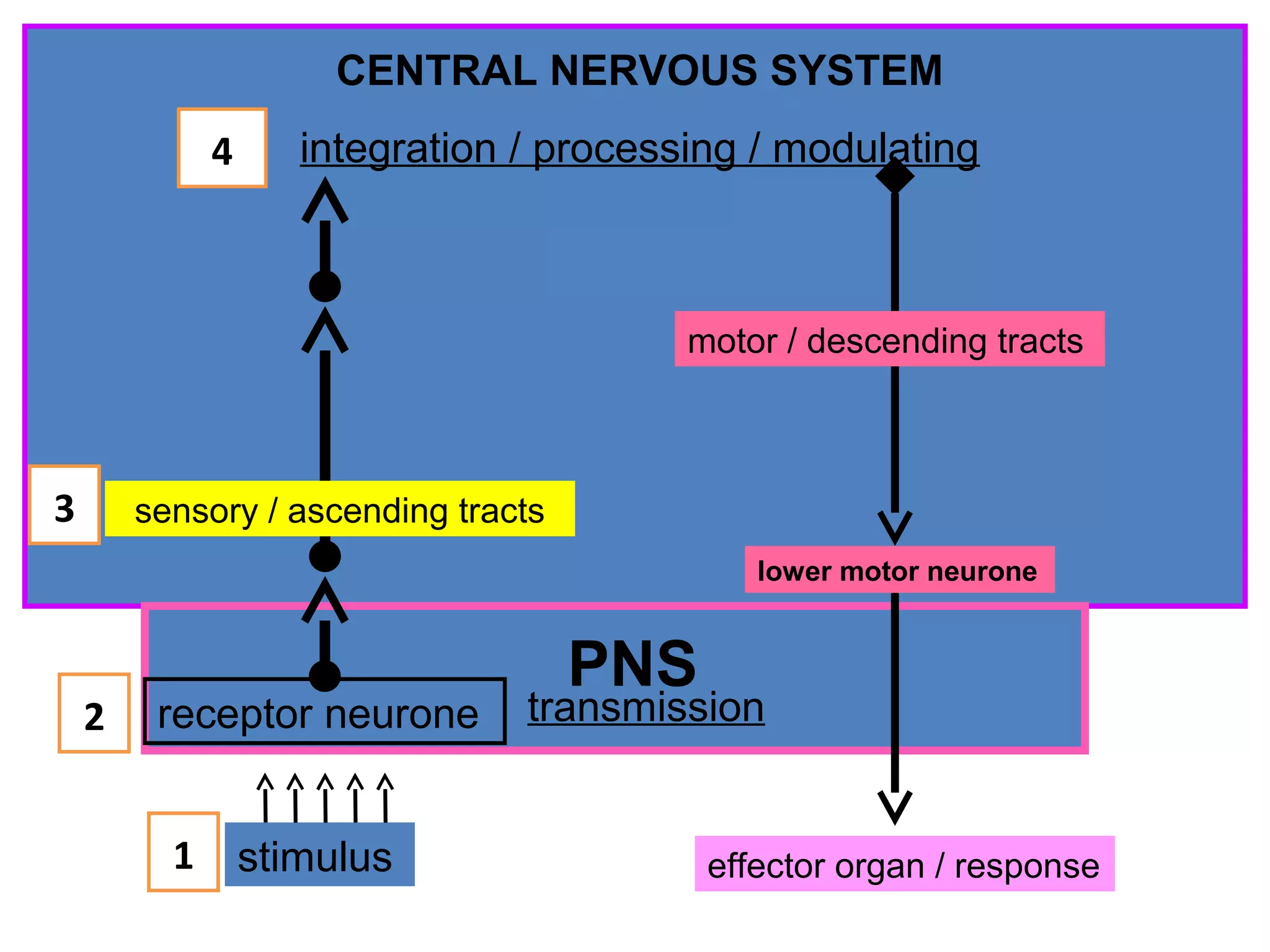
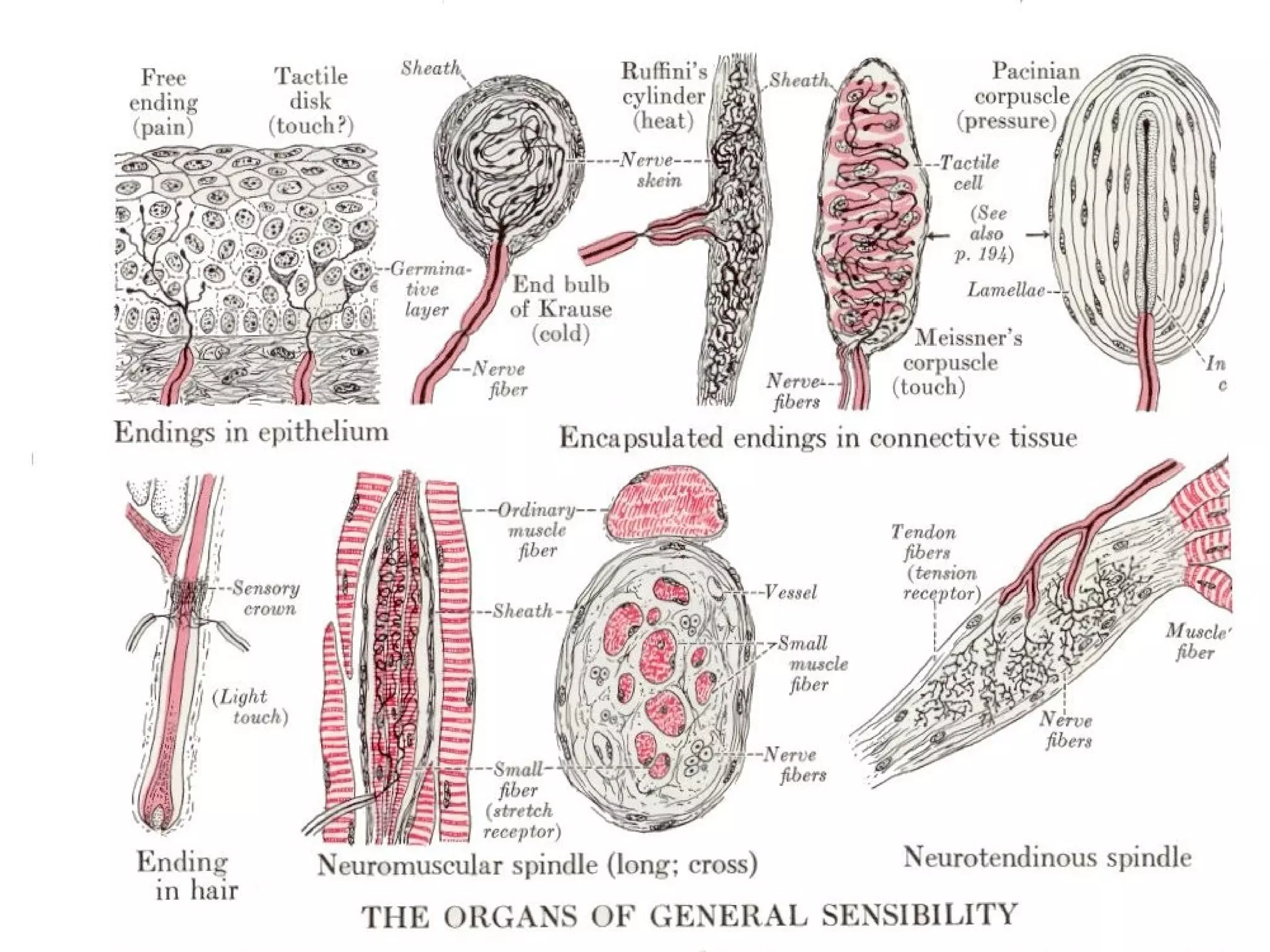
