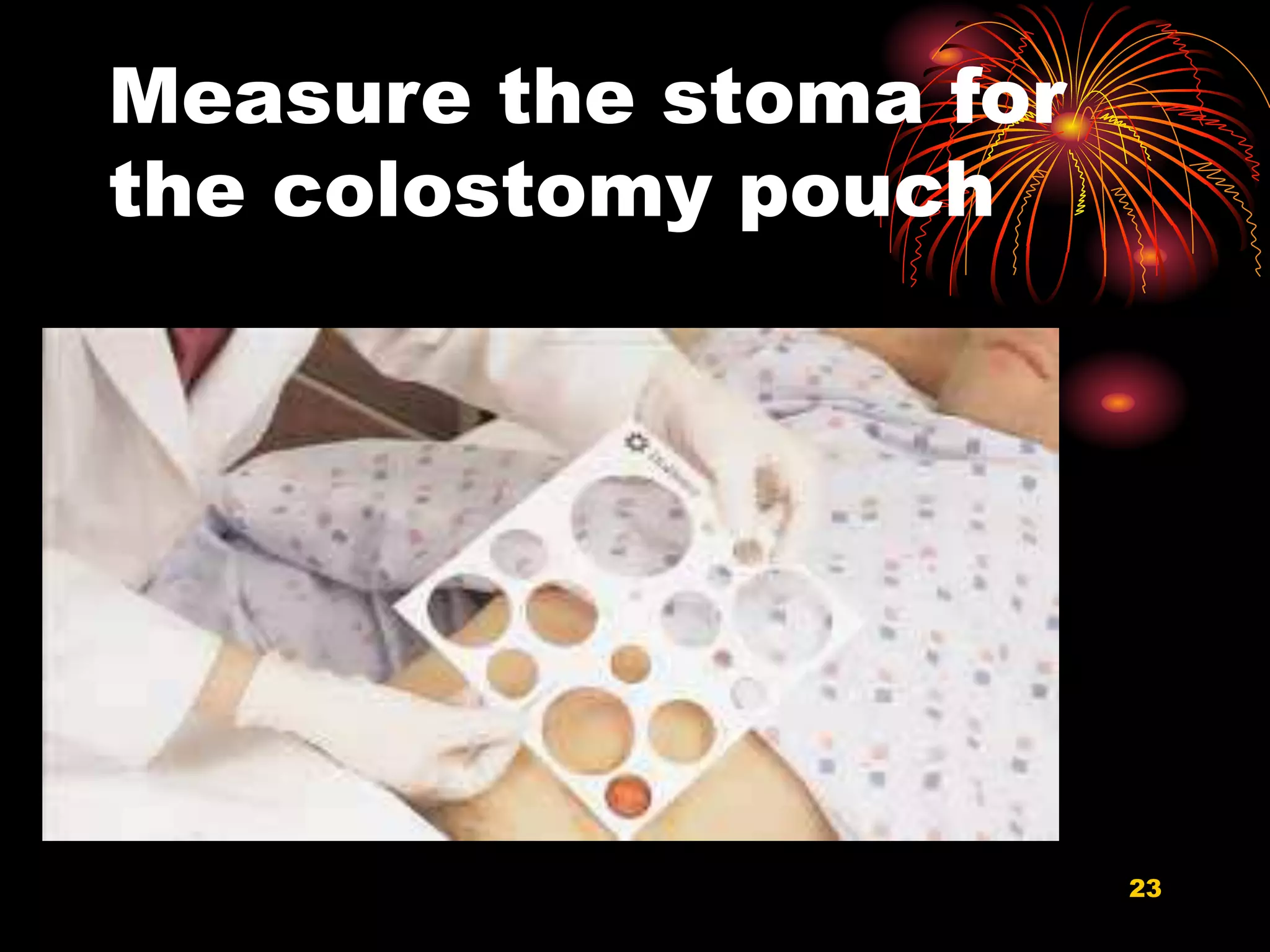
This document provides information about stomas, including definitions and types. It discusses colostomies and ileostomies, which are artificial openings of the colon or ileum onto the abdominal surface. Characteristics and indications for stomas are described. The document outlines preoperative management and nursing care before and after stoma surgery. Potential postoperative complications are listed. Information is provided about appliances and how to change a stoma bag.