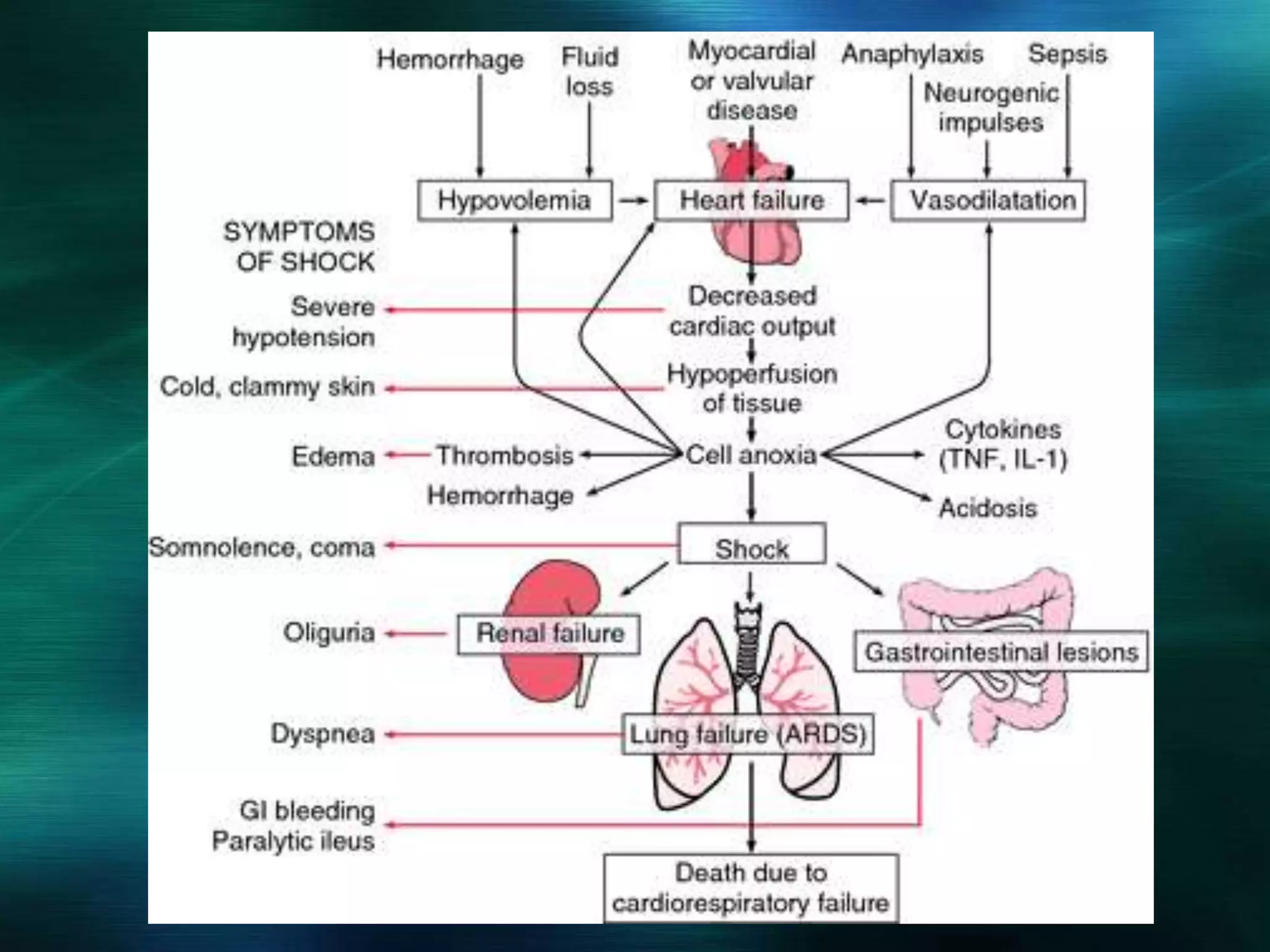
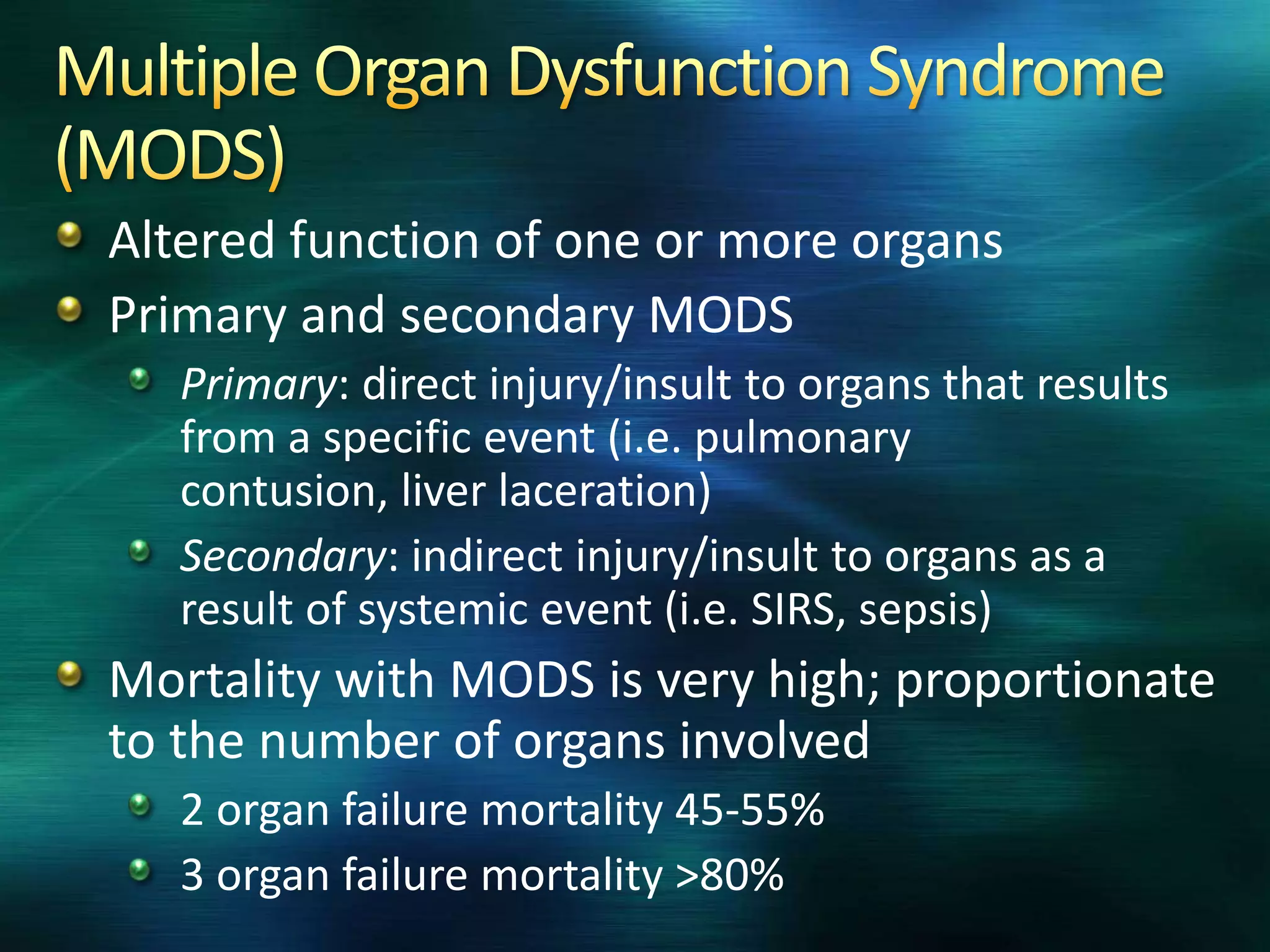
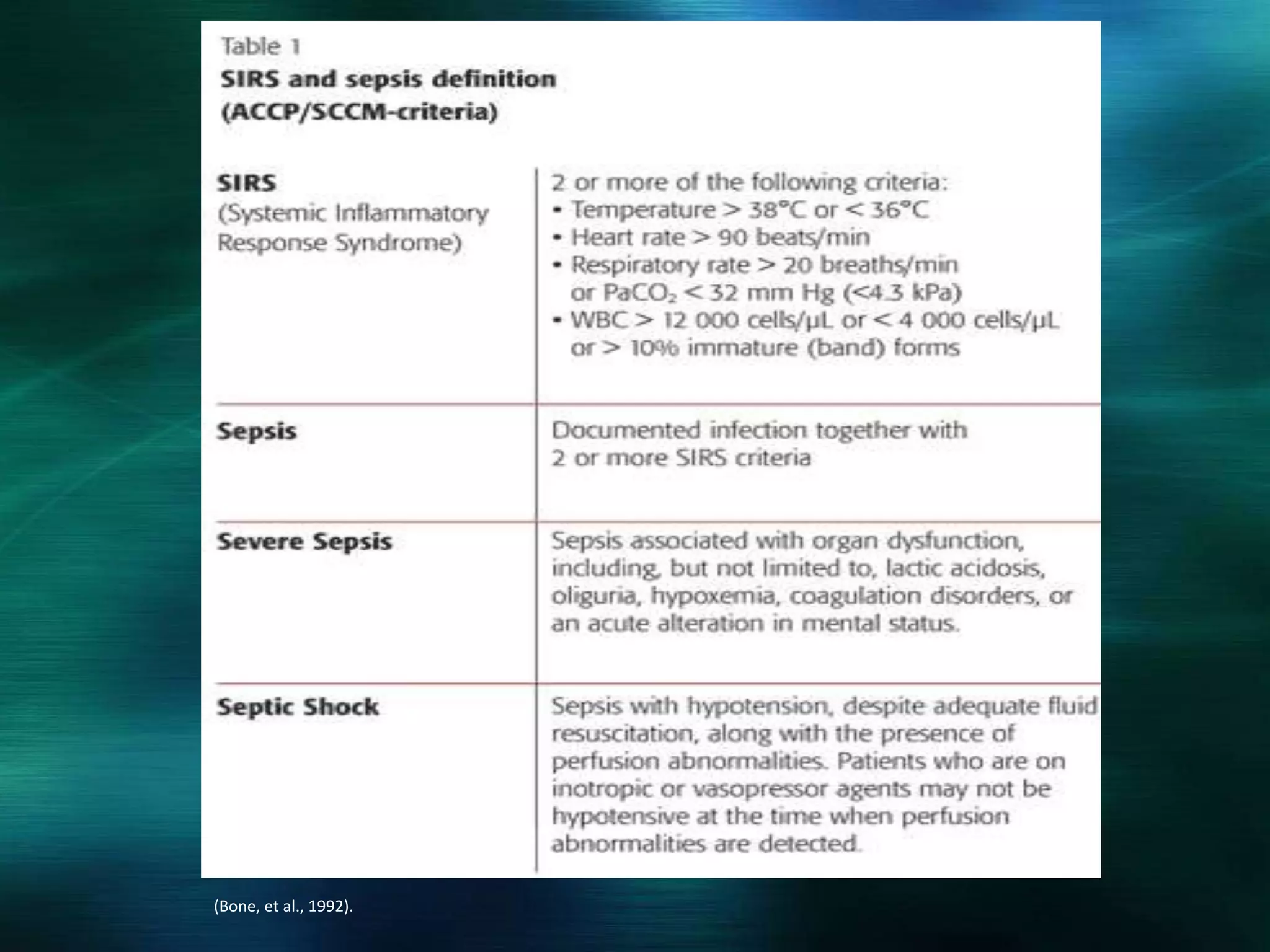
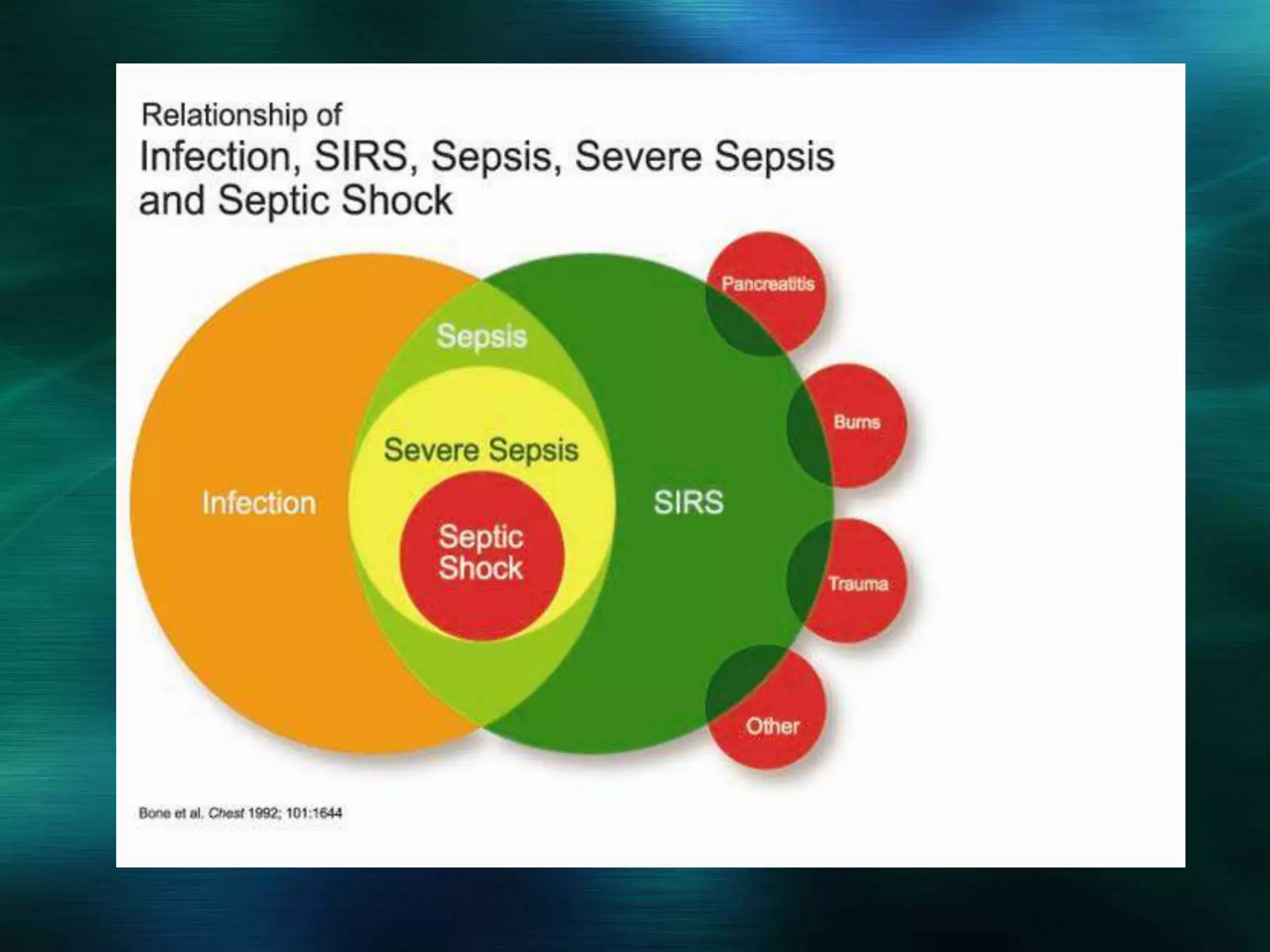
