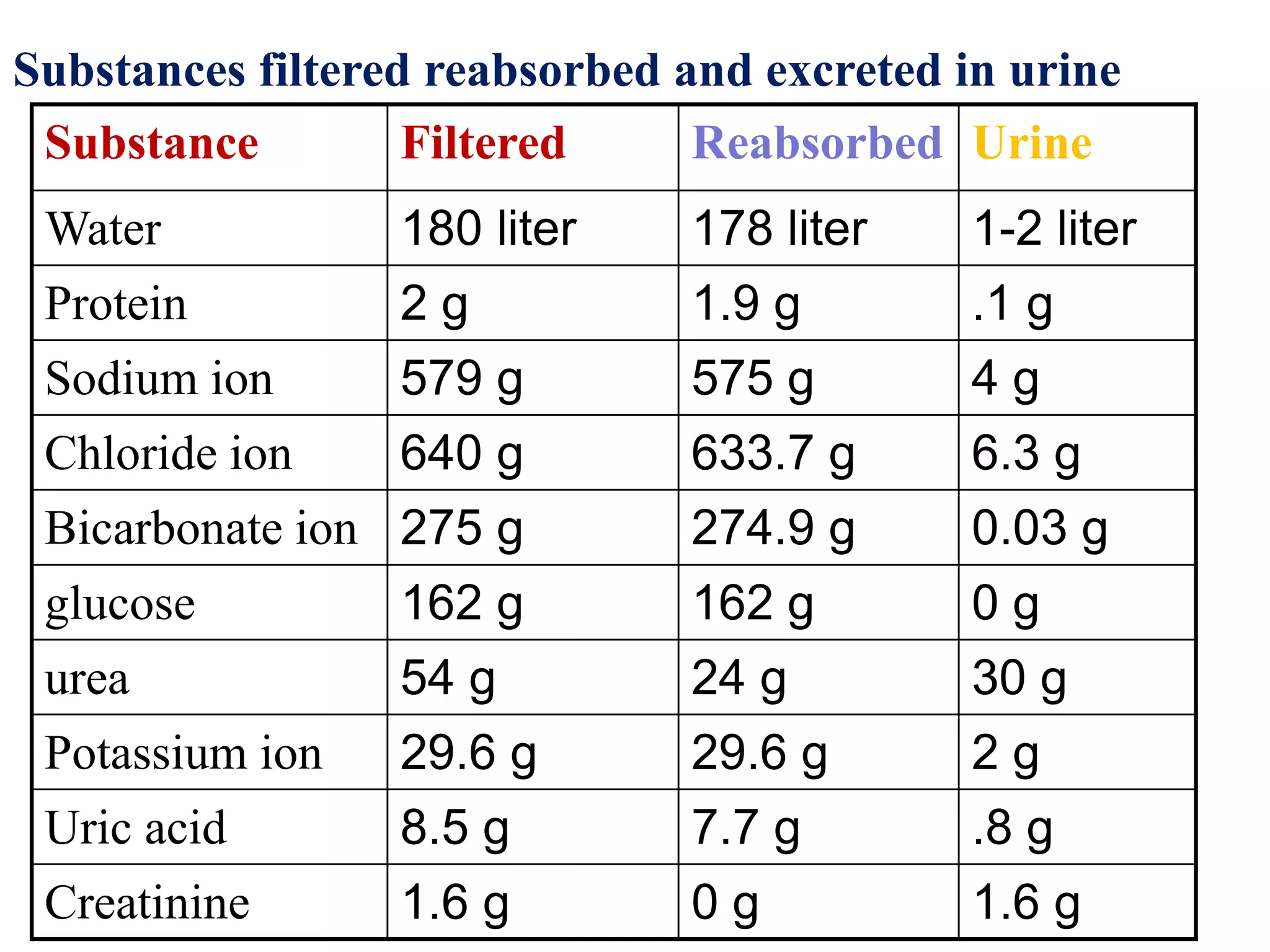
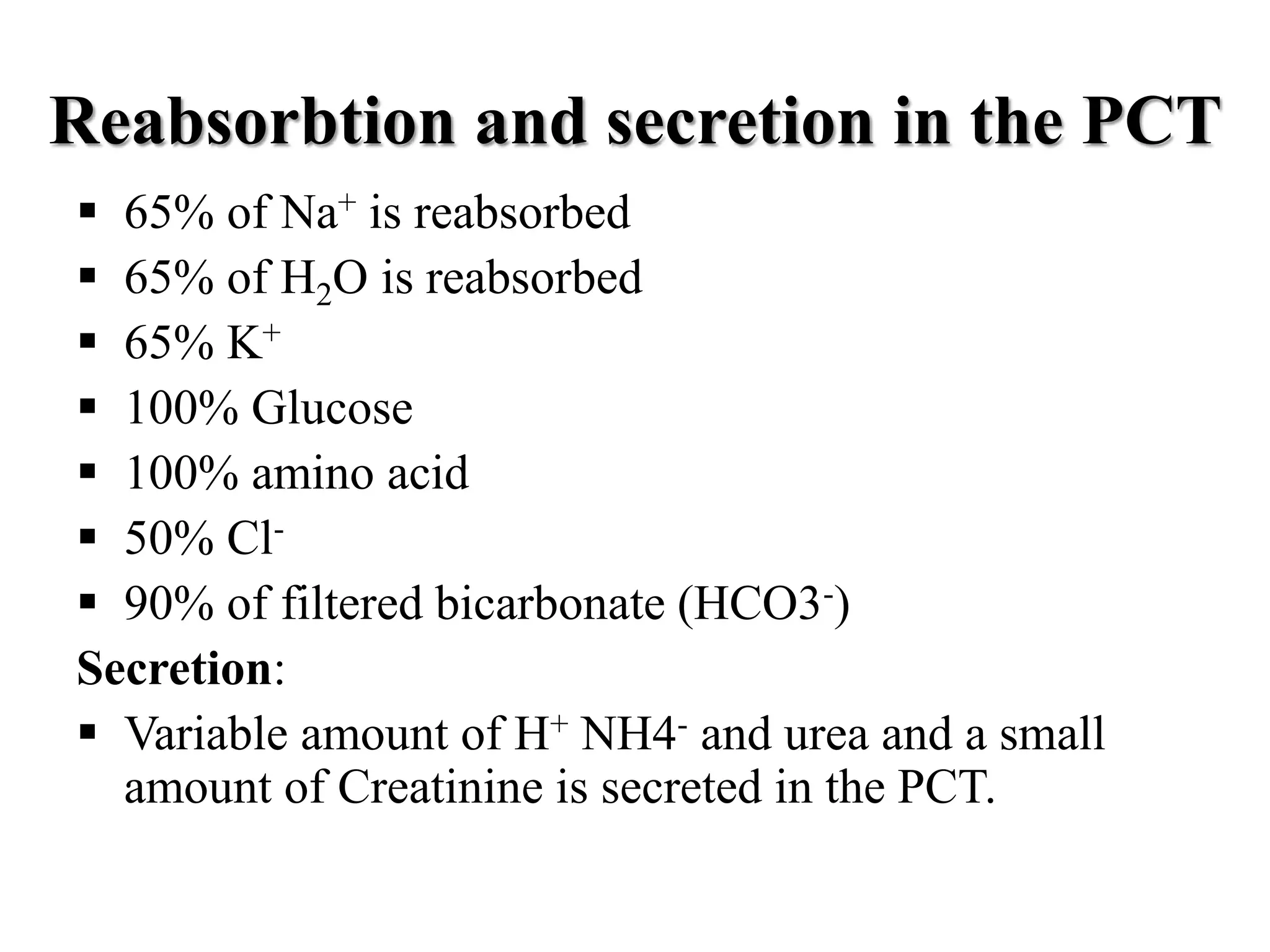
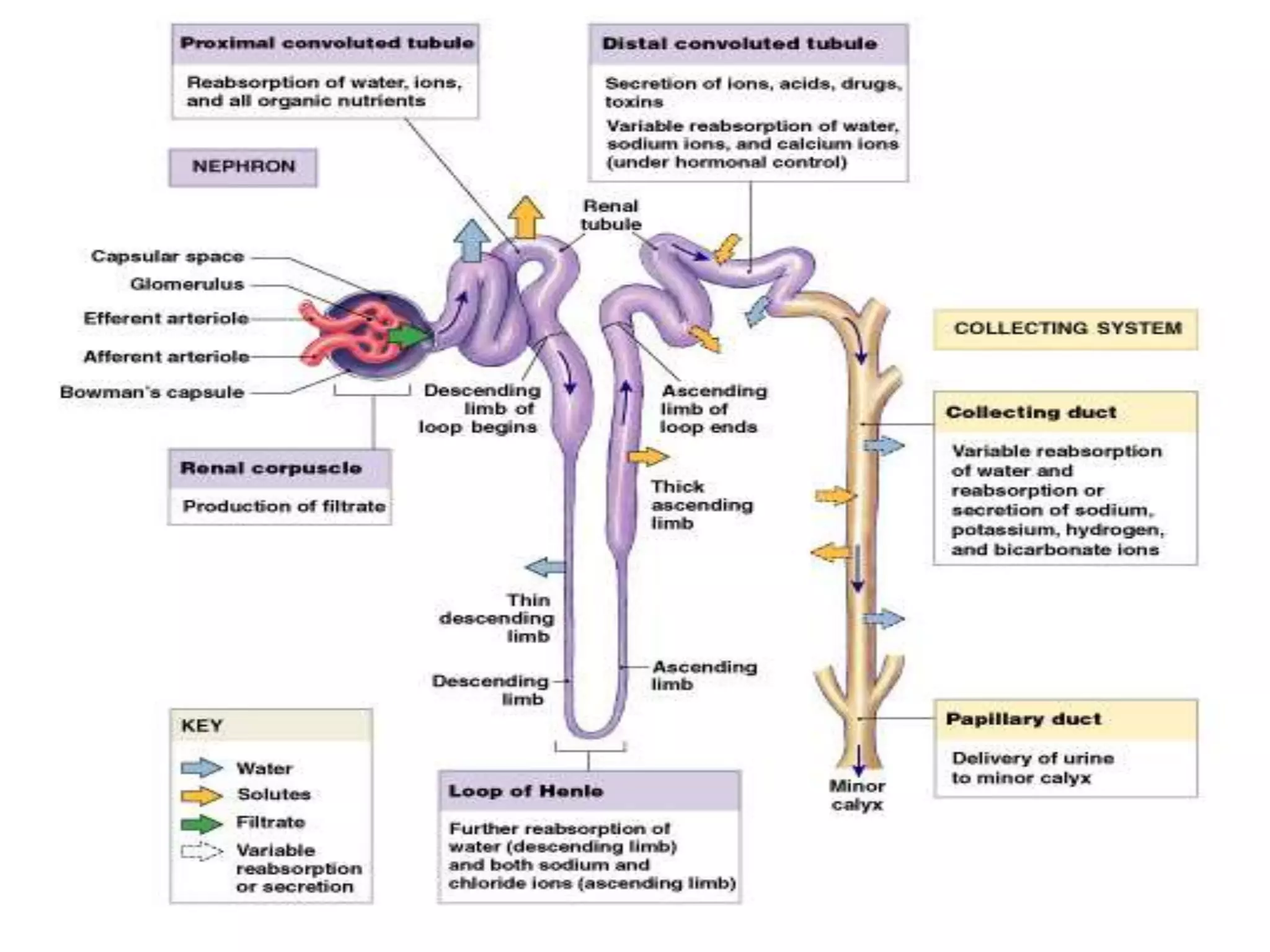
