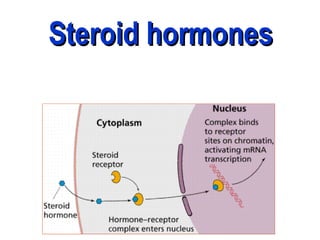
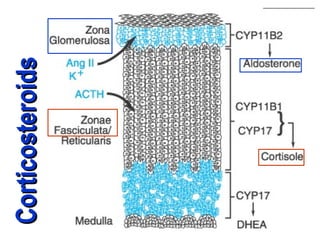
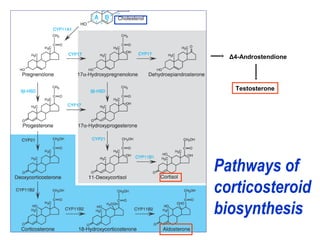
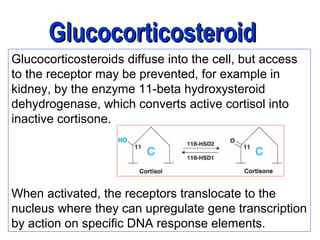
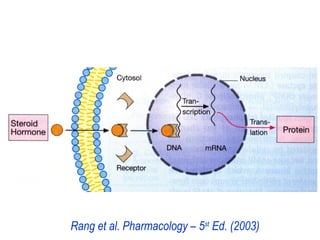
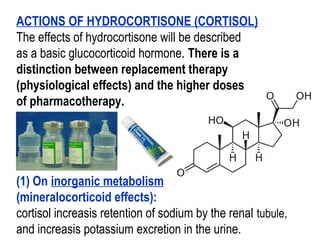
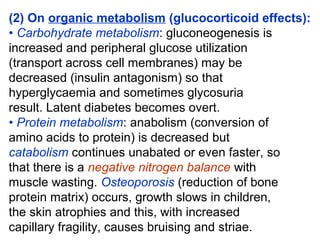
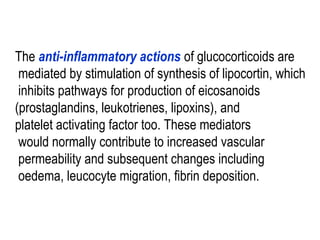
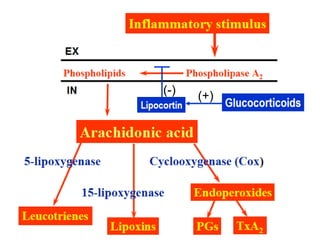
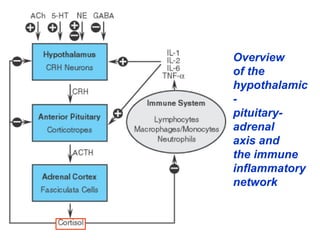
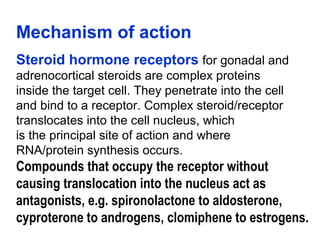
1. Steroid hormones include corticosteroids and sex hormones. Corticosteroids such as cortisol act through intracellular receptors to regulate processes like carbohydrate metabolism, protein metabolism, and the inflammatory response.
