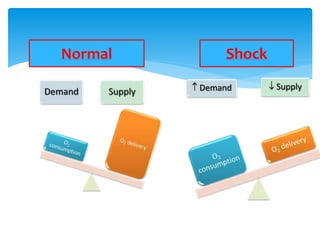
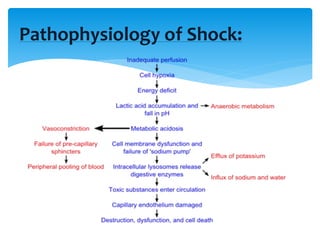
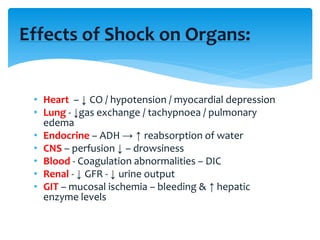
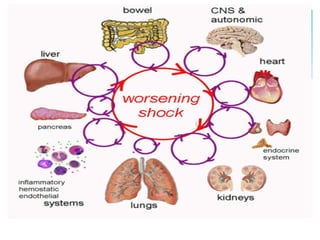
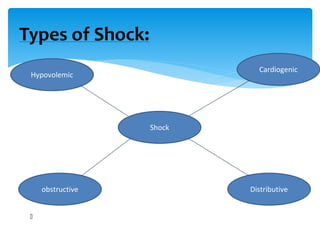
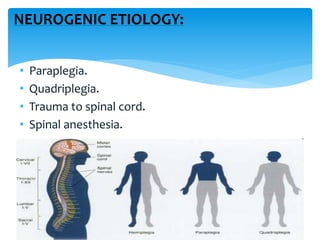
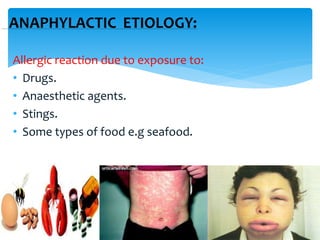
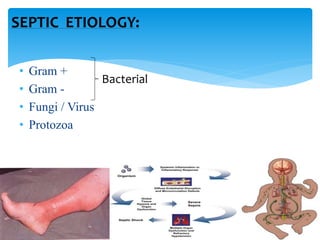
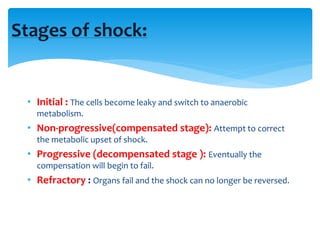
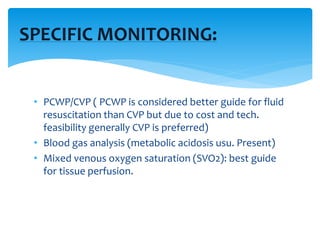
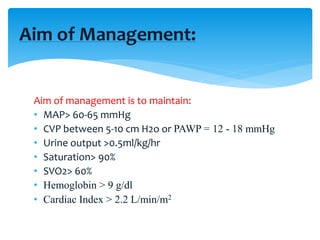
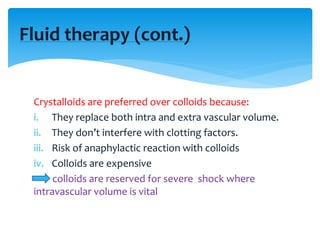
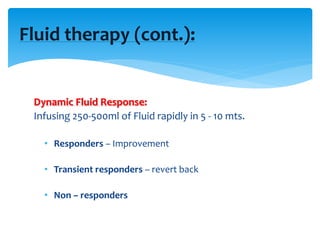
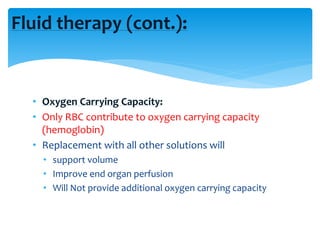
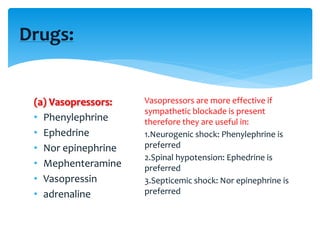
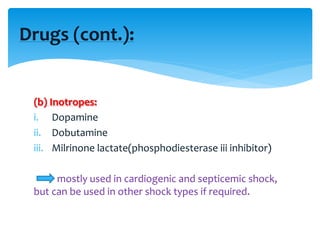
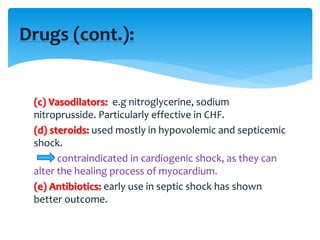
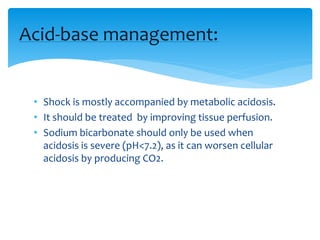
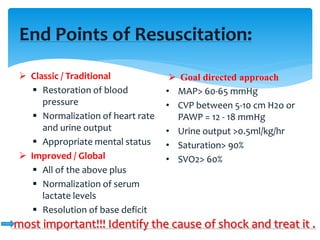
Shock is a state of poor tissue perfusion that can result from various causes like hemorrhage, infection, trauma, etc. It impairs cellular metabolism. There are several types of shock including hypovolemic, cardiogenic, obstructive, distributive, and neurogenic shock. The management involves treating the underlying cause, improving cardiac function and tissue perfusion through fluid resuscitation, vasopressors, inotropes, and other supportive measures. The goals are to maintain adequate blood pressure, urine output, oxygen delivery and other parameters. Early identification and treatment of the cause is critical to reversing shock.