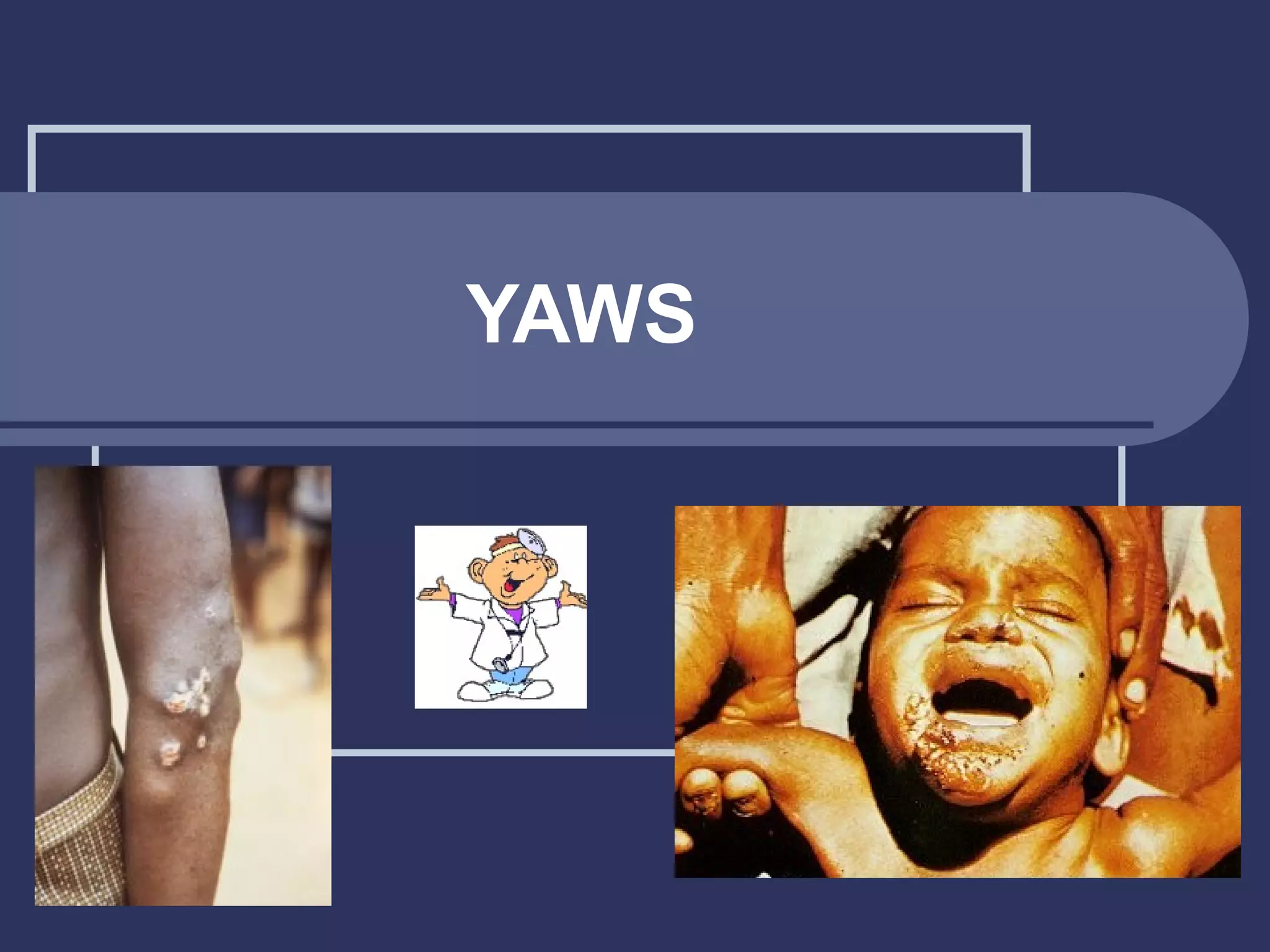
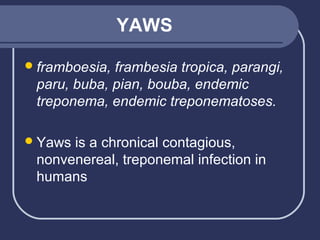
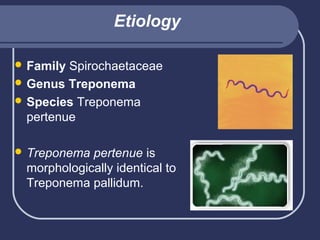
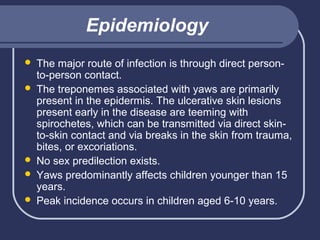
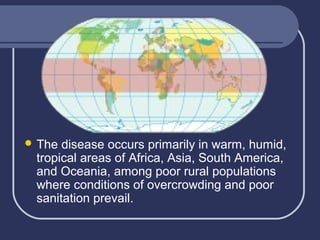
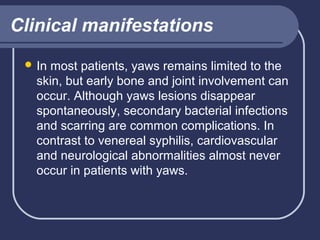
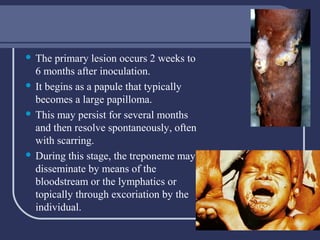
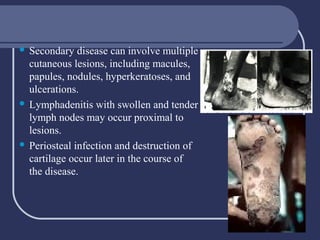
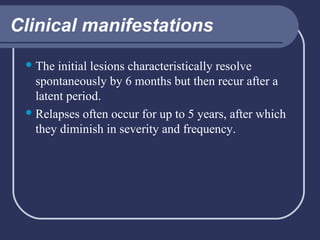
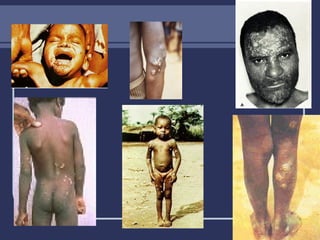
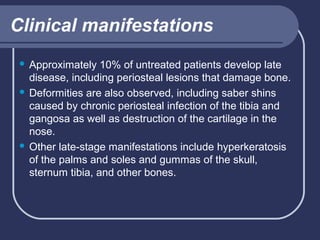
Yaws is a chronic, nonvenereal infection caused by the Treponema pertenue bacteria that is transmitted through direct skin-to-skin contact. It commonly affects children in tropical areas where sanitation is poor. Early symptoms include skin lesions that can cause long-term damage if left untreated. Laboratory tests confirm the presence of the bacteria, while treatment involves antibiotics like penicillin. Prevention relies on improving living conditions and interrupting transmission between individuals.


![Laboratory diagnostic
Nontreponemal
test (eg, rapid plasma reagent
[RPR], VDRL) results are positive in all stages,
except very early lesions.
Confirmatory treponemal tests (eg,
Treponema pallidum hemagglutination
[TPHA], microhemagglutination Treponema
pallidum [MHA-TP], fluorescent treponema
antibody absorption [FTA-ABS]) are not
practical in remote areas.](https://image.slidesharecdn.com/yaws-131205032601-phpapp01/85/Yaws-17-320.jpg)