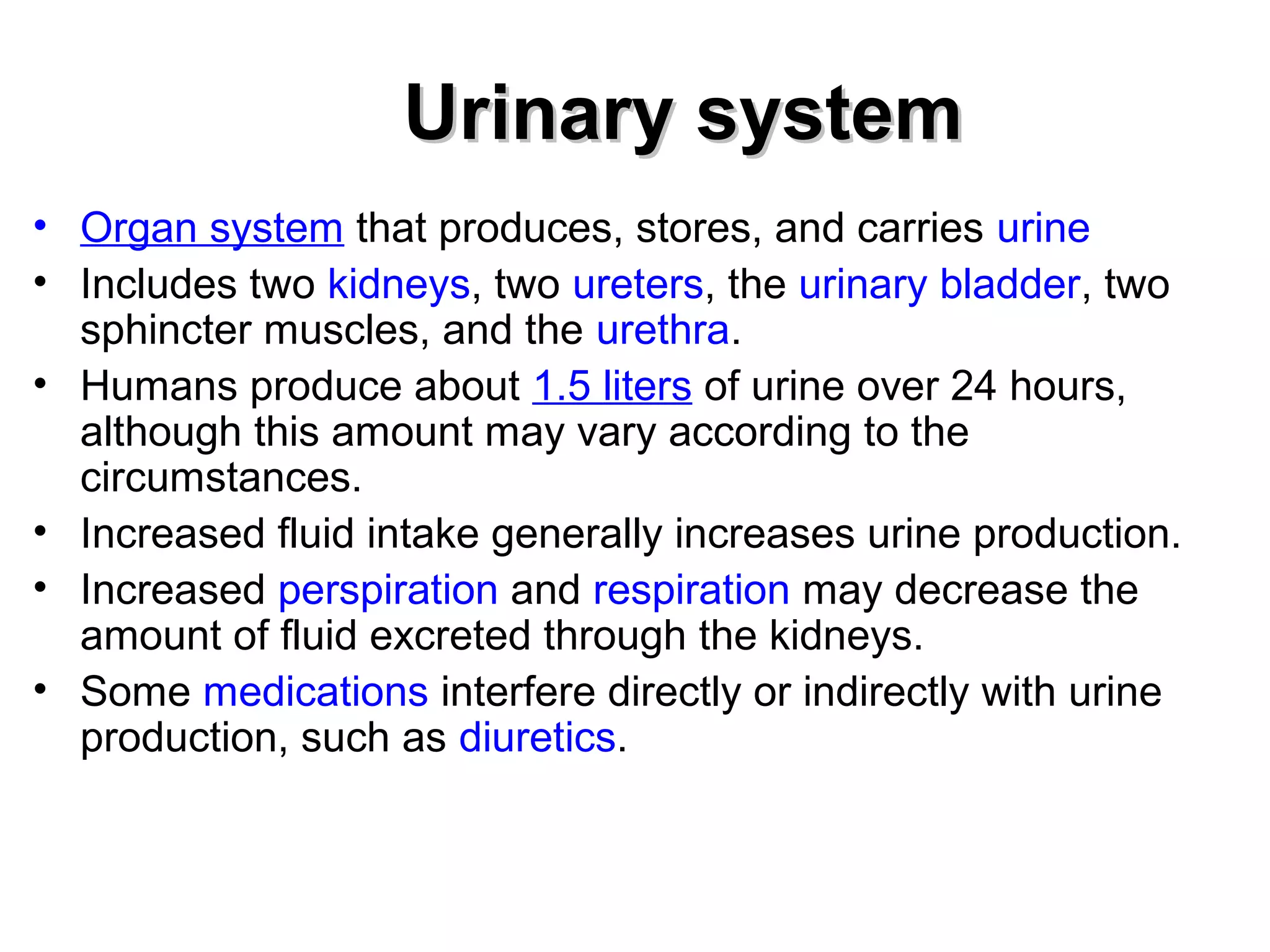
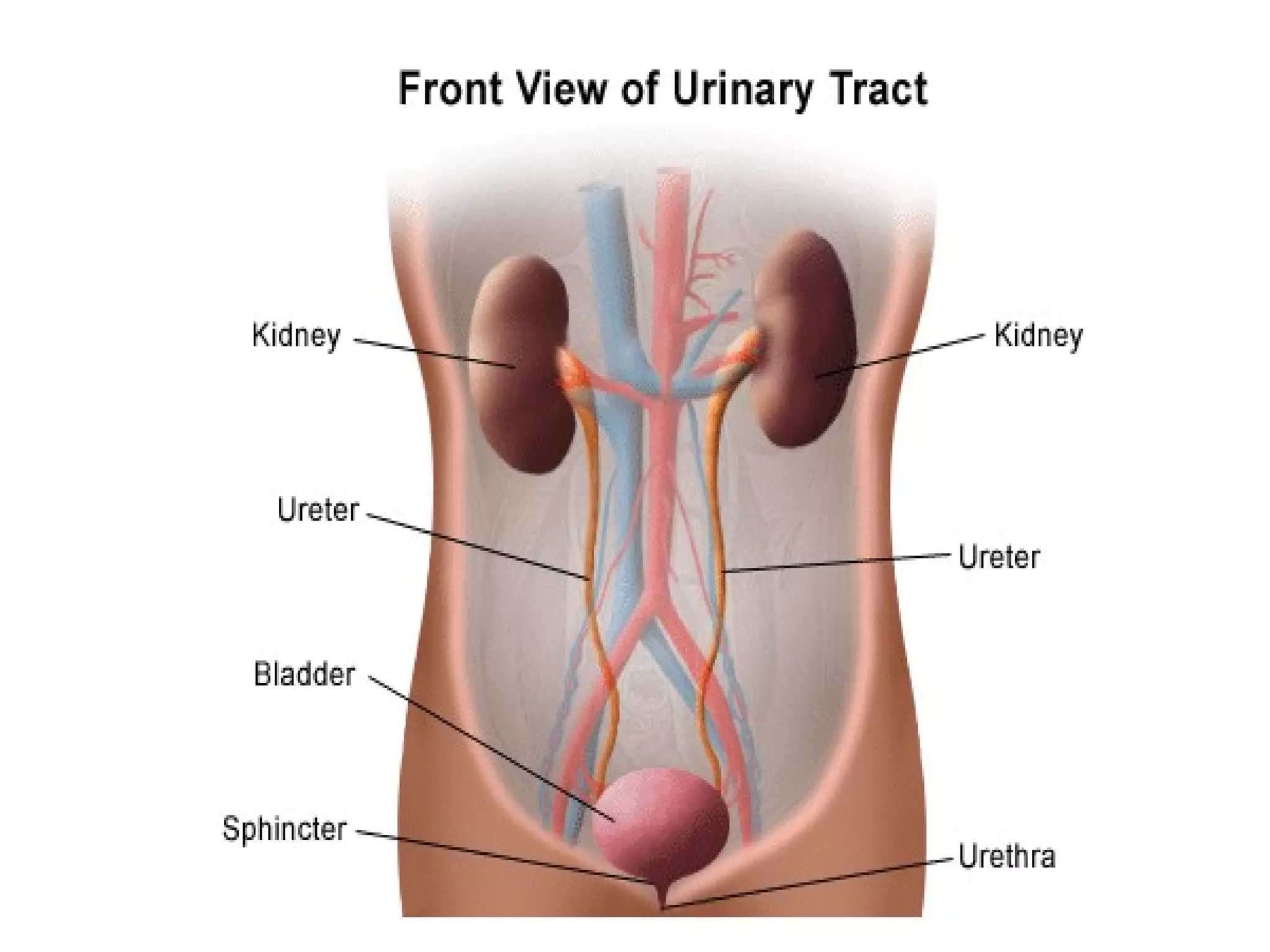
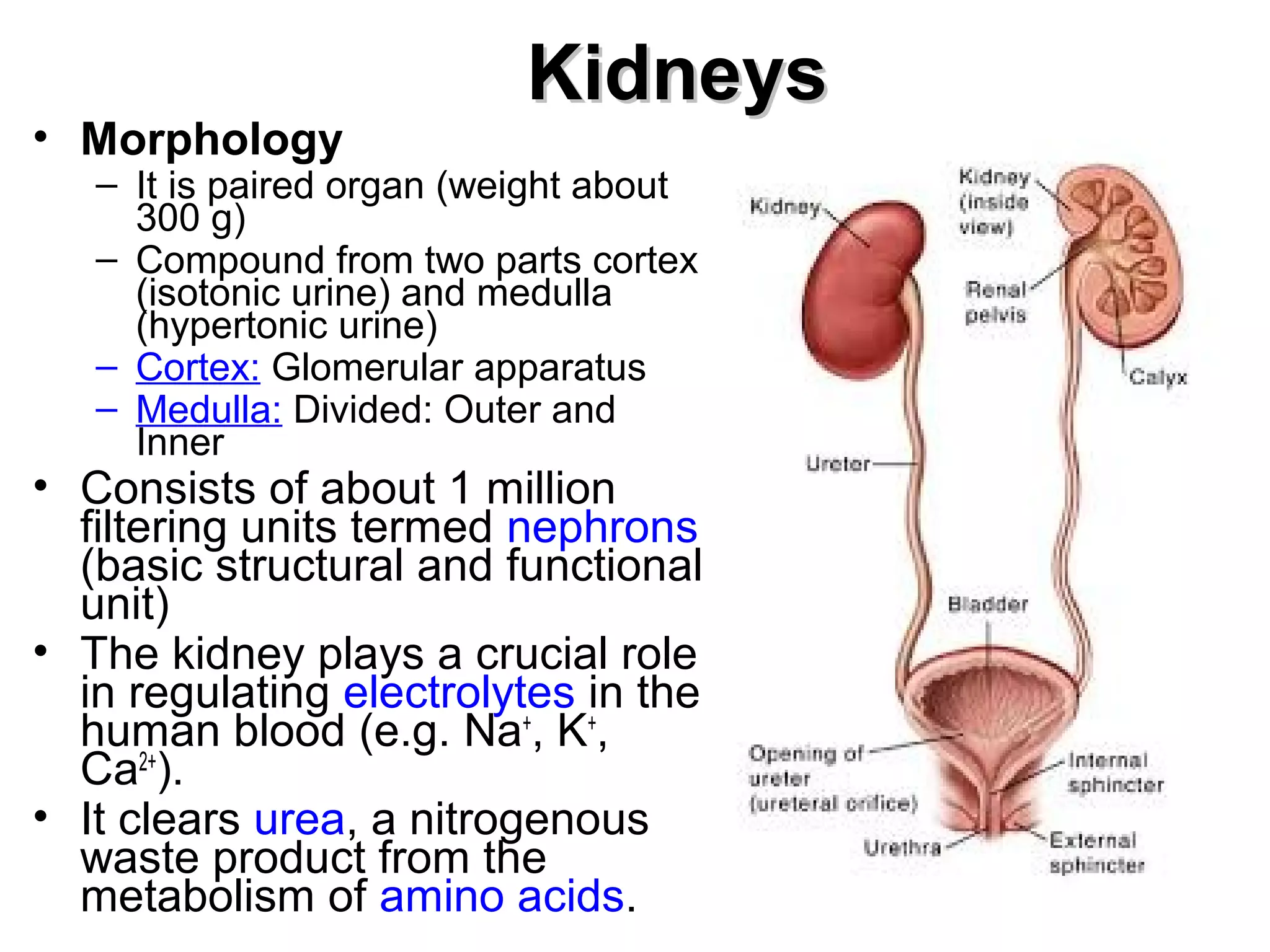
