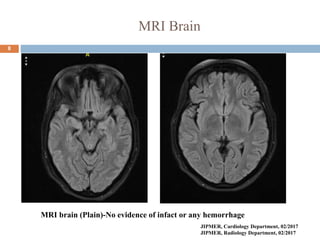
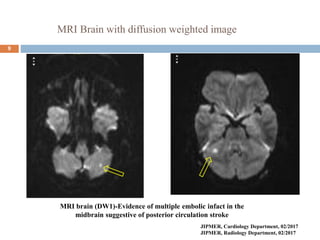
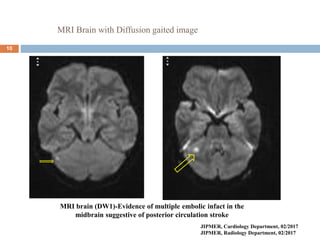
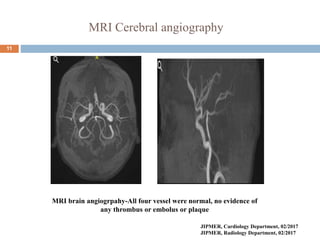
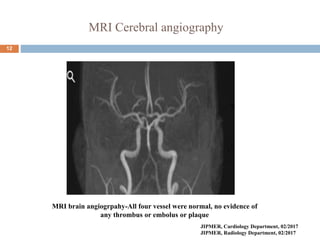
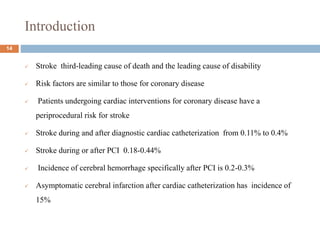
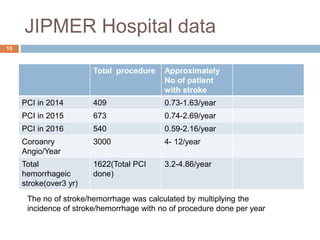
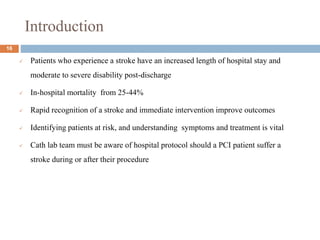
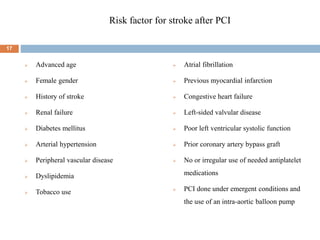
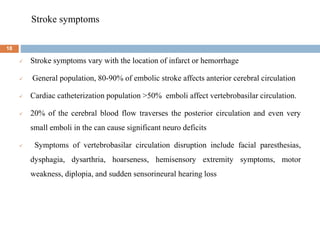
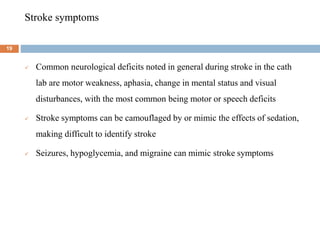
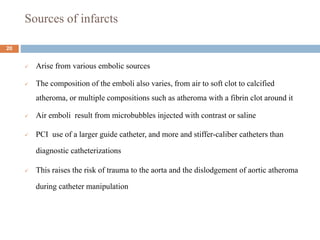
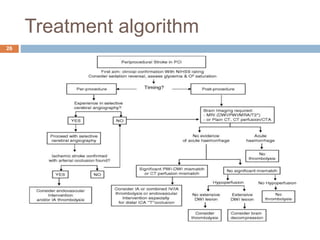
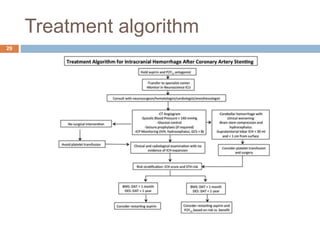
The document details a case study of a 42-year-old female with diabetes who experienced a posterior circulation stroke following a successful transradial PCI procedure. MRI results showed multiple embolic infarcts in the midbrain, although cerebral angiography indicated no thrombus or embolus. The document discusses the risks, symptoms, responses, and treatment algorithms related to stroke during and after PCI procedures, emphasizing the importance of rapid recognition and intervention.