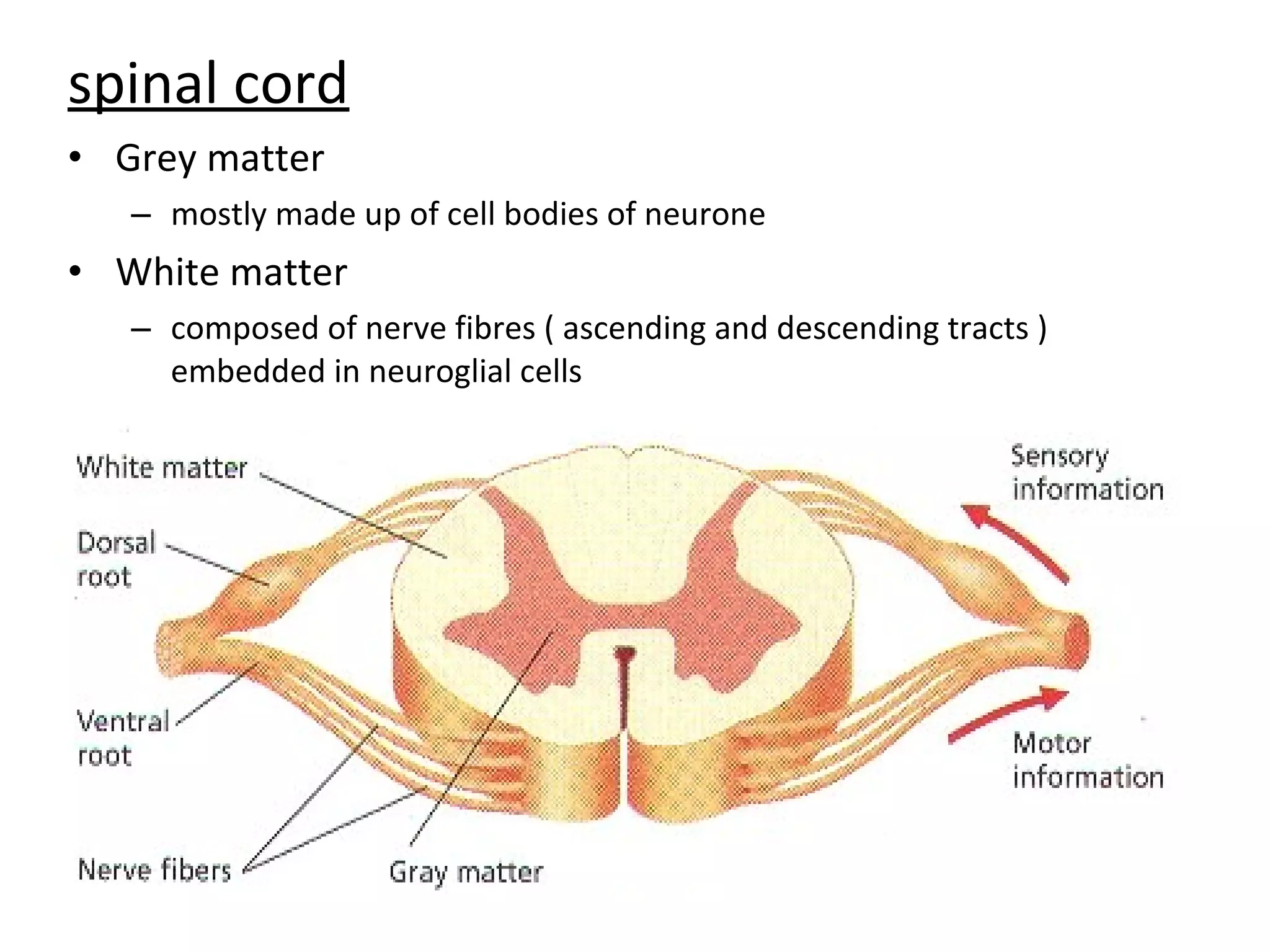
This document summarizes the