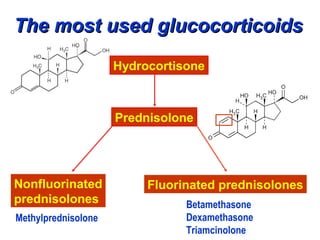
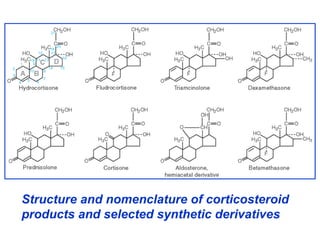
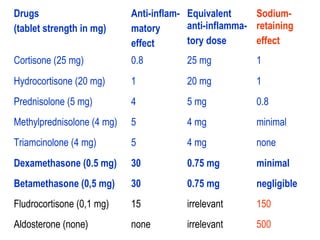
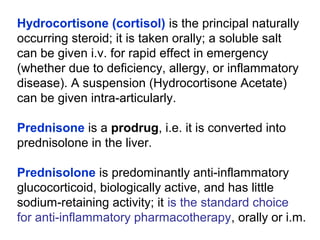
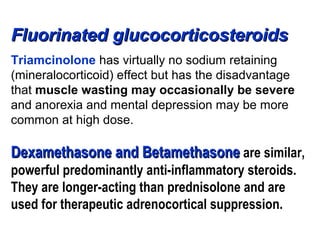
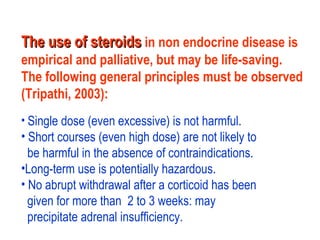
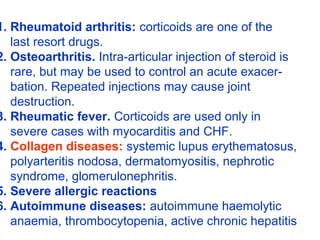
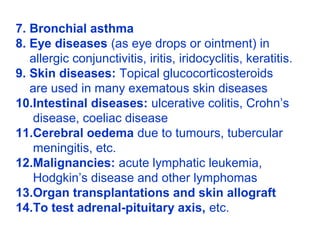
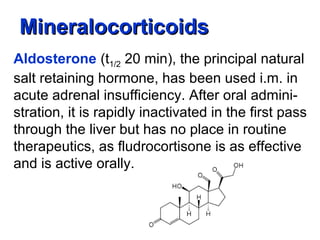
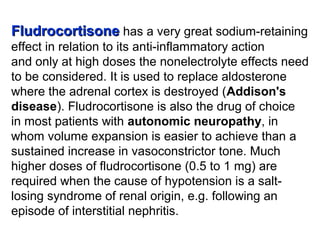
2. Glucocorticoids like hydrocortisone and prednisone are used for conditions like rheumatoid arthritis, asthma, and inflammatory bowel disease. Mineralocorticoids including fludrocortisone help retain sodium.
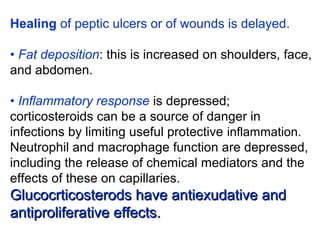
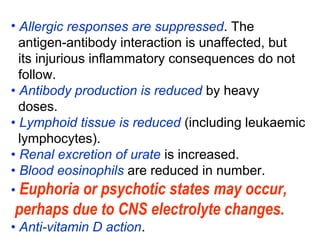
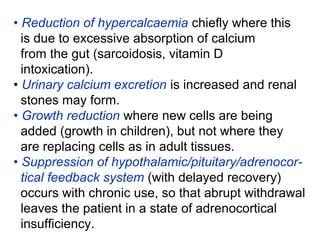
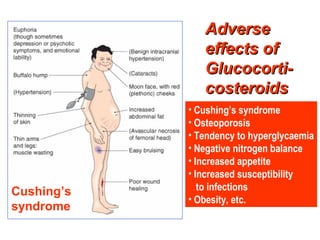
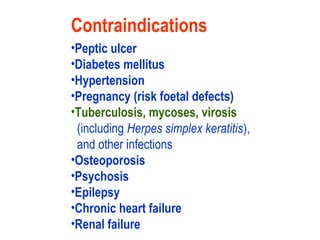
3. Long term glucocorticoid use can cause side effects like Cushing's syndrome, osteoporosis, infections, and obesity. Their use requires monitoring adverse effects.