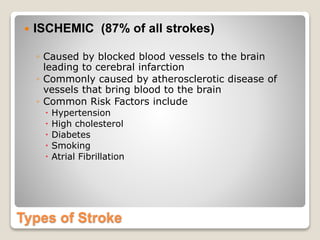
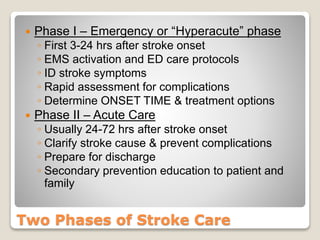
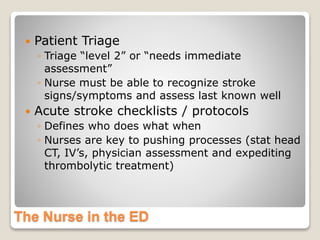
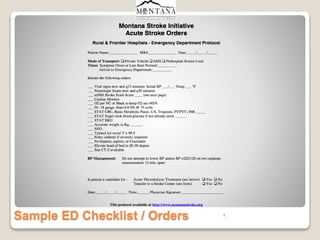
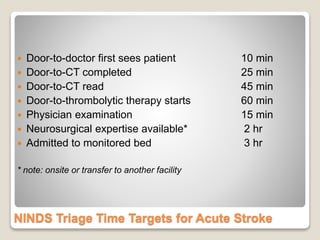
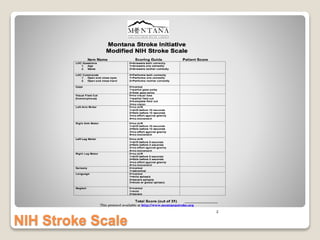
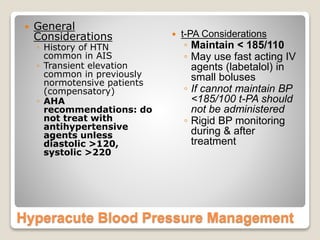
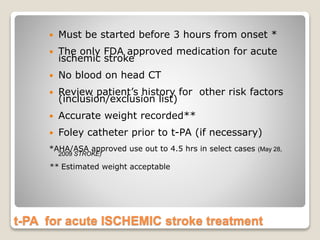
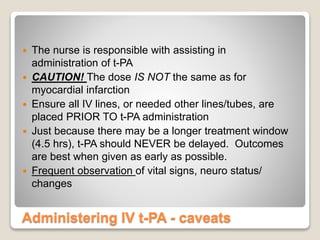
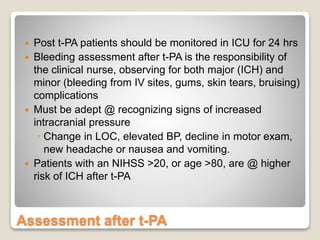
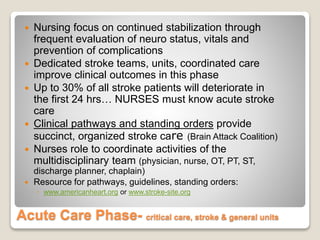
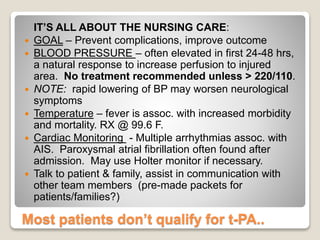
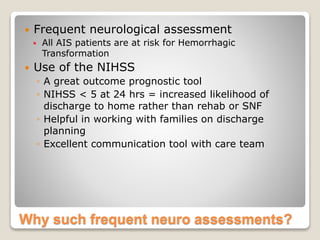
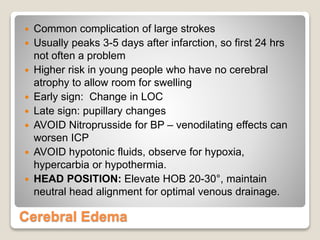
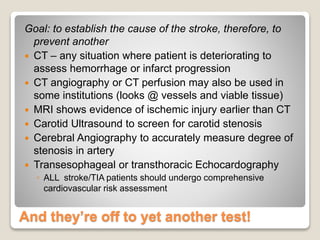
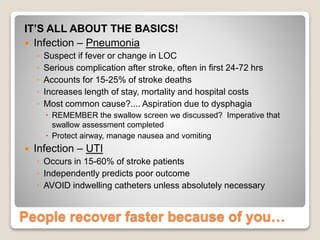
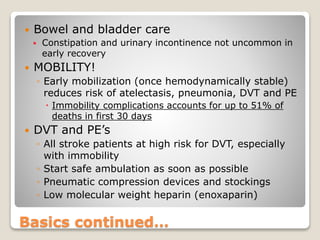
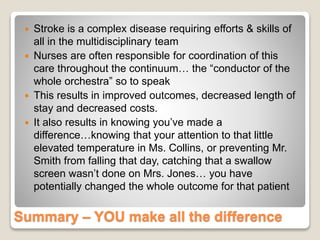
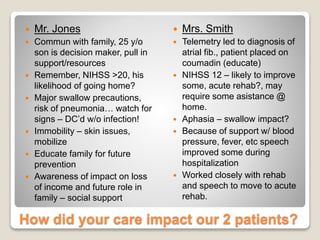
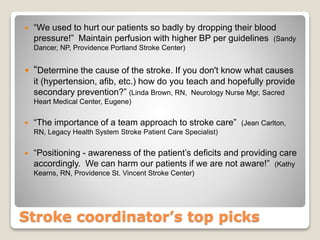
Mr. Jones, a 57-year-old successful businessman, suffered a severe ischemic stroke while out to dinner with friends. He received t-PA and other treatments but was still left with major deficits. Nursing plays a pivotal role in acute stroke care from the emergency response through hospitalization, with the goals of preventing complications, improving outcomes, and preparing patients and families for discharge and secondary prevention. Common complications include cerebral edema, fever, arrhythmias, and hemorrhagic transformation. Frequent neurological assessments and careful management of vital signs are important aspects of nursing care. Additional tests help determine the cause of the stroke to guide further prevention efforts.