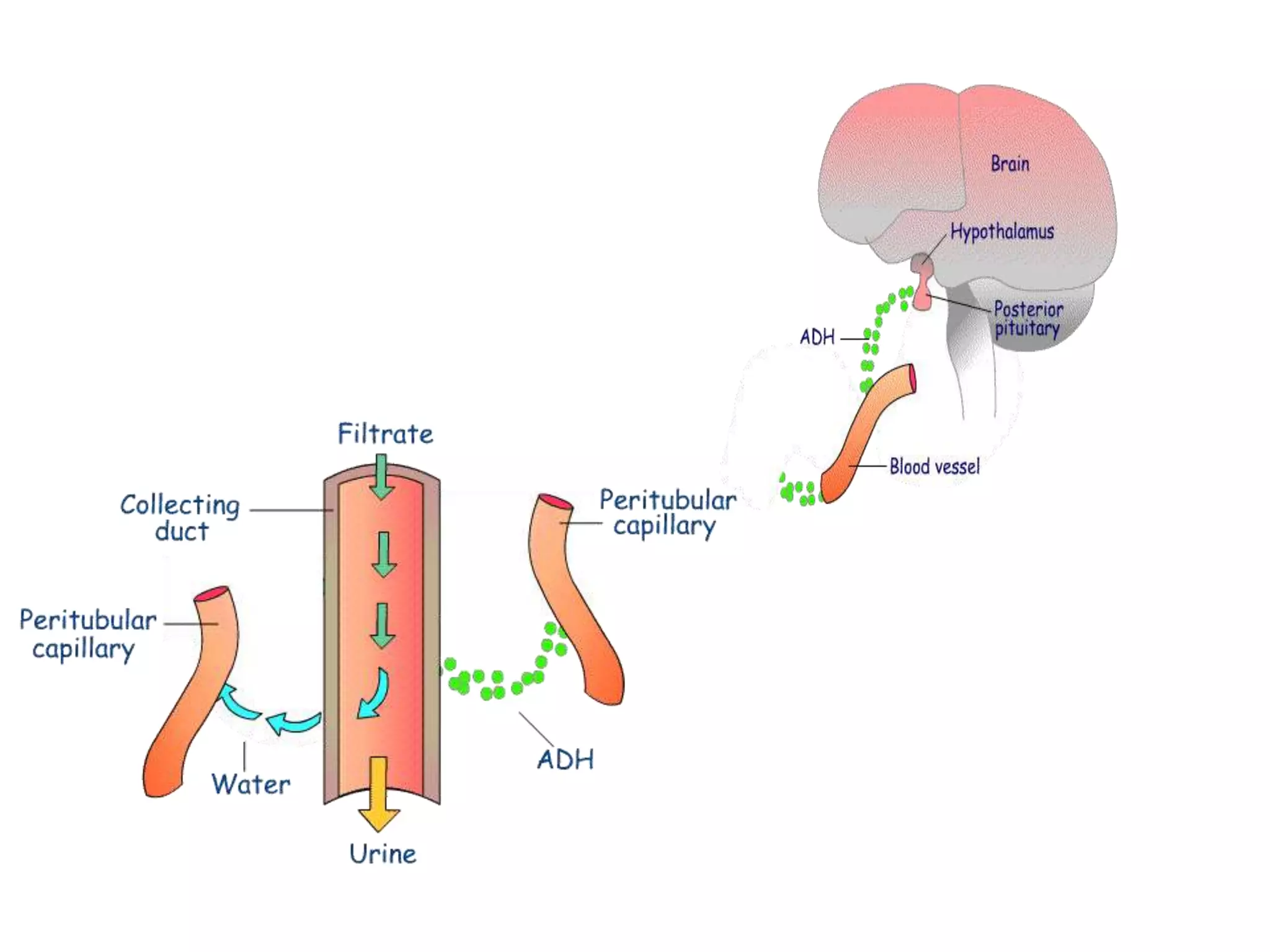
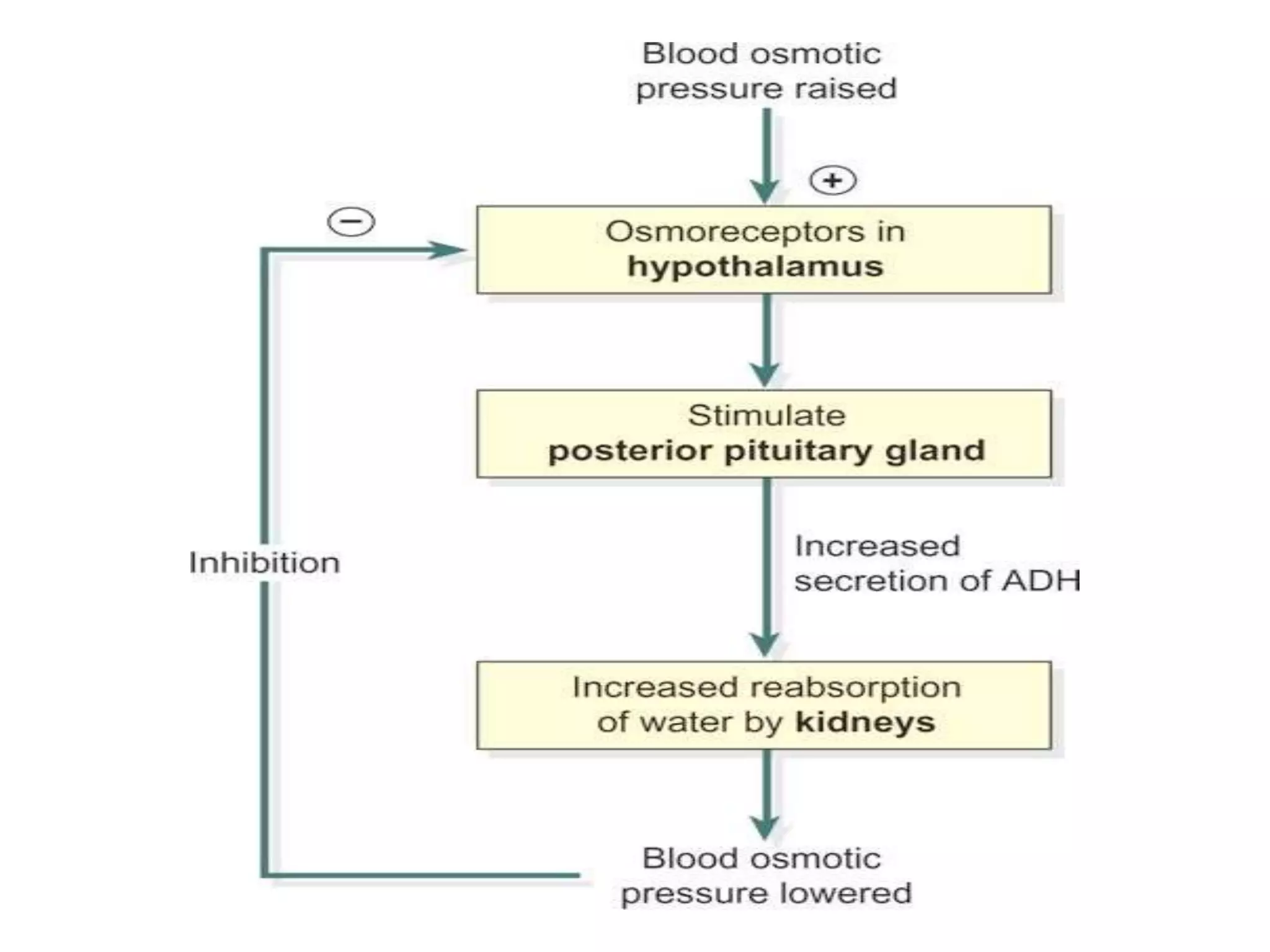
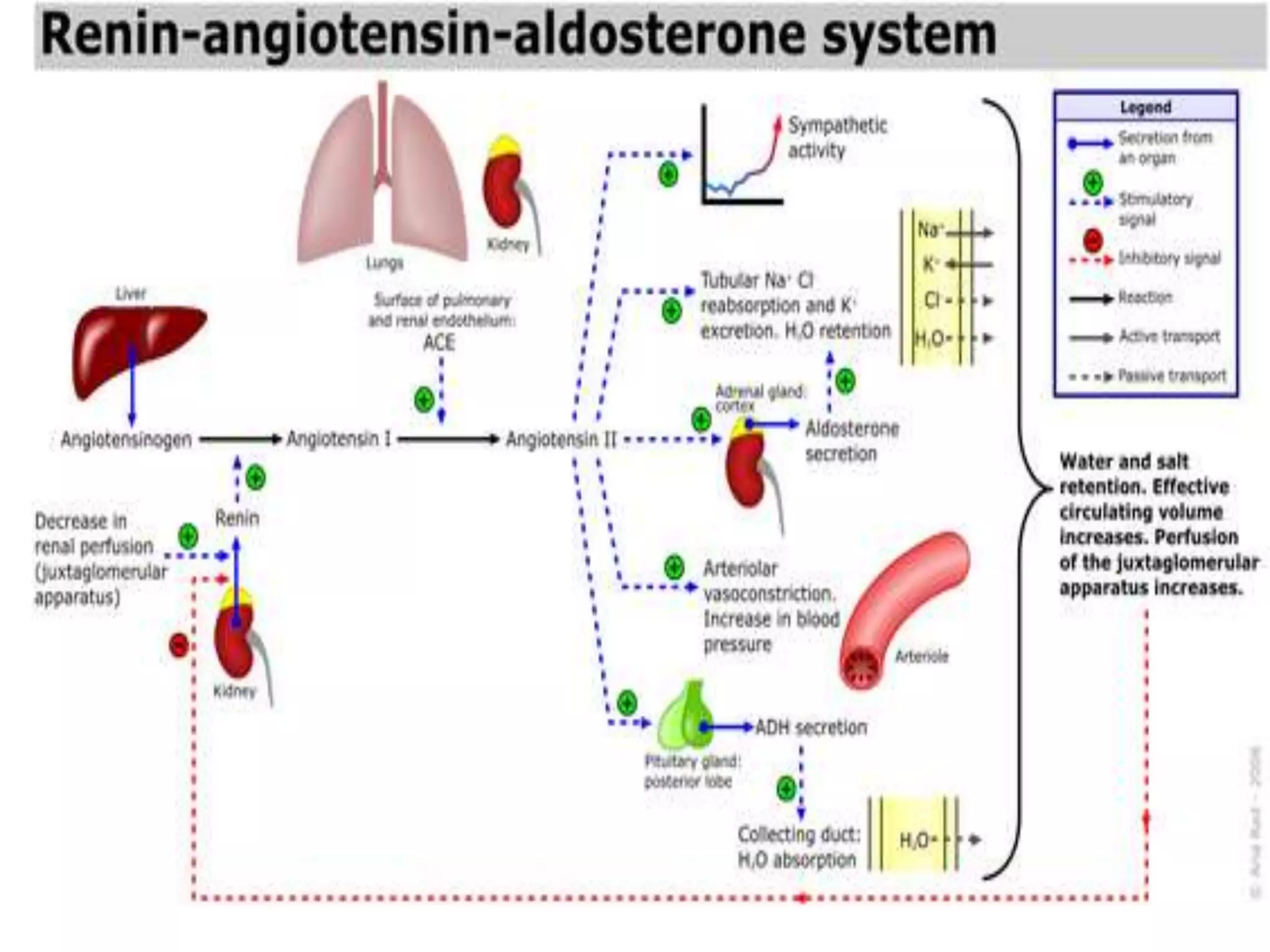