key components of the human sensory system. It describes how sensory information is received by receptors, transmitted through neurons in the peripheral and central nervous systems, and integrated and processed in the brain. Specifically, it discusses:
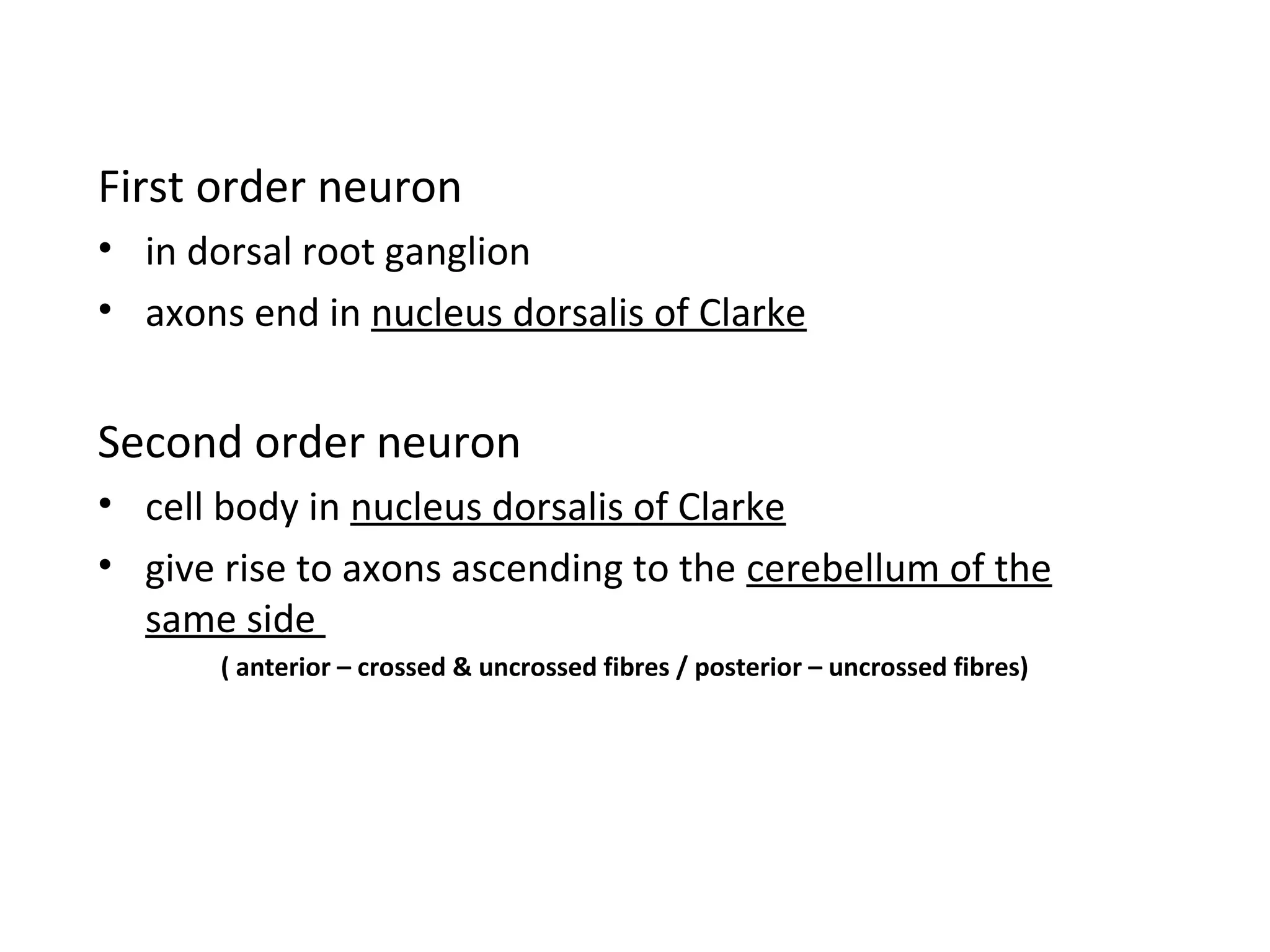
