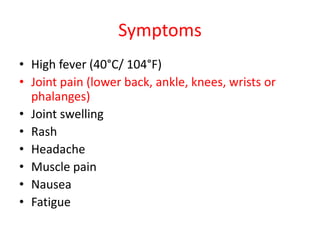
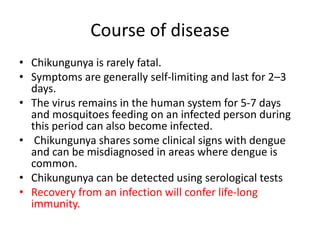
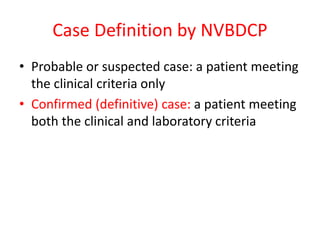
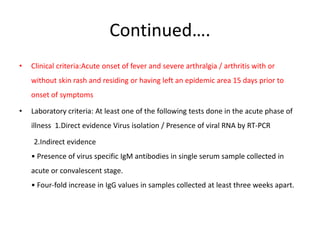
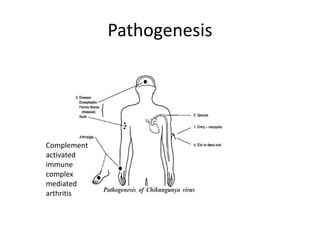
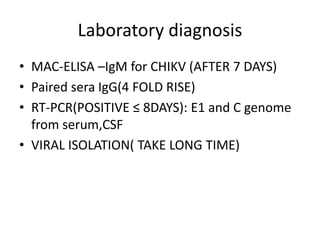
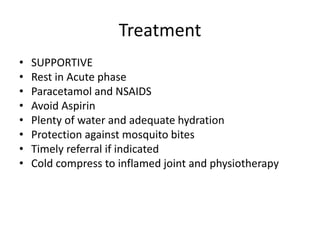
Chikungunya is an arboviral disease transmitted by Aedes mosquitoes that causes fever and severe joint pain. It was first identified in Tanzania in 1952 and has since caused outbreaks in Asia and Africa. India saw a major outbreak in 2006 with over 1.5 million cases reported. Clinical symptoms include high fever, joint pain and swelling, rash, and fatigue. While rarely fatal, the joint pain can last for months in some cases. Diagnosis is confirmed through serological tests showing IgM or IgG antibodies. There is no vaccine or antiviral treatment, so care is supportive with rest, hydration, and pain medication. Prevention relies on controlling mosquito populations and avoiding bites.