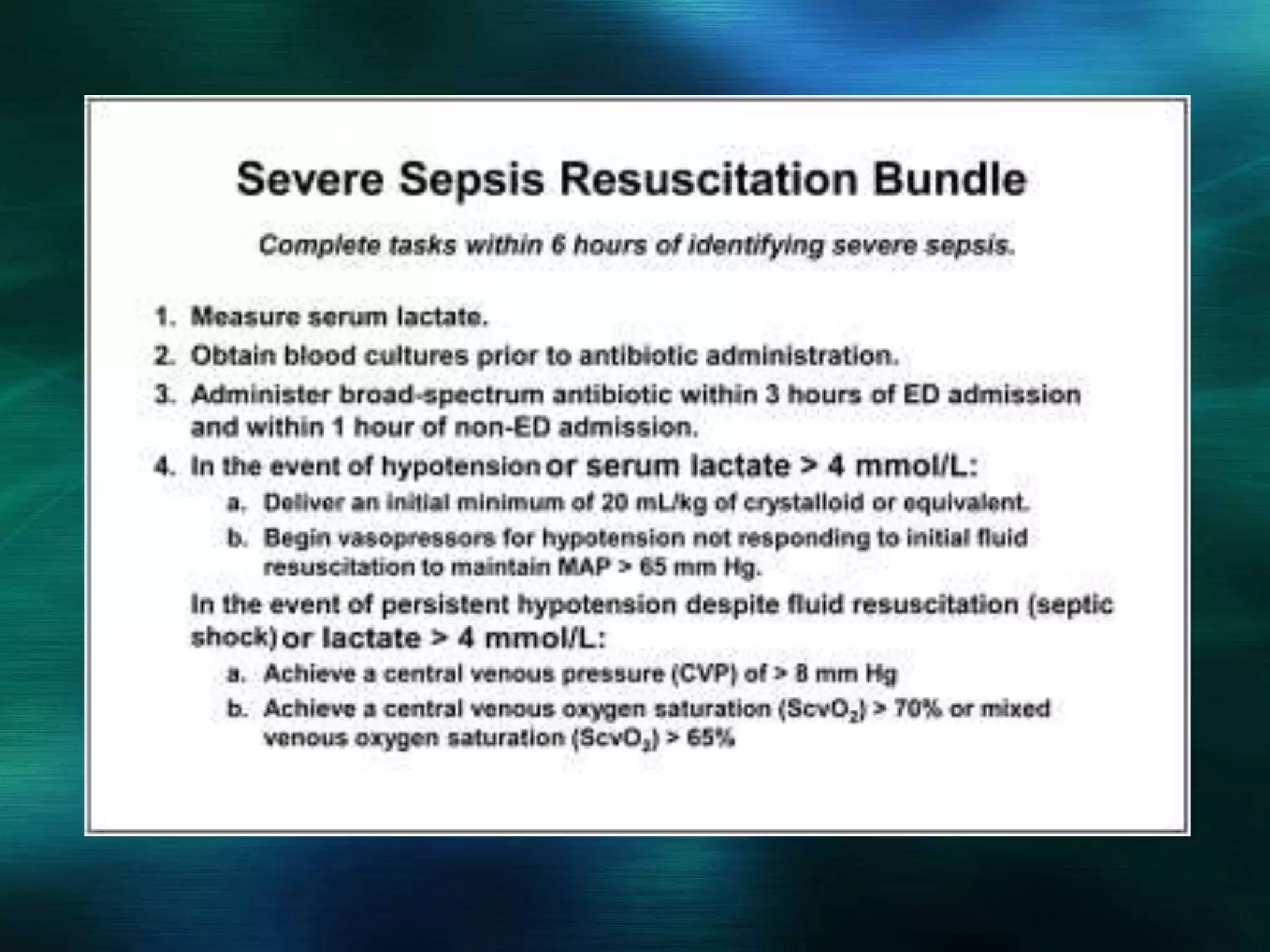
Sepsis is a clinical syndrome resulting from a dysregulated inflammatory response to infection. It occurs on a continuum from systemic inflammatory response syndrome (SIRS) to sepsis to septic shock and multiple organ dysfunction syndrome (MODS). Sepsis affects over 750,000 Americans annually and is a leading cause of death, with high mortality rates the more severe the presentation becomes. Early recognition and treatment, including antibiotics within 1-3 hours, fluids, and vasopressors if needed, are critical to improving outcomes.