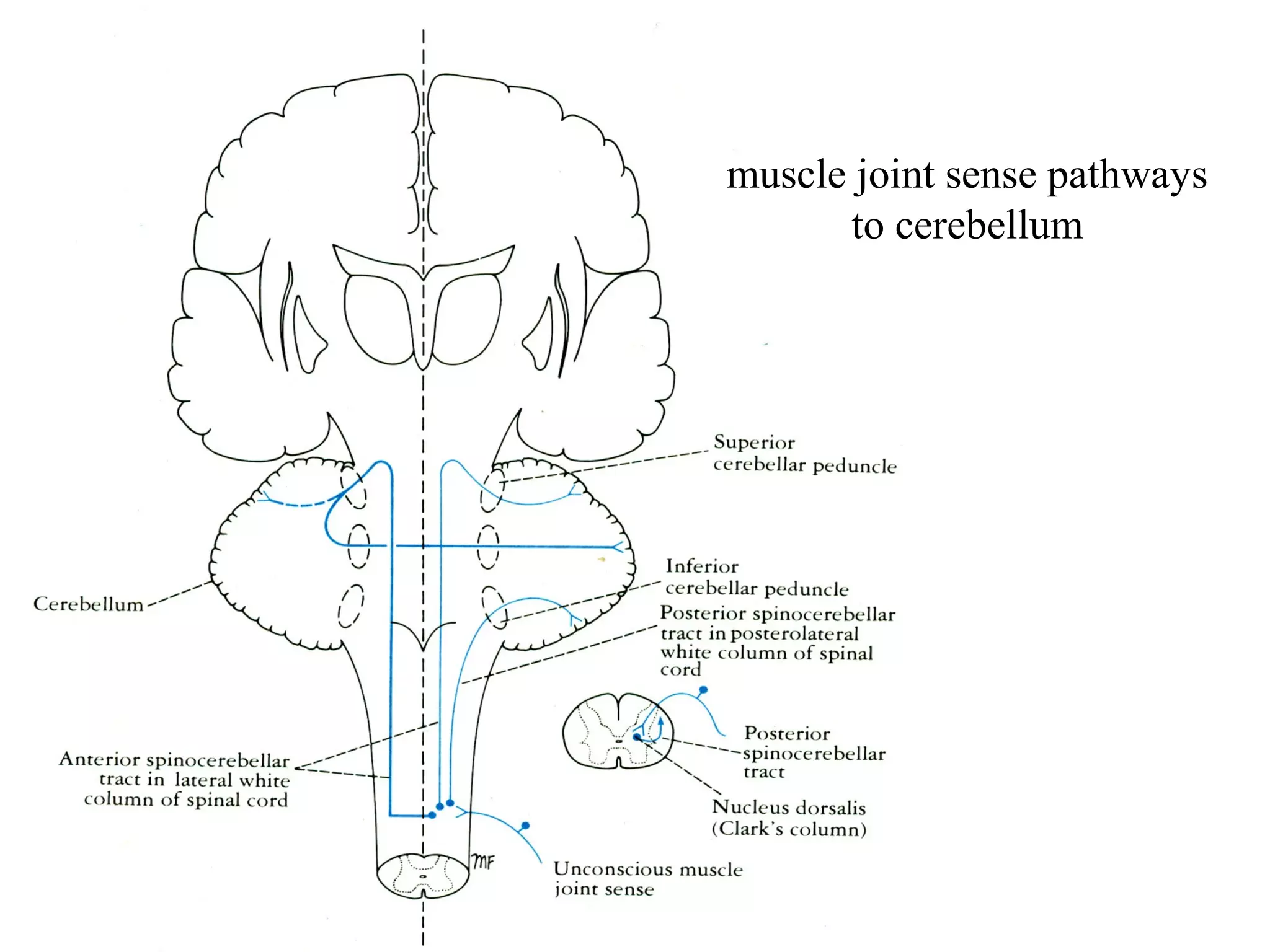
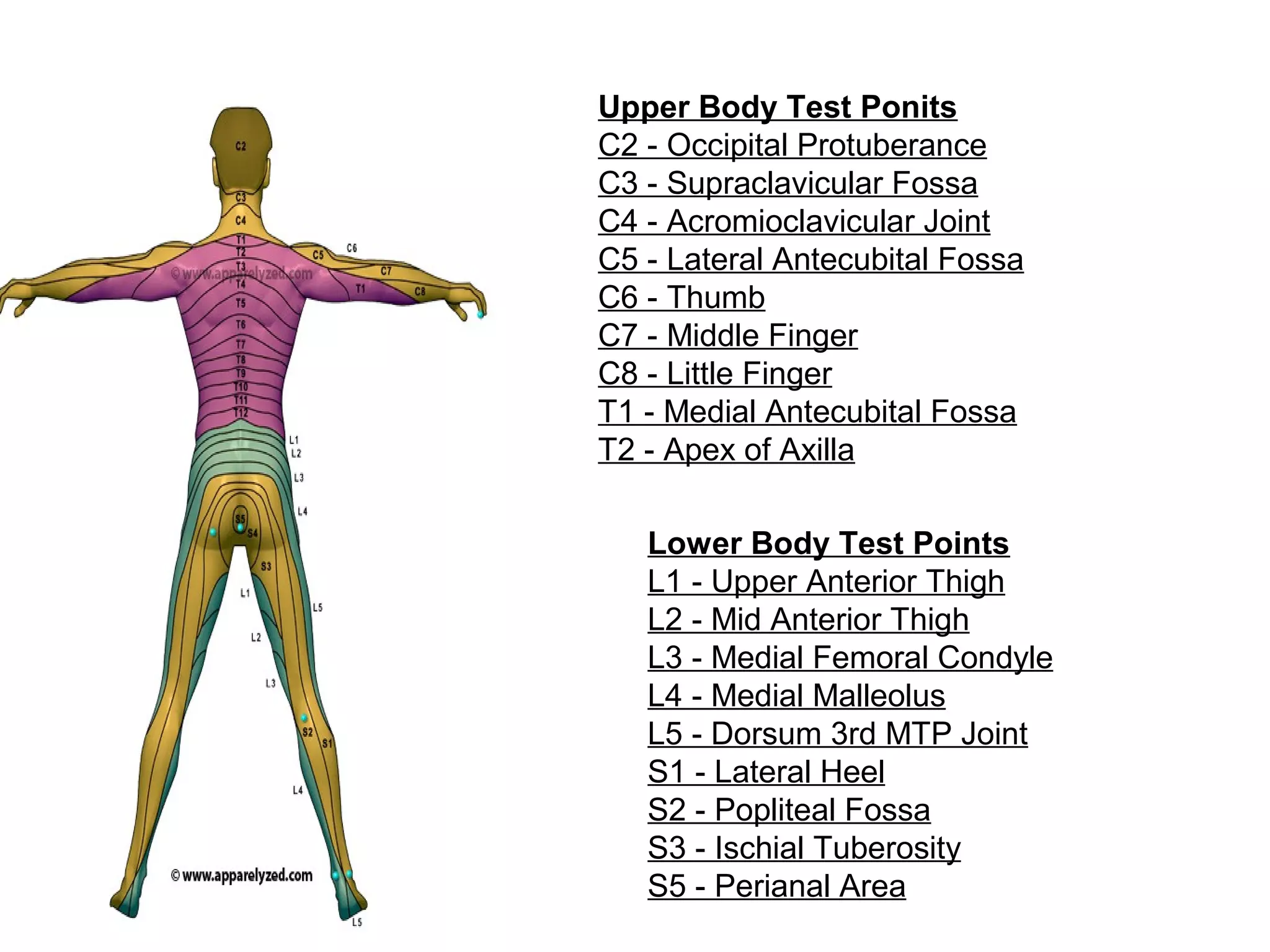
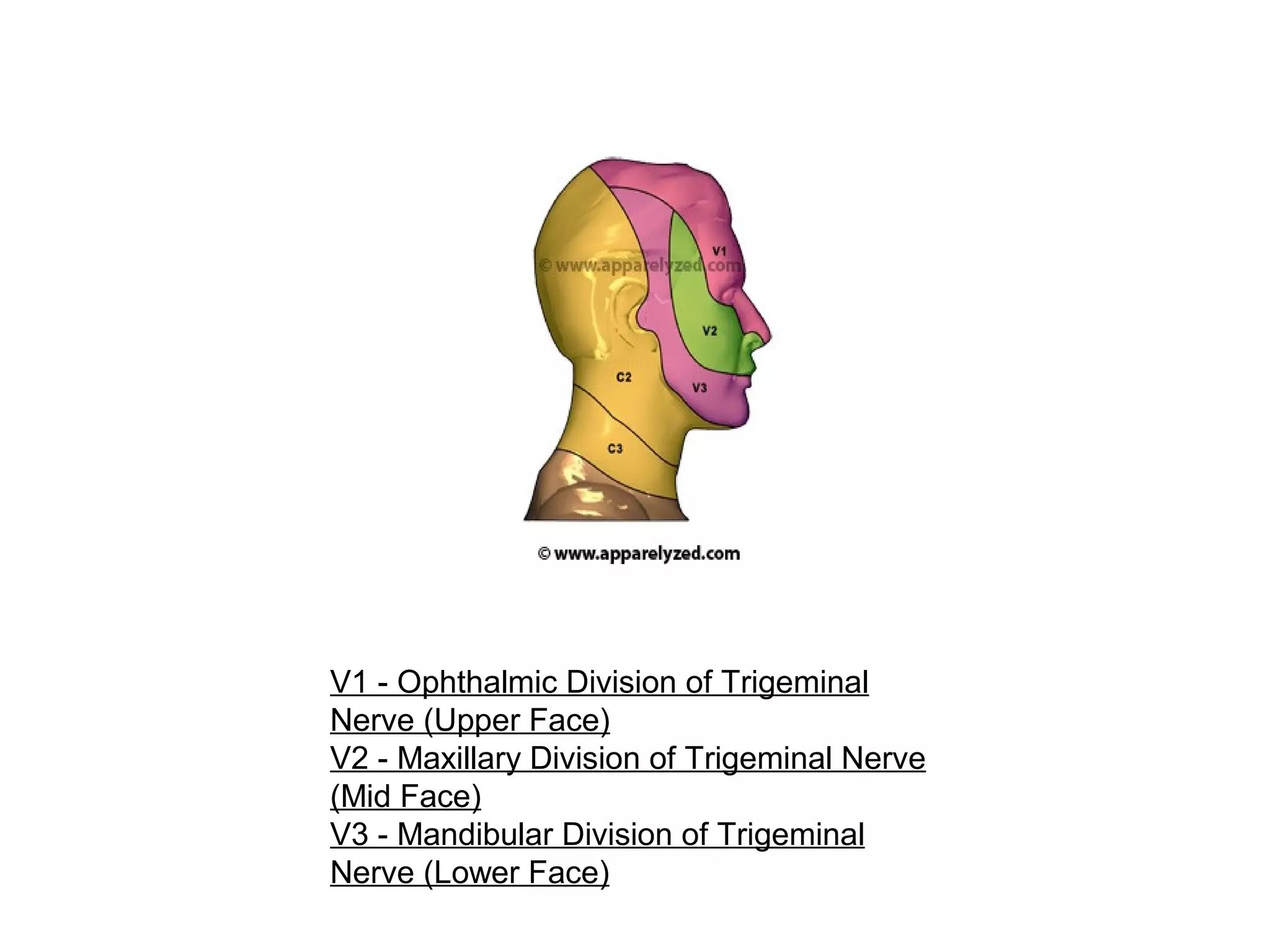
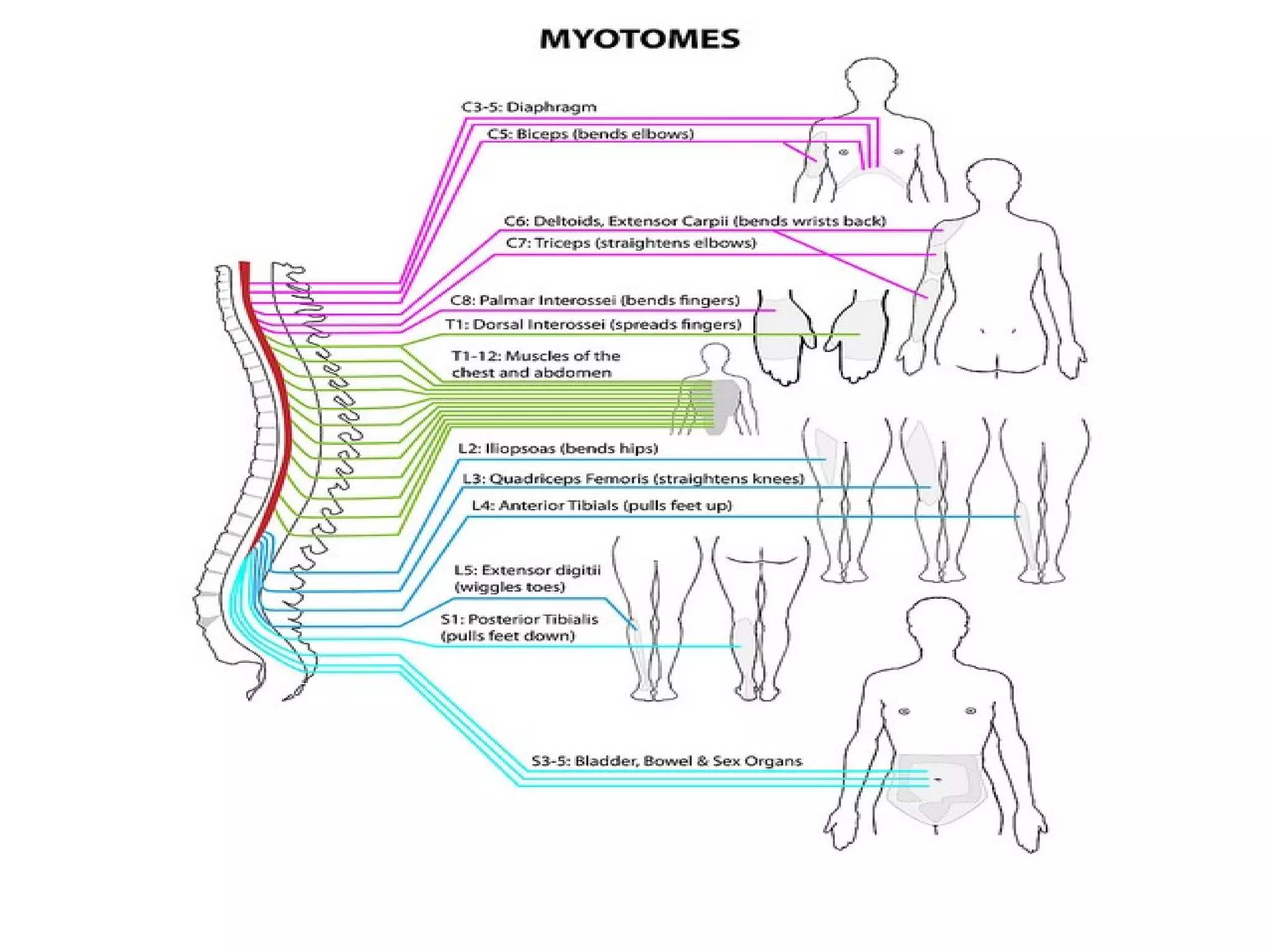
