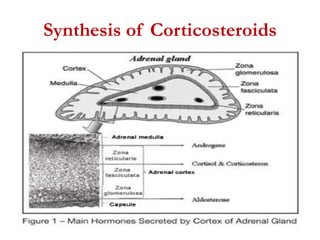
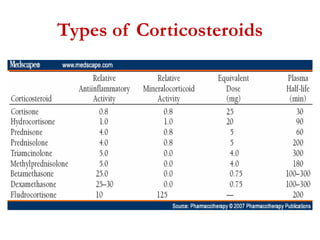
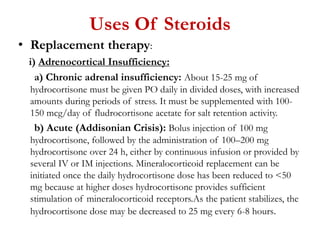
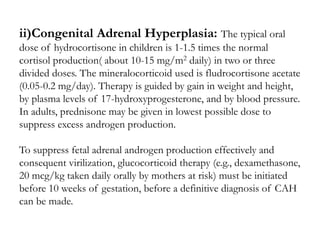
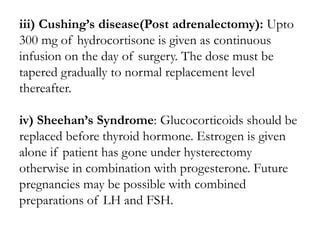
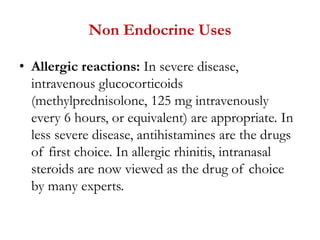
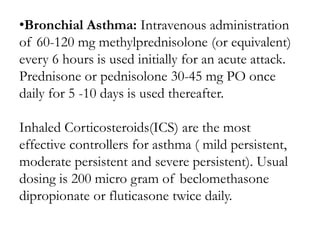
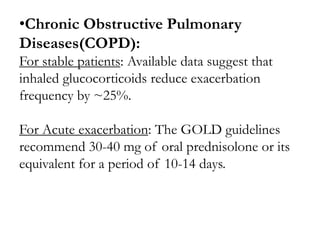
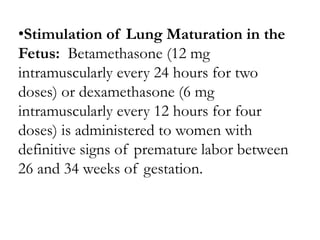
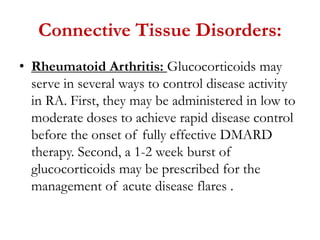
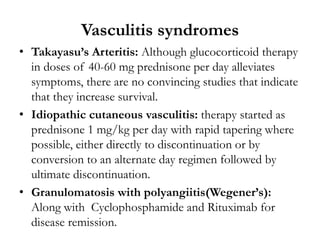
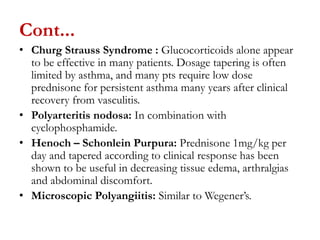
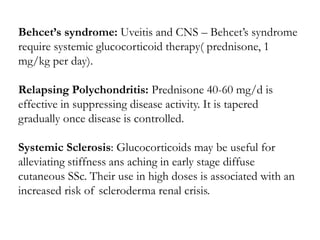
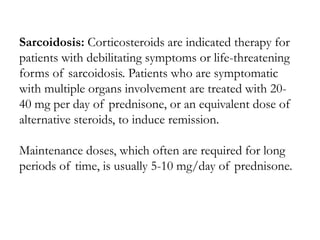
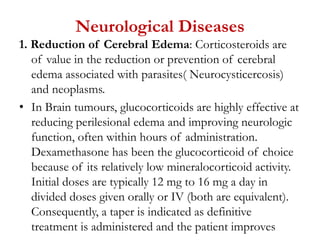
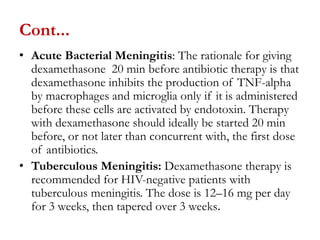
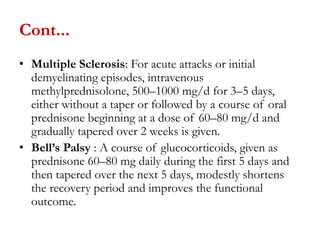
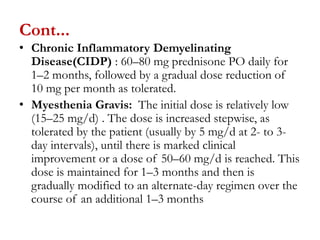
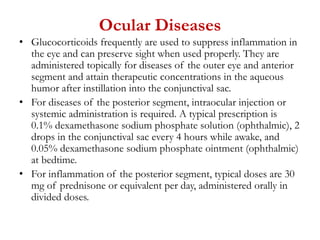
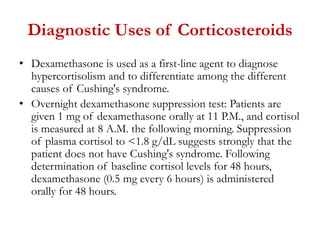
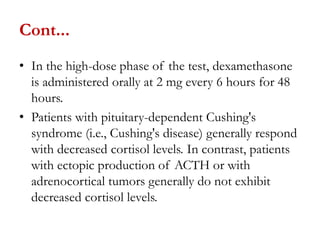
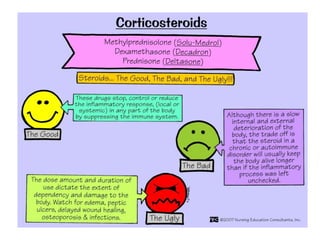
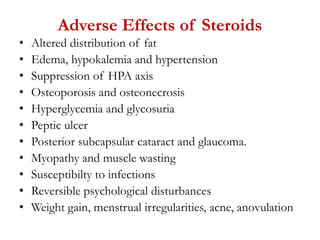
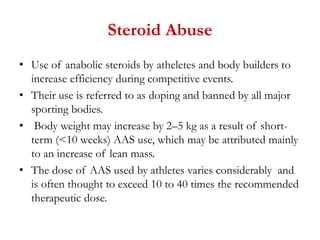
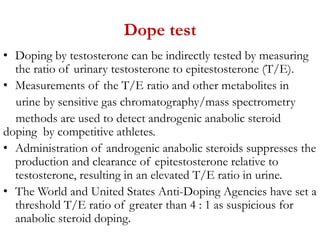
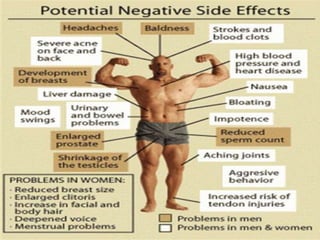
The document provides a detailed overview of corticosteroids, including their types, actions, and various medical applications such as replacement therapy for adrenal insufficiency and treatment for autoimmune diseases. It outlines specific dosing regimens and therapeutic strategies for conditions like rheumatoid arthritis, asthma, and inflammatory bowel diseases, emphasizing both systemic and local steroid usage. Additionally, it covers the roles of glucocorticoids in managing complications from infectious diseases, neurological conditions, and organ transplantation.