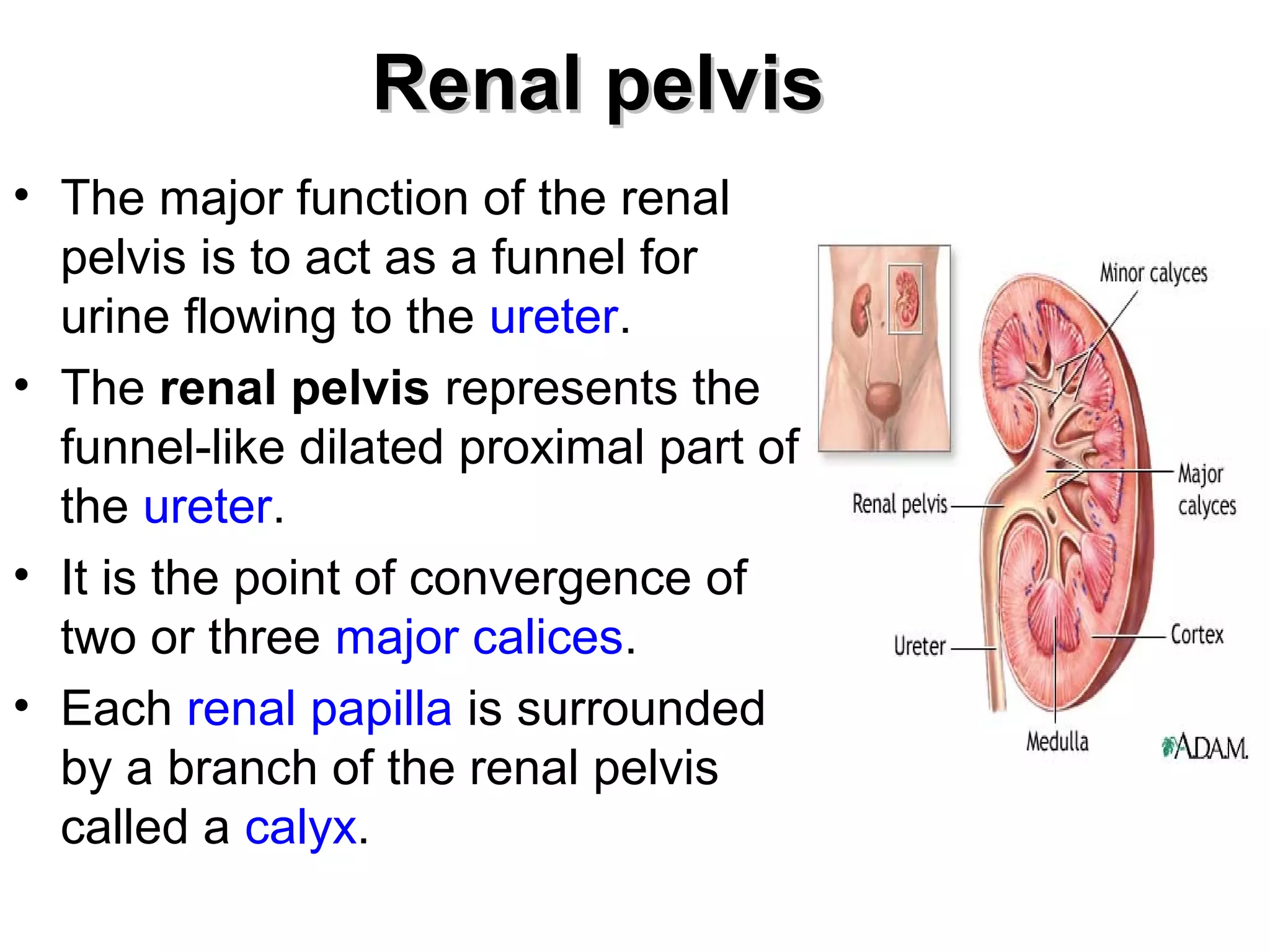
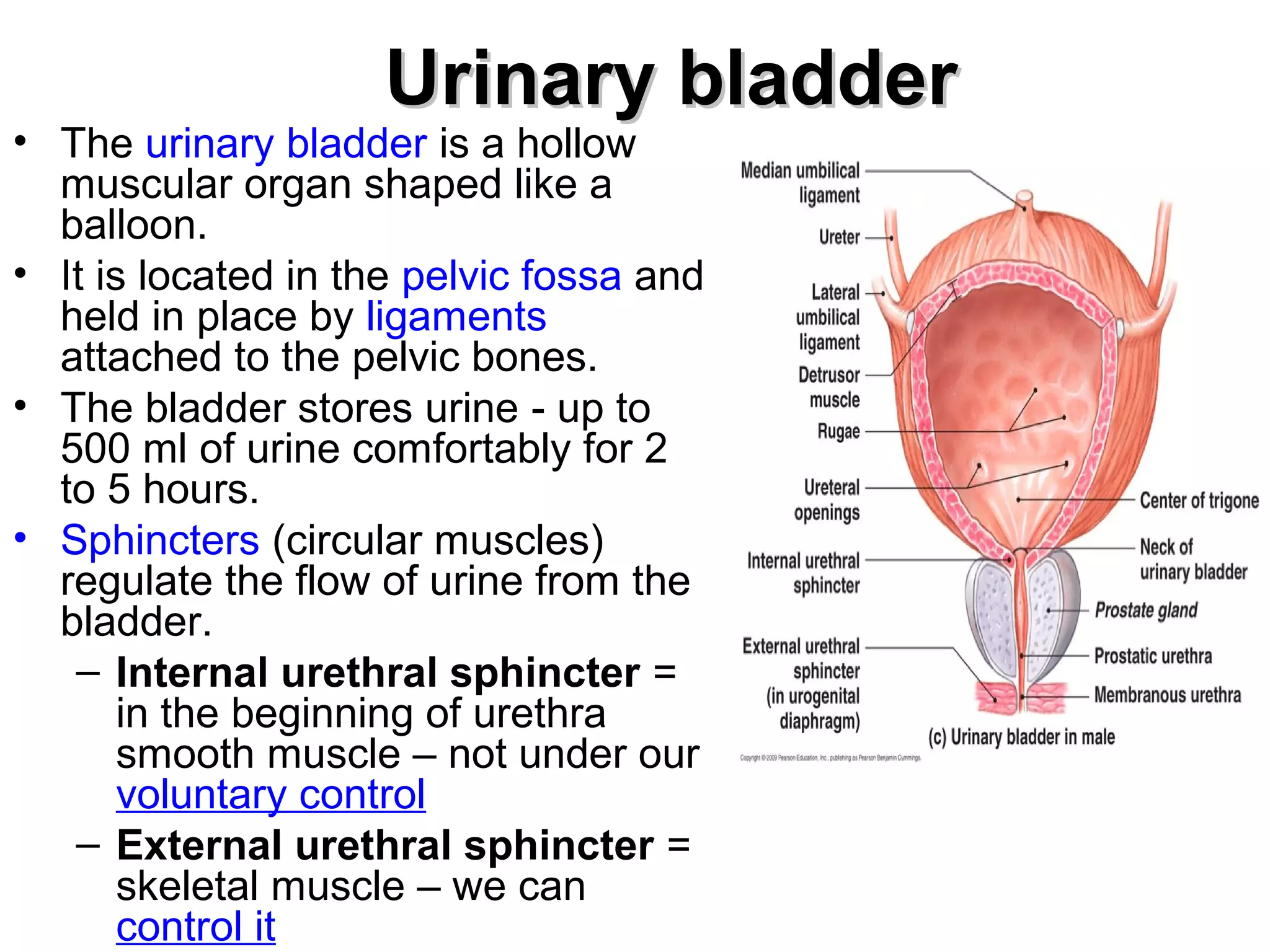
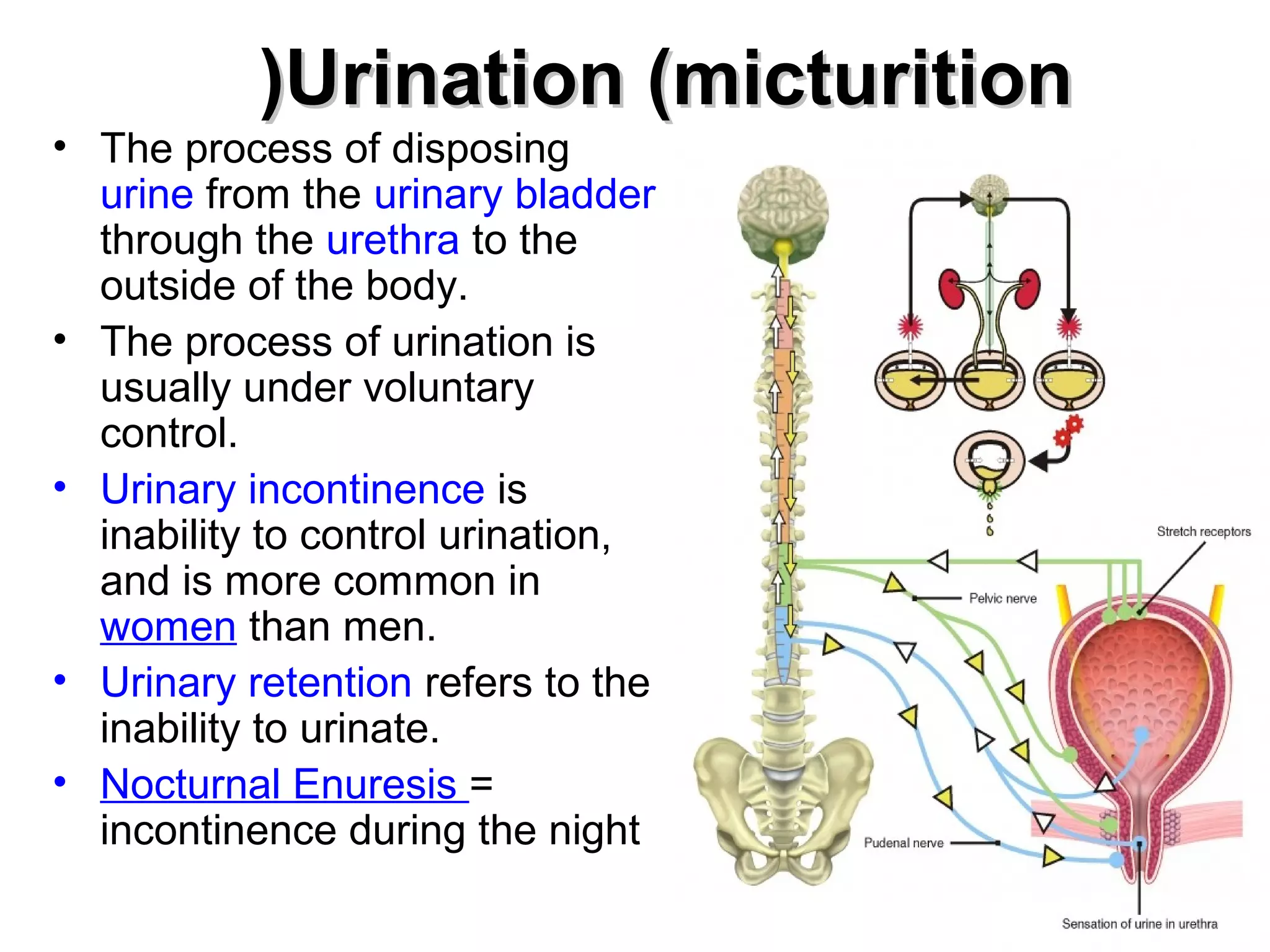