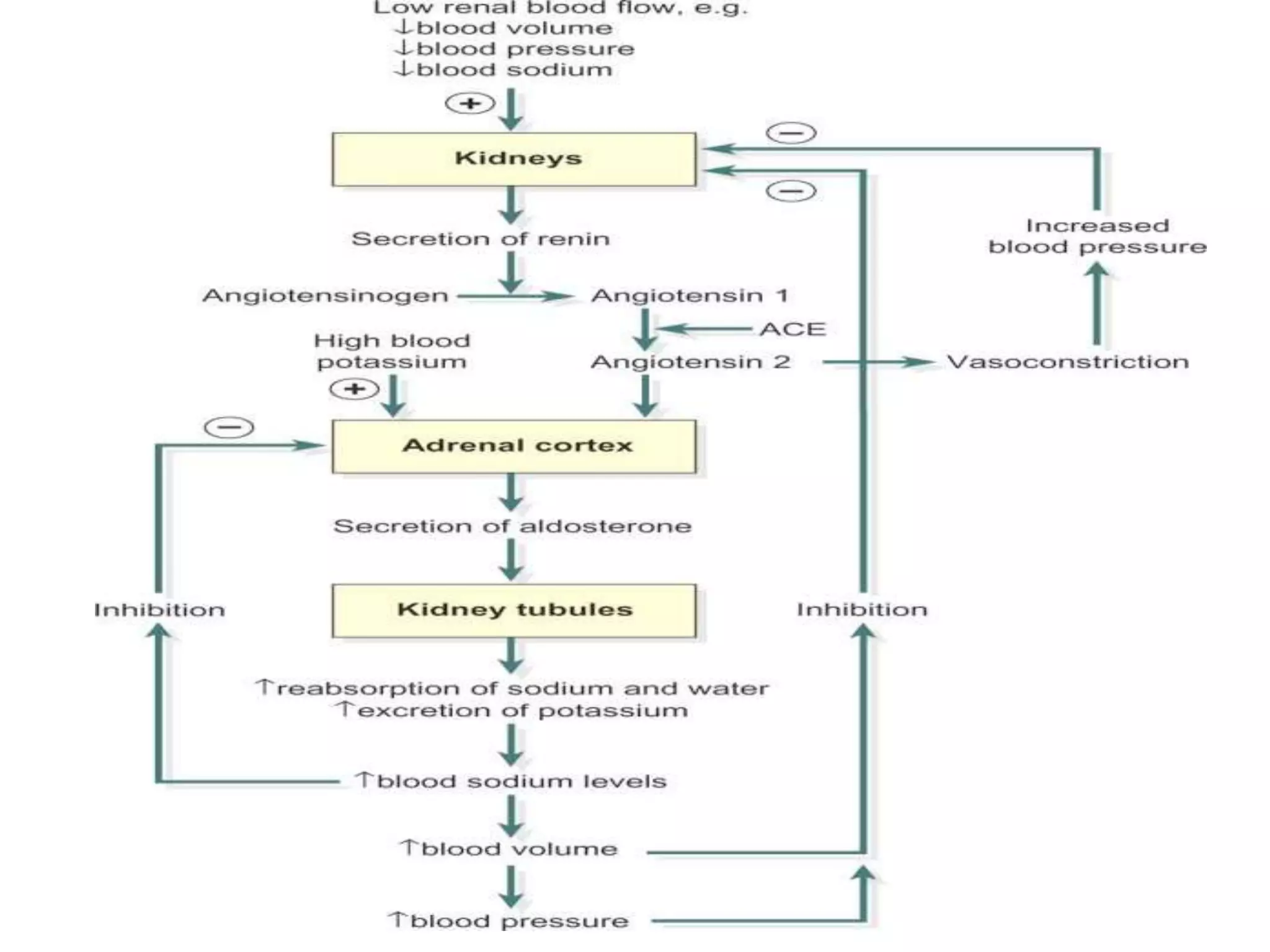
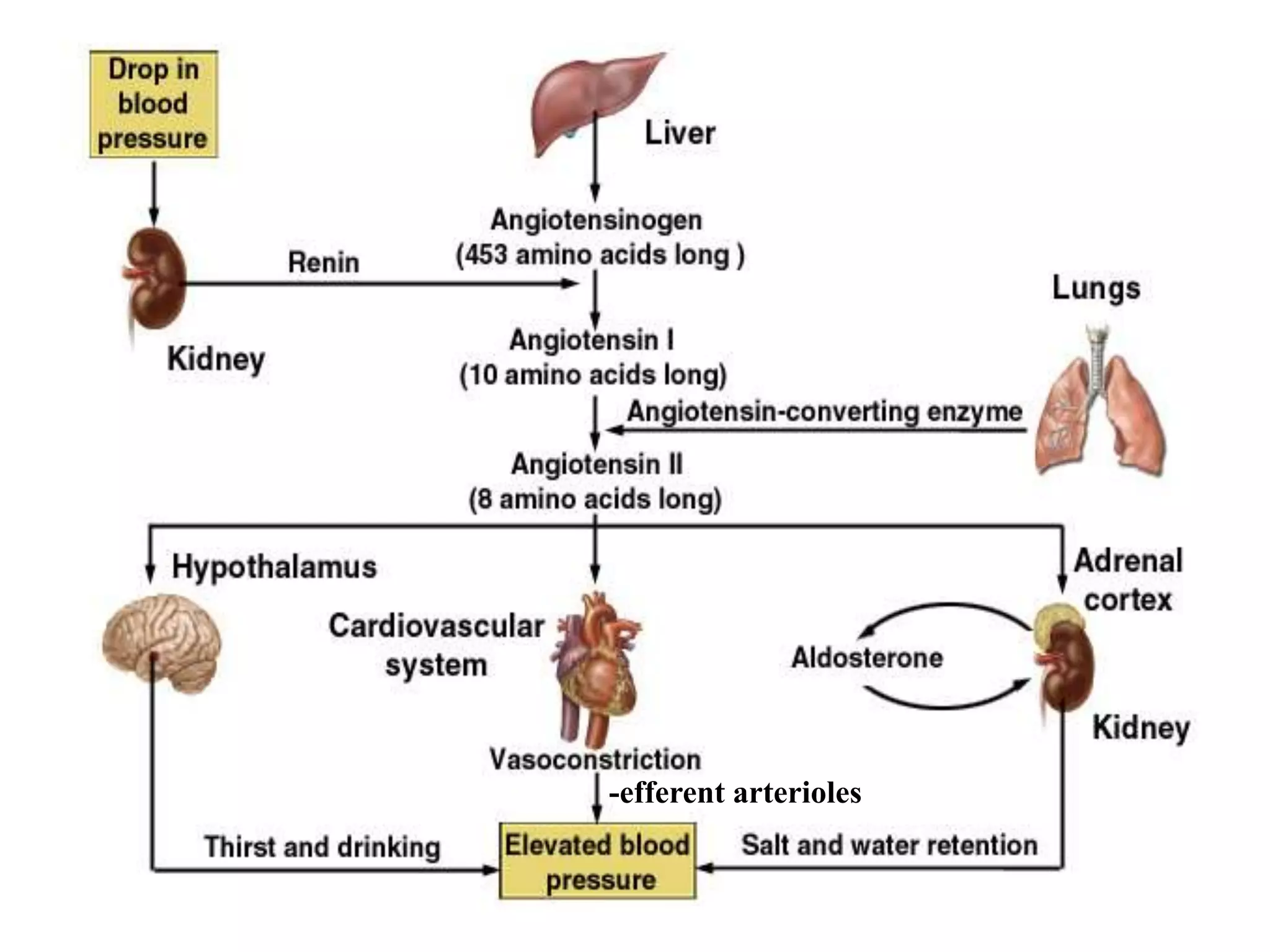
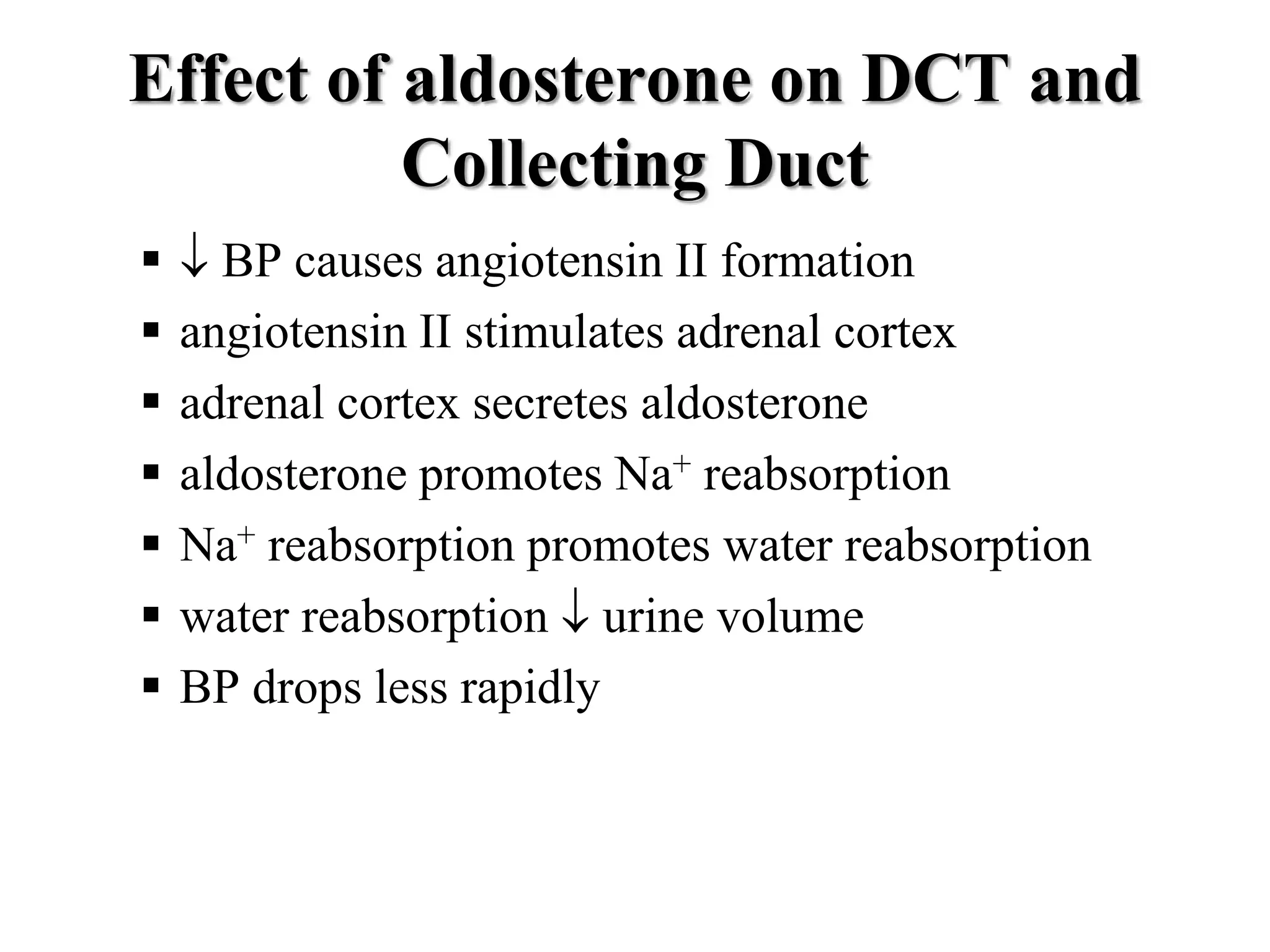
