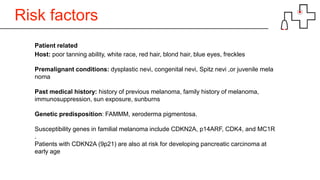
Melanoma is the most lethal form of skin cancer. While it only accounts for about 3% of skin cancer cases, it causes around 75% of skin cancer deaths. The rate of melanoma is increasing in older age groups. Risk factors include poor tanning ability, red or blond hair, family history, and sun exposure. Melanoma can spread locally, to lymph nodes, or distantly to organs. Staging involves tumor thickness and presence of metastases. Treatment involves surgery to remove the primary tumor and lymph nodes, with the addition of radiation therapy or immunotherapy for higher-risk cases. Advanced or metastatic melanoma may be treated with targeted therapies, immunotherapy, chemotherapy, or palliative radiation.

![Epidemiology
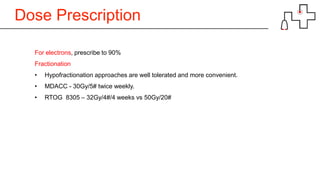
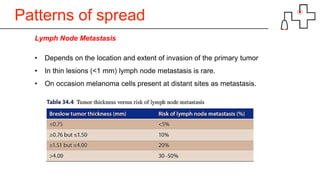
• Among the common skin cancers, melanoma is the most lethal.
• only 3% of all skin cancers diagnosed each year
• 75% of all skin cancer-related deaths. [1]
• Incidence and mortality are decreasing in the younger population,
• Increasing in the older age groups. [2]
1.Chang DT, Amdur RJ, Morris CG, Mendenhall WM. Adjuvant radi therapy for cutaneous melanoma: comparing hypofractionation to onventional fractionation. Int J Radiat Oncol Biol Phys 2006;66:1 5
1-5. [PUBMED] [FULLTEXT]
2.French J, McGahan C, Duncan G, Lengoc S, Soo J, Cannon J. How gender, age, and geography influence the utilization of radiation therapy in the management of malignant melanoma. Int J Radiat
Oncol Biol Phys 2006;66:1056-63.
[PUBMED] [FULLTEXT]
3.Mowbray M, Stockton DL, Doherty VR. Changes in the site distribution of malignant melanoma in south-east Scotland (1979-2002). Br J Cancer 2007;96:832-5. [PUBMED] [FULLTEXT]](https://image.slidesharecdn.com/melanoma-181003152548/85/Melanoma-2-320.jpg)
![Epidemiology
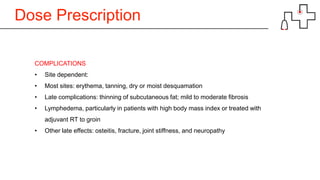
The rate of increasing incidence varies
geographically
• “High incidence regions" like Australia,
• “Moderate incidence regions" like
Canada and USA, and
• “Low incidence regions" like Scotland
and India. [3]
HIGH
LOW
LOWMODERATE](https://image.slidesharecdn.com/melanoma-181003152548/85/Melanoma-3-320.jpg)
![Treatment Surgery
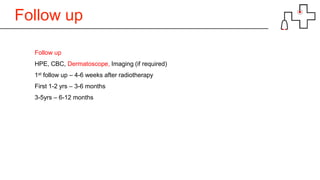
cN0: WLE and SLN biopsy, with completion LND if SLN+.
Spares patients from the complications associated with elective lymphadenectomy
SLNB improves staging to identify patients who may need completion node dissection
and/or adjuvant therapy
The false-negative rate of SLNB is <5%
Clinically N+: WLE and nodal dissection
Patients with positive SLNB and immediate lymphadenectomy had a superior
overall survival advantage as compared with patients with lymphadenectomy
at the time of clinically evident nodal diseases[1].
1. Morton DL, Thompson JF, Cochran AJ et al (2006) Sentinel-node biopsy or nodal observation in melanoma. N Engl J Med. 355:1307–1317.](https://image.slidesharecdn.com/melanoma-181003152548/85/Melanoma-23-320.jpg)
![Treatment Systemic therapy
For node-negative IA - IIA: observation or clinical trial
For node-negative IIB–IIC: observation vs clinical trial vs high-dose IFN
For node positive: observation, clinical trial, interferon alfa, ipilimumab, or other bioche
motherapy agents
A Meta-analysis shows a statistically significant improvement in overall and disease-
free survival in patients with high risk cutaneous melanoma treated with IFN-α [1]
1. Mocellin S, Pasquali S, Rossi C et al (2010) Interferon alpha adjuvant therapy in patients with high-risk melanoma: a sy
stematic review and meta-analysis; J. Natl Cancer Inst. 102(7): 493-501; Wheatley K, Ives N, Hancock B et al (20 3) Doe
s adjuvant interferon for high risk melanoma provide a worthwhile benefi t? A meta-analysis of ranomizede trials. Cancer t
reat rev 29: 241-252](https://image.slidesharecdn.com/melanoma-181003152548/85/Melanoma-26-320.jpg)