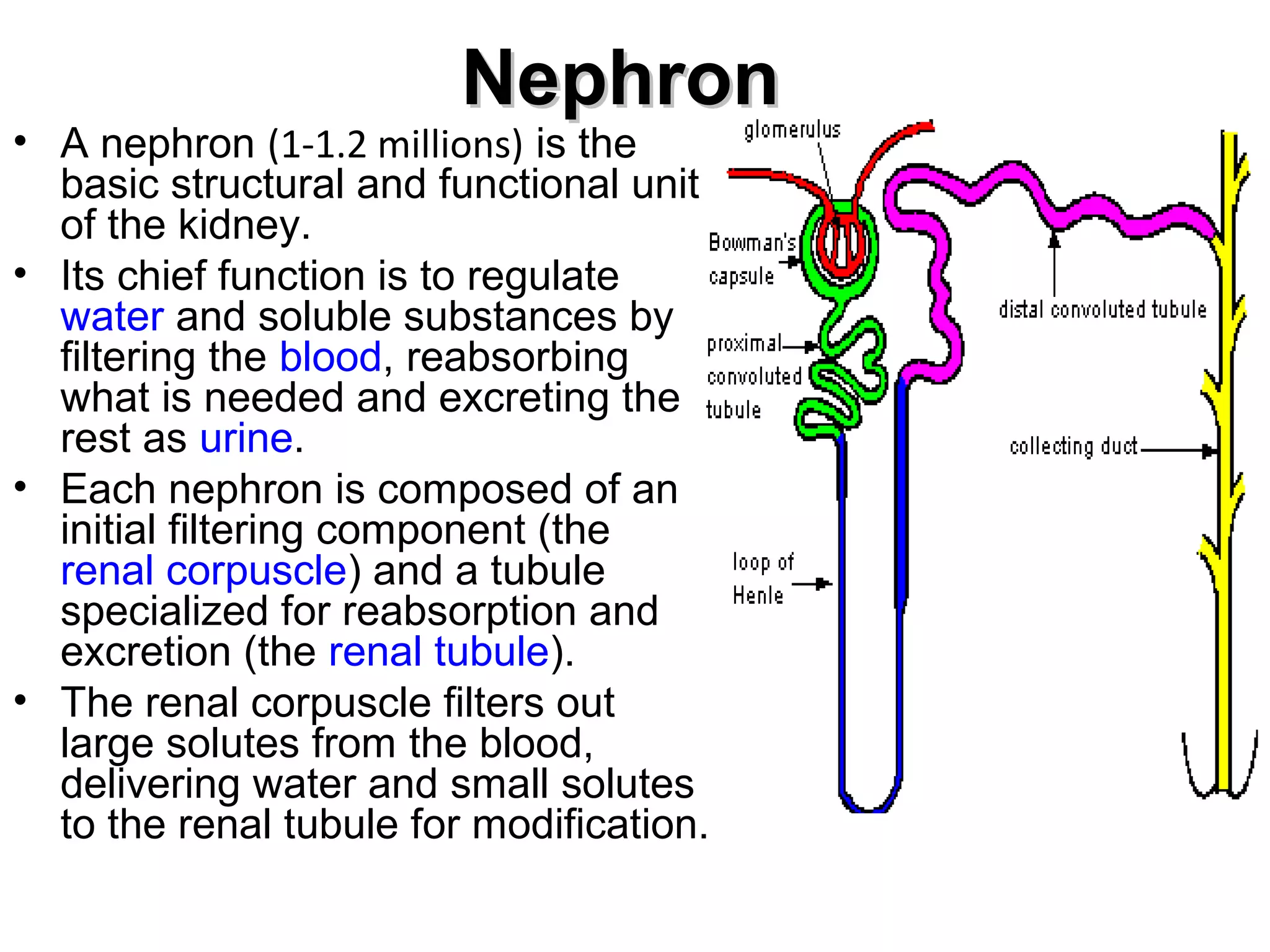
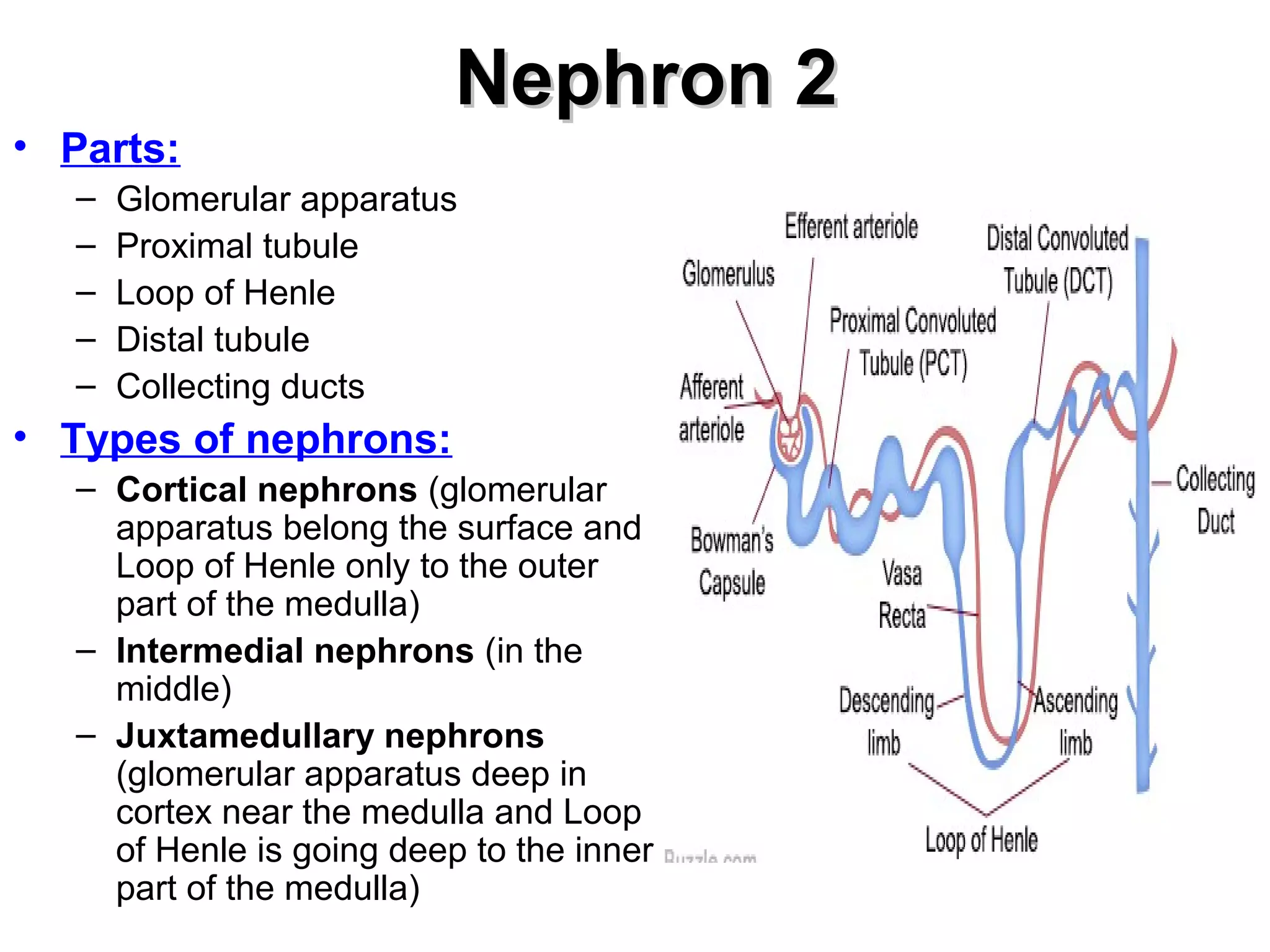
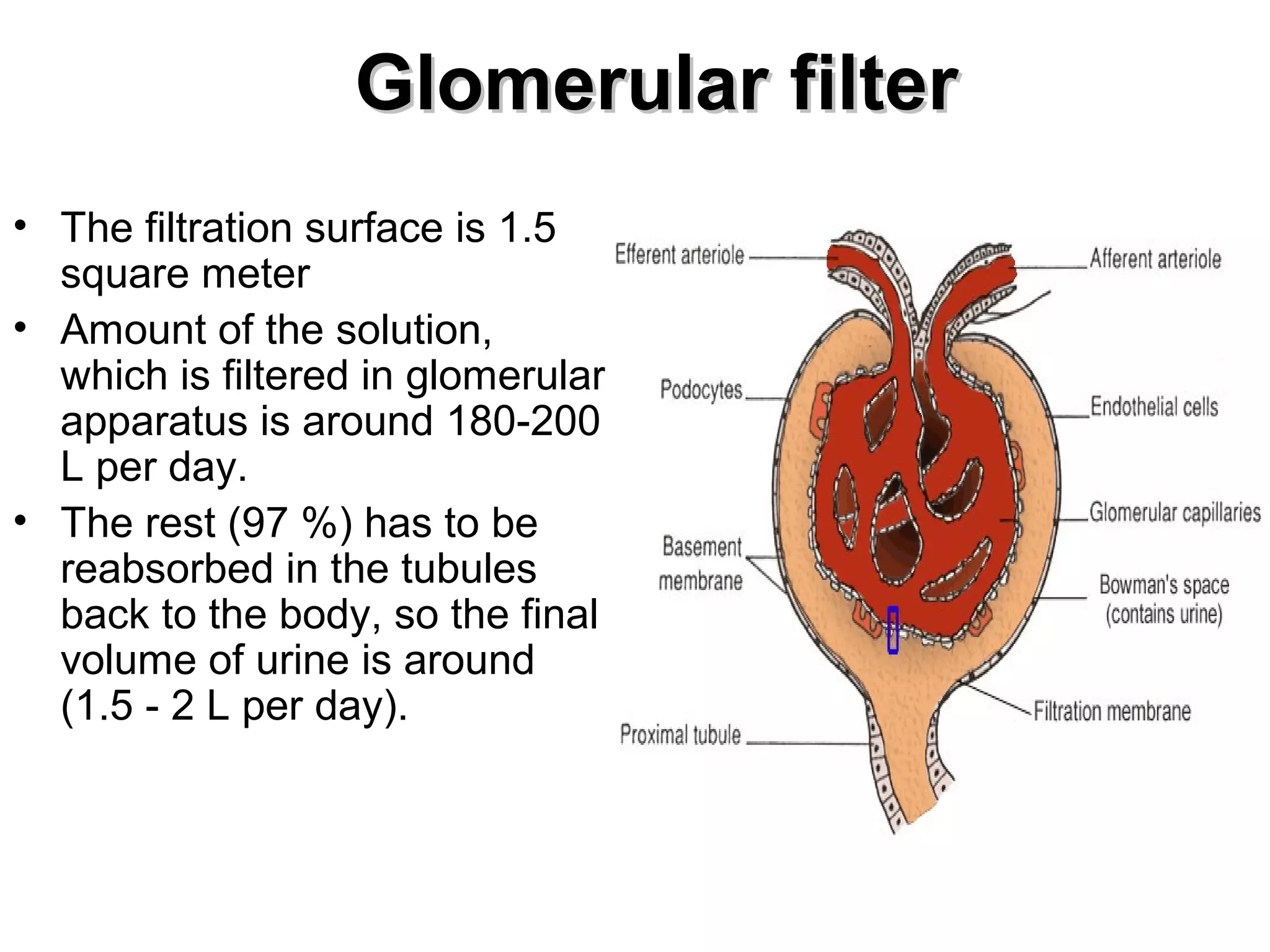
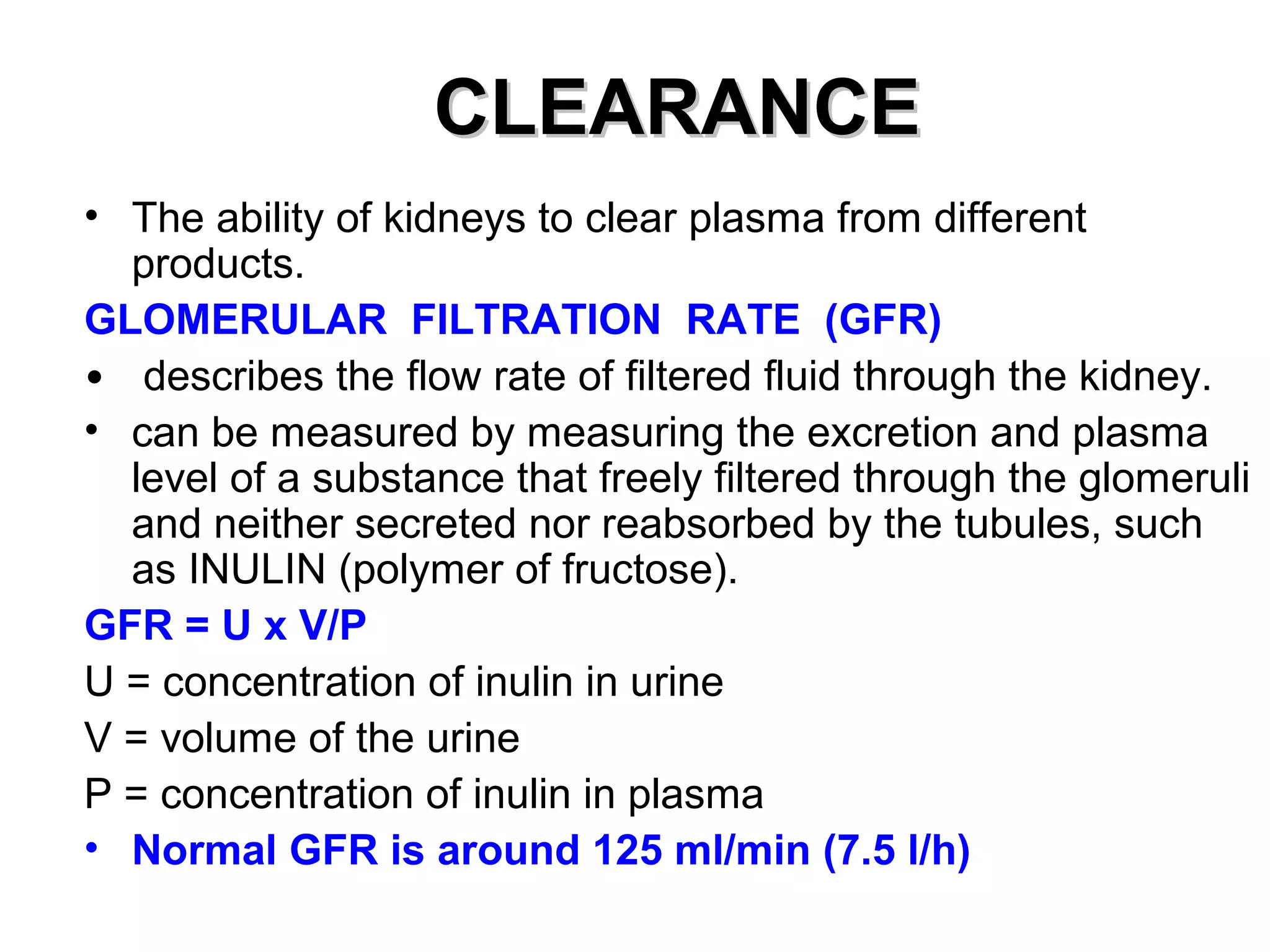
