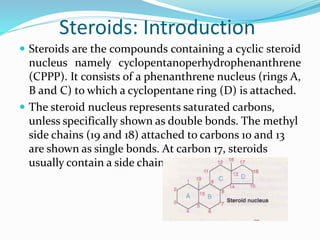
Steroids are compounds containing a cyclic steroid nucleus. They include mineralocorticoids like aldosterone, glucocorticoids like cortisol, and sex hormones. Glucocorticoids have effects on metabolism, inflammation, immunity, and more. They are used to treat conditions like inflammatory bowel disease. Long term steroid use can suppress the HPA axis and cause adverse effects, so tapering is important. During stress and surgery, steroids may need to be increased or supplemented to avoid adrenal insufficiency.




![Action of Mineralocorticoid
Major endogenous mineralocorticoid is aldosterone. It
acts in DCT of the kidney to cause reabsorption of Na+
and excretion of K+ and H+.
Thus, excess of mineralocorticoids can lead to retention of
sodium and water (hypertension and edema),
hypokalemia and alkalosis whereas Addison’s disease
(deficiency of adrenal corticoids) is characterized by
hyperkalemia, acidosis and hypotension.
Aldosterone is also involved in causing myocardial
remodeling associated with CHF and the drugs
blocking this effect [spironolactone, ACE inhibitors,
angiotensin receptor antagonists (ARBs) and β blockers]
decrease the mortality in patients with CHF.](https://image.slidesharecdn.com/steroids-converted-191111101956/85/Steroids-converted-7-320.jpg)

