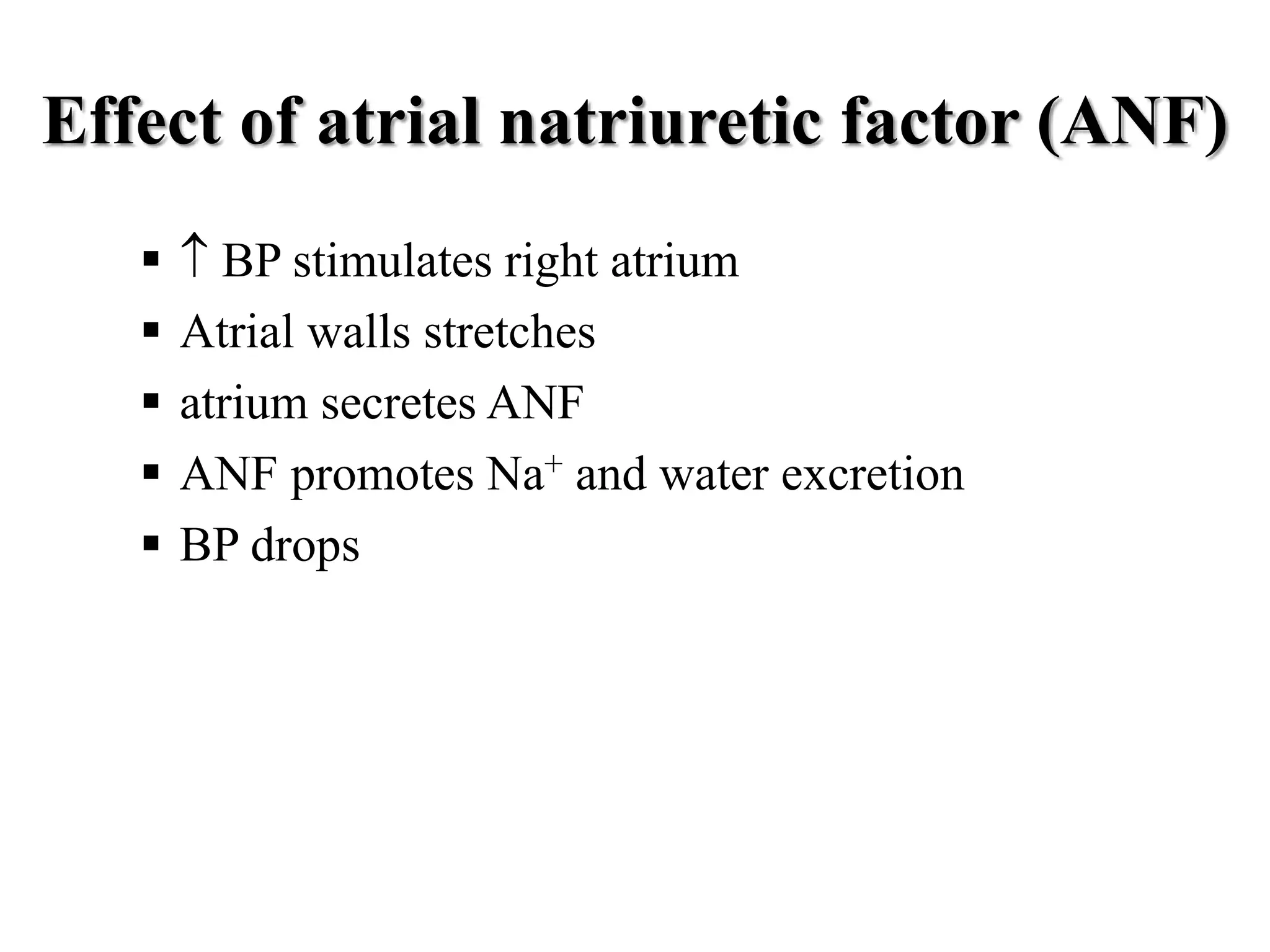
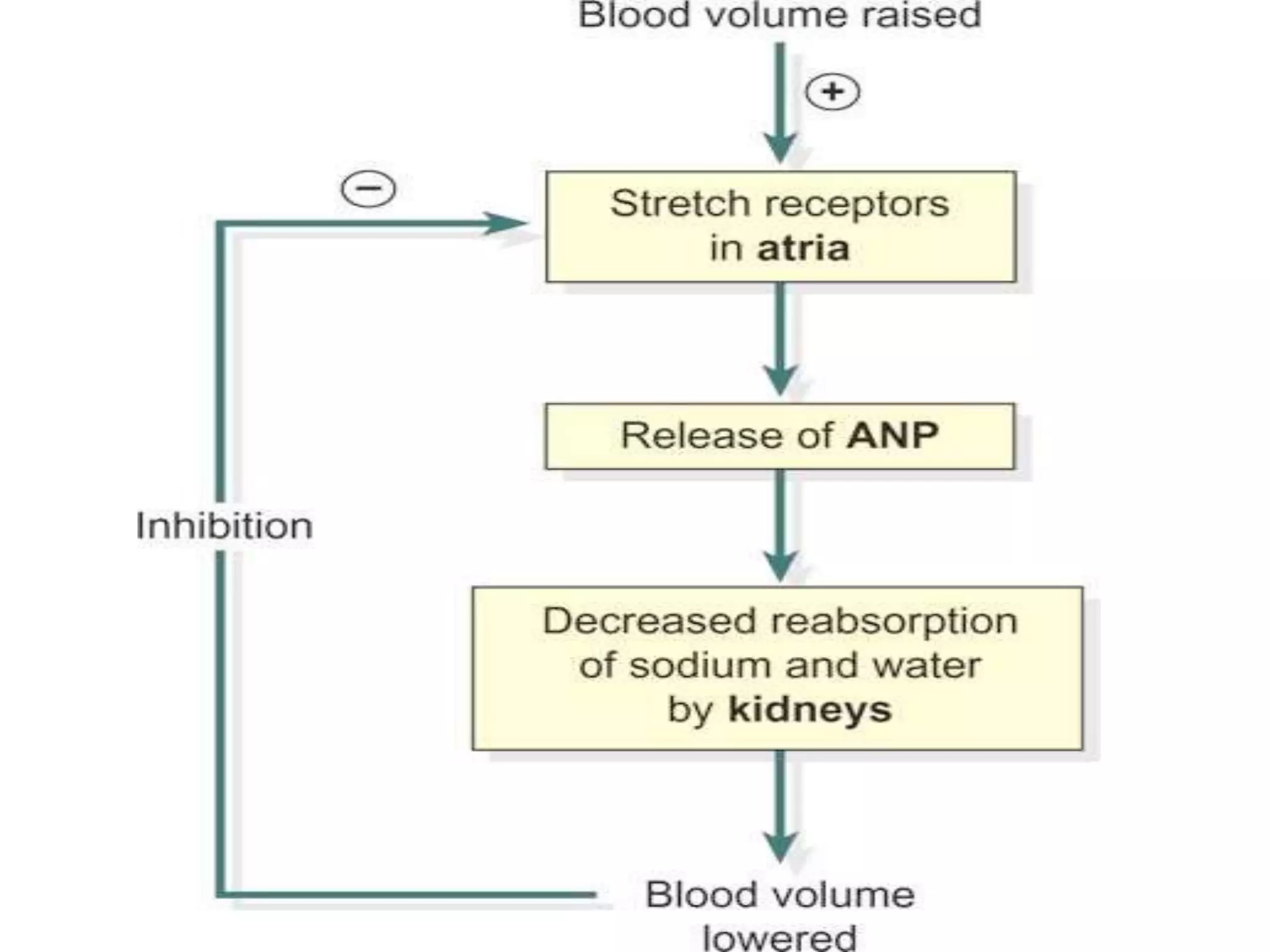
Neural and hormonal factors regulate glomerular filtration rate (GFR). Sympathetic nerves release norepinephrine which causes blood vessel constriction and decreases GFR. The hormones angiotensin II and atrial natriuretic peptide respectively decrease and increase GFR. Tubular reabsorption and secretion are also regulated. Most filtered water, sodium, and other solutes are reabsorbed, while the kidney secretes substances like hydrogen ions, potassium, and drugs. Hormones such as aldosterone and antidiuretic hormone impact reabsorption of water and sodium.