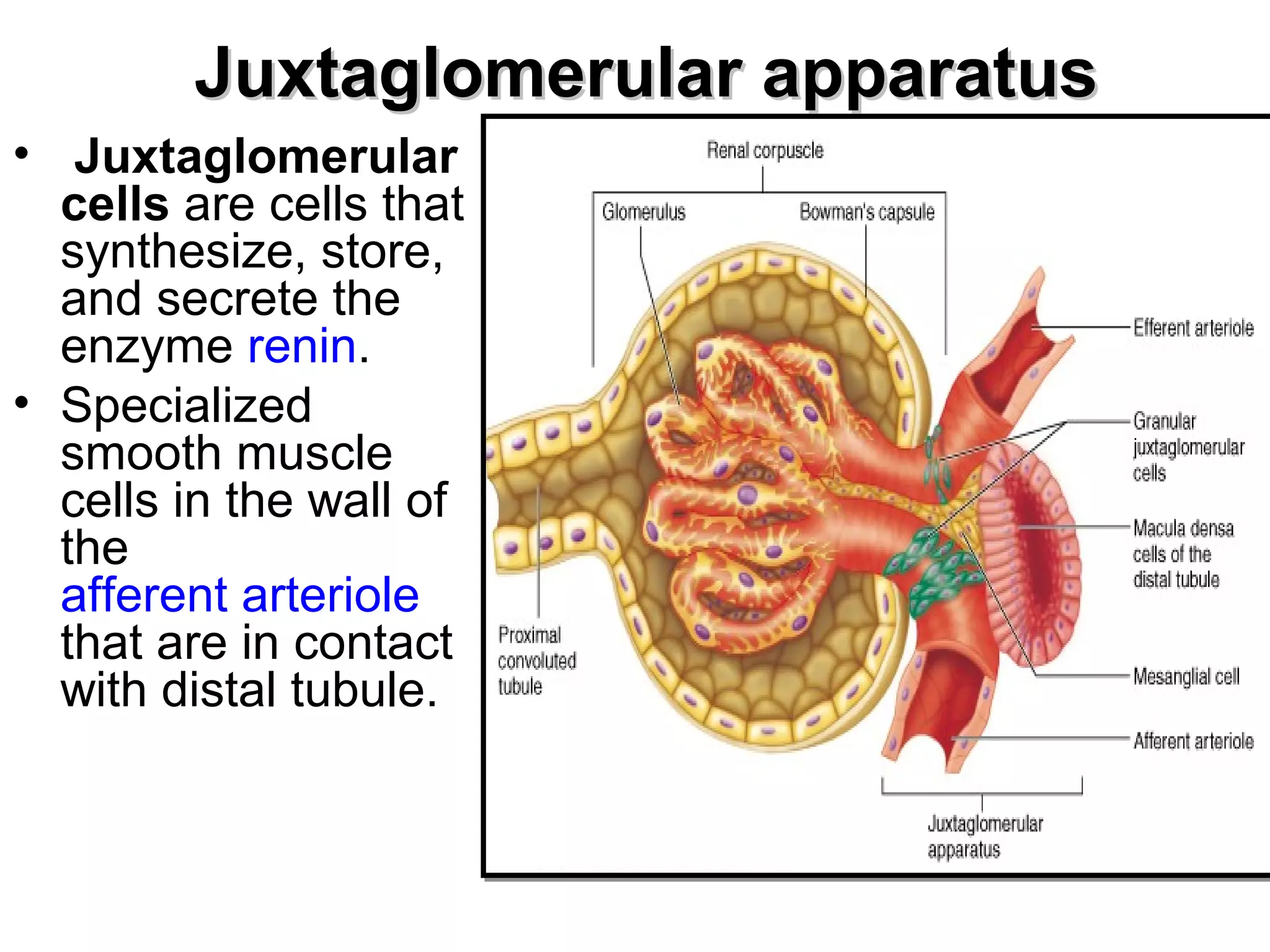
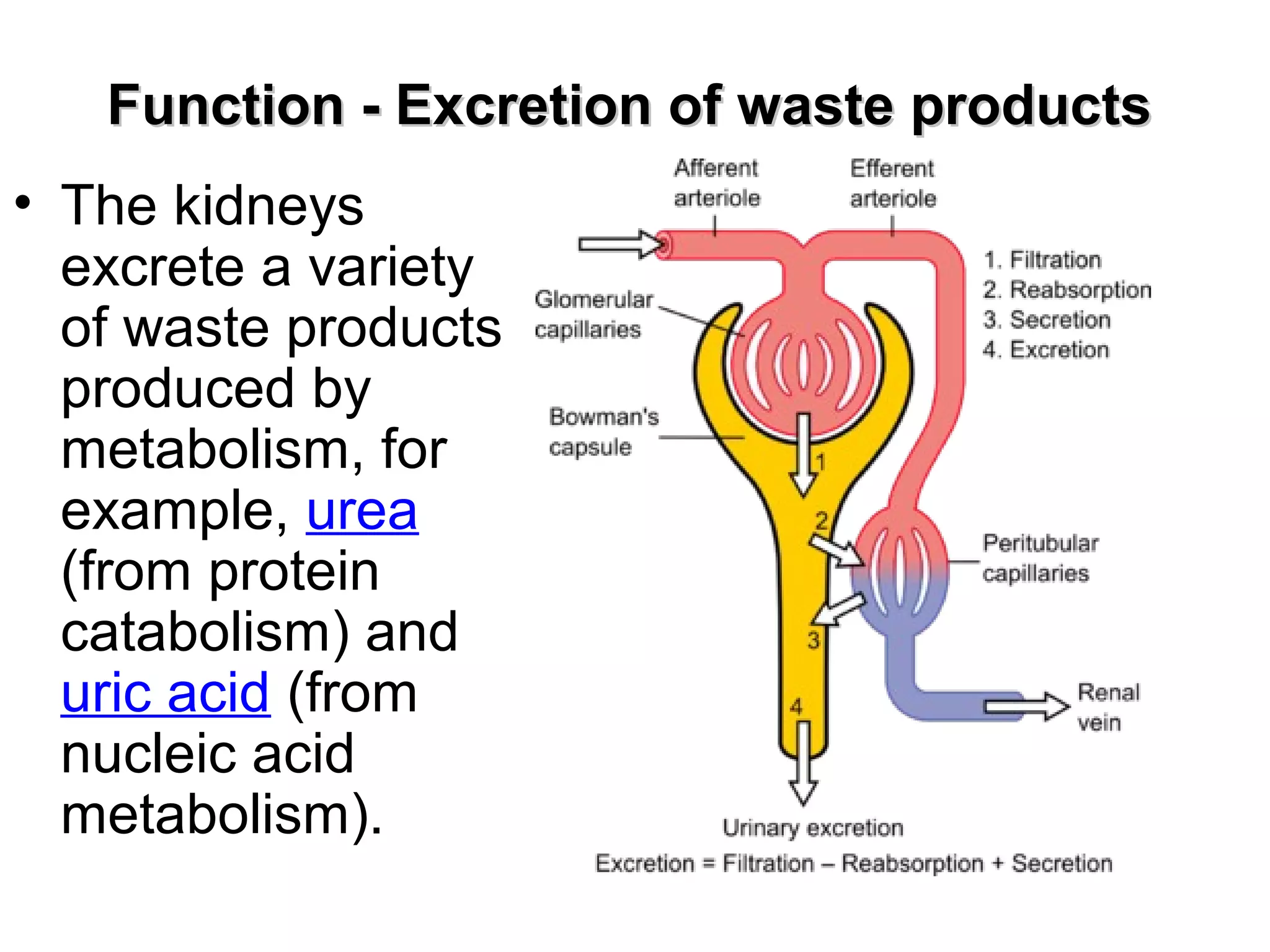
The urinary system includes the kidneys, ureters, urinary bladder, and urethra. The kidneys filter the blood to produce urine, regulating electrolytes and clearing waste. Each kidney contains over 1 million nephrons, the functional units that filter blood in the glomeruli and reabsorb needed substances through the tubules. Urine is stored in the bladder and emptied via the urethra under control of sphincter muscles. The lecture discusses the anatomy and physiology of each component and their roles in homeostasis, acid-base balance, and excretion.