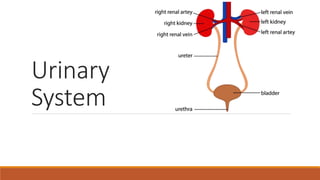
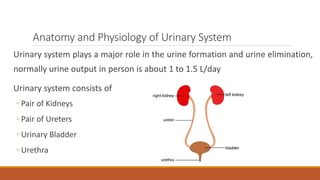
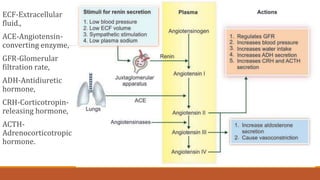
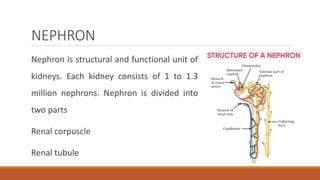
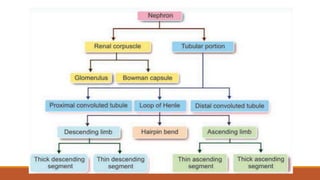
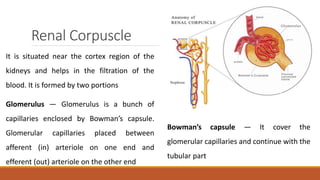
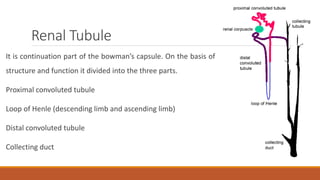
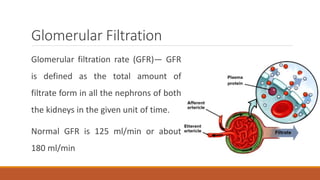
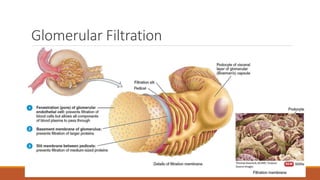
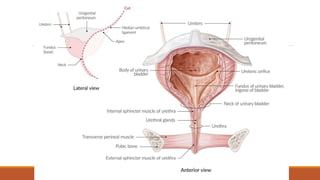
The urinary system works to filter waste from the blood and excrete it as urine. It includes the kidneys, ureters, bladder, and urethra. The kidneys contain millions of nephrons, which are the functional filtering units. Blood is filtered through nephrons, and the resulting glomerular filtrate undergoes reabsorption and secretion processes to form urine, which is stored in the bladder and expelled through the urethra. The urinary system helps regulate water balance, electrolyte levels, acid-base balance, and blood pressure.