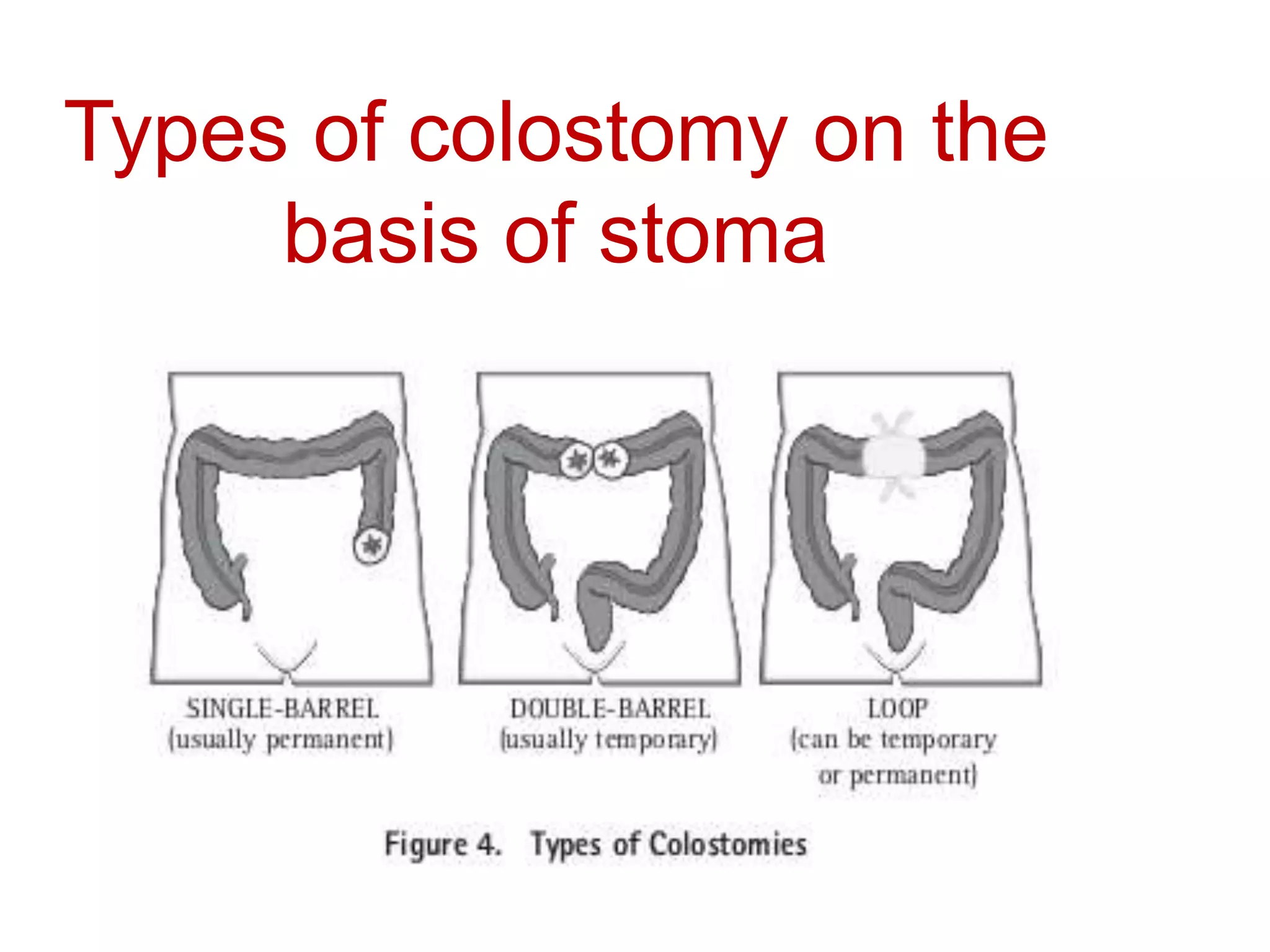
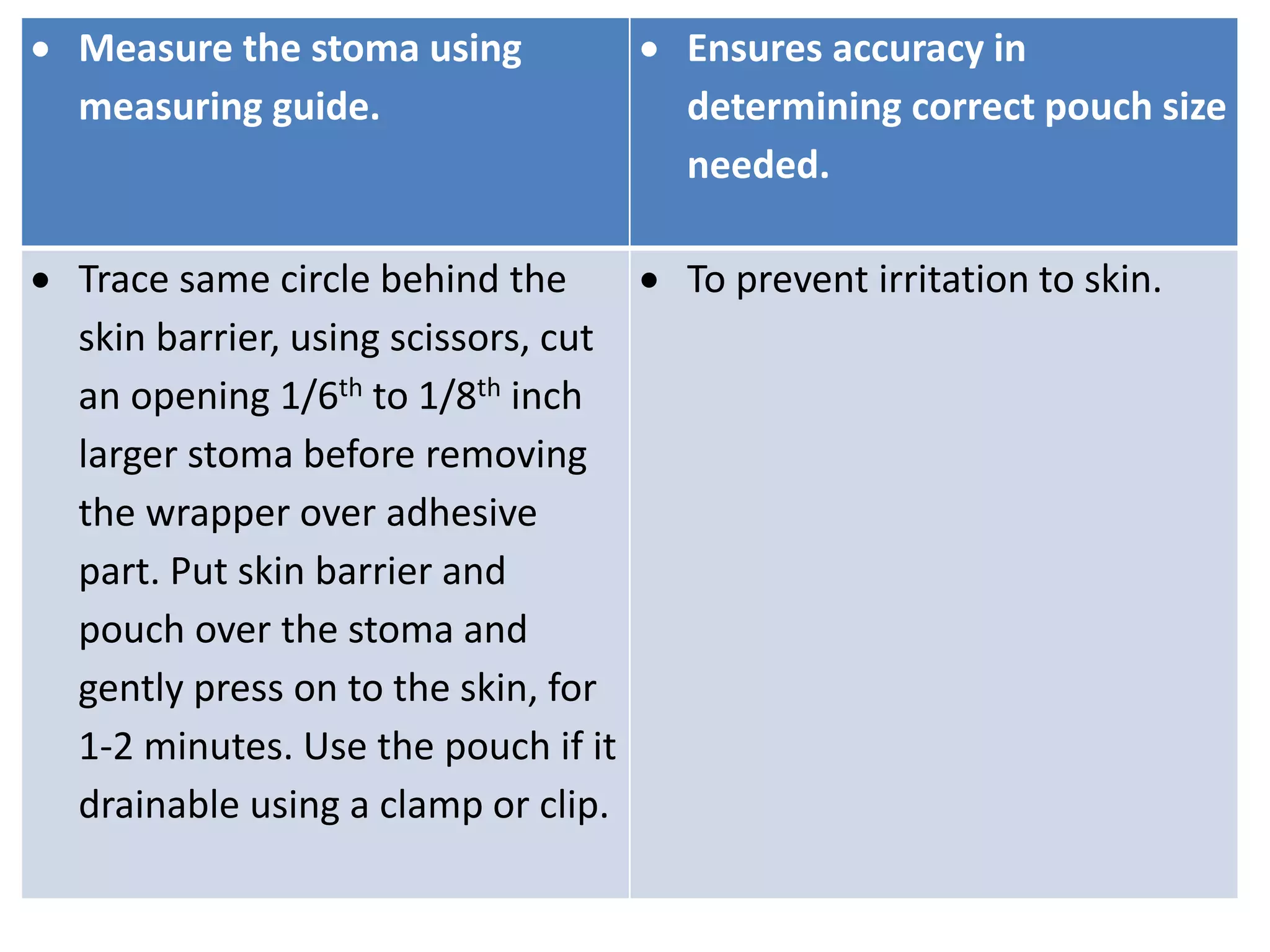
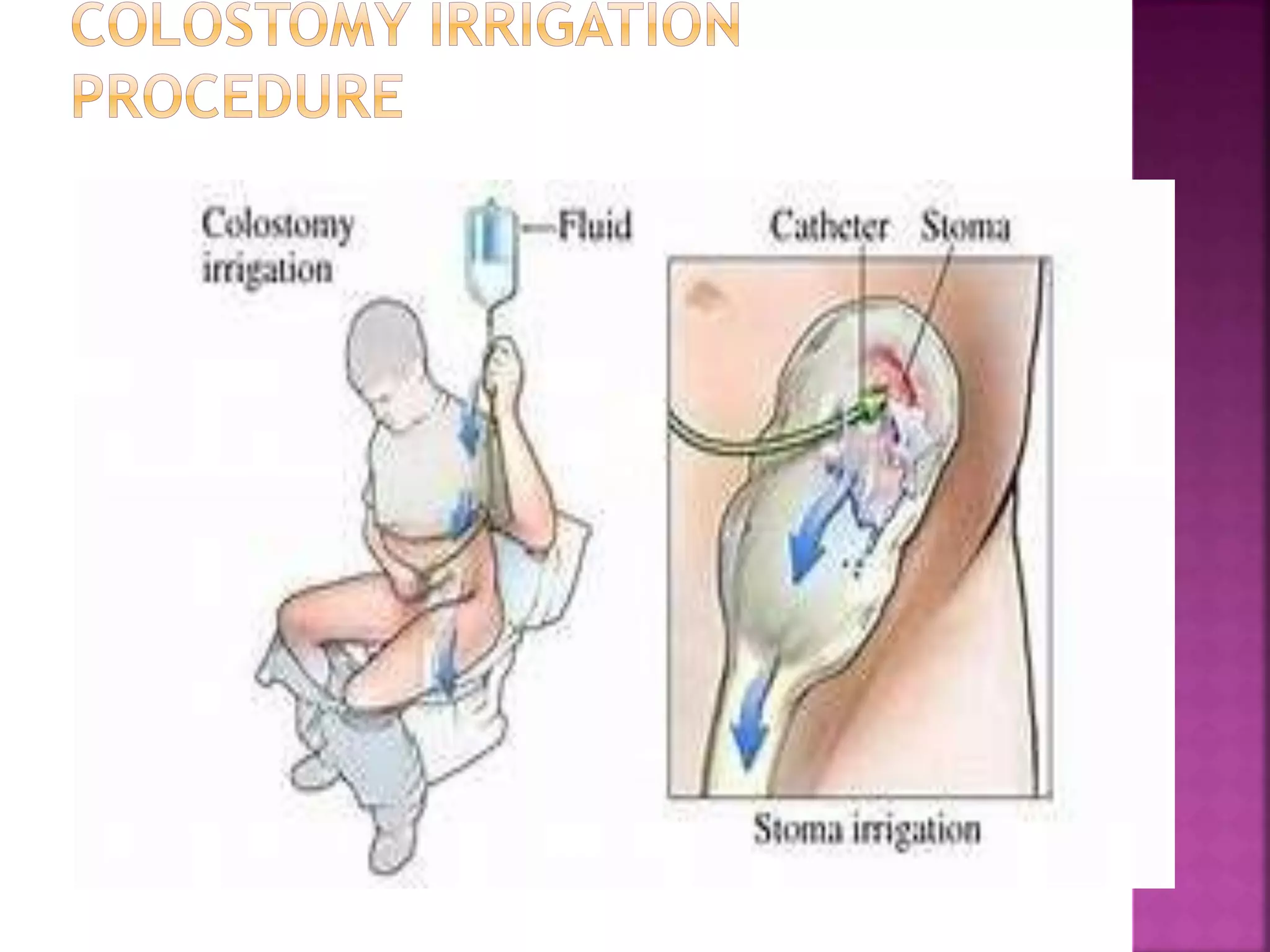
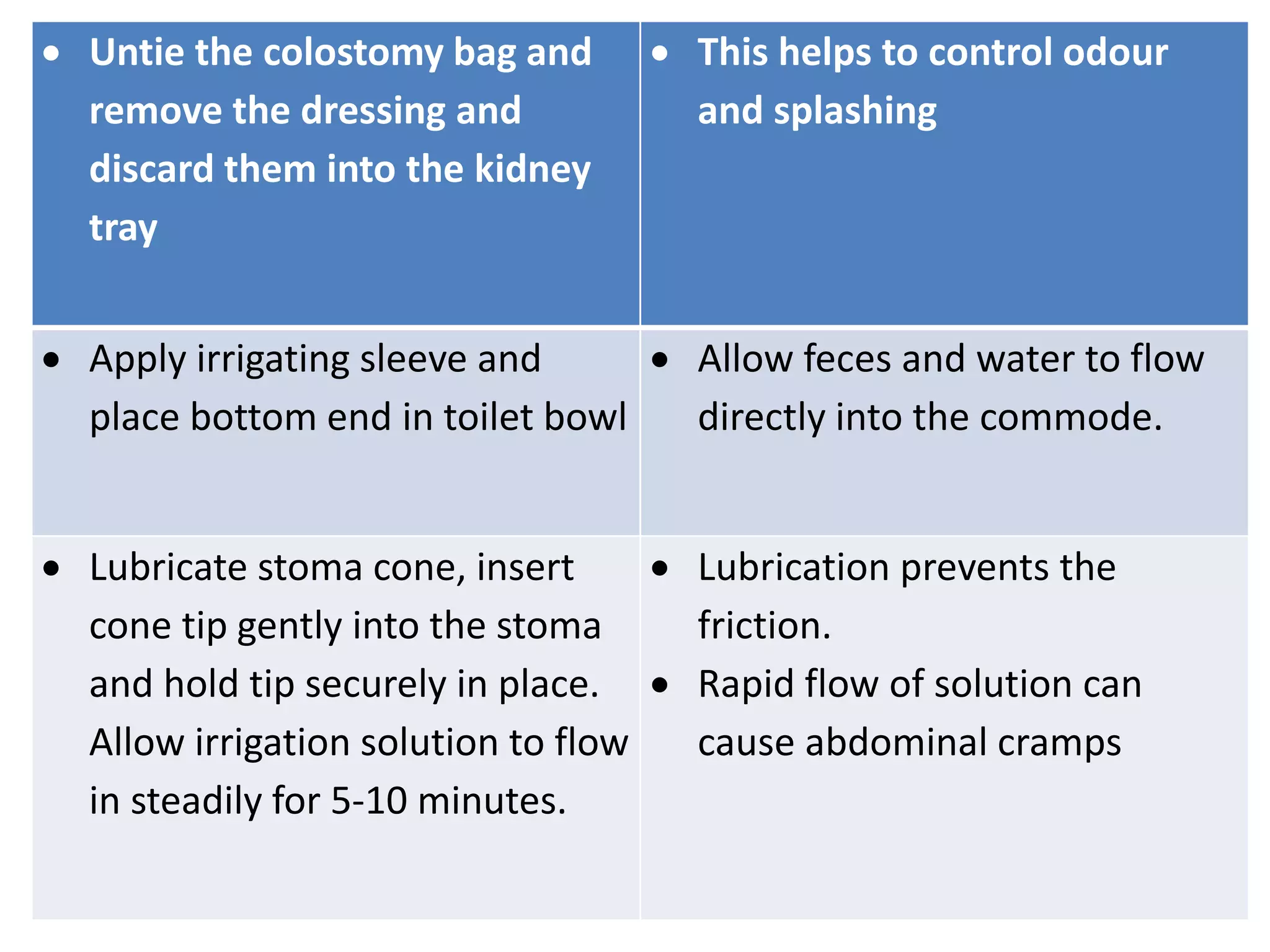
A colostomy is a surgical procedure where part of the large intestine is diverted through an opening in the abdominal wall called a stoma. This creates an artificial path for waste to exit the body. The document discusses the different types of colostomies based on location and stoma construction. It also covers potential complications, nursing care after surgery, diet guidelines, and proper pouch and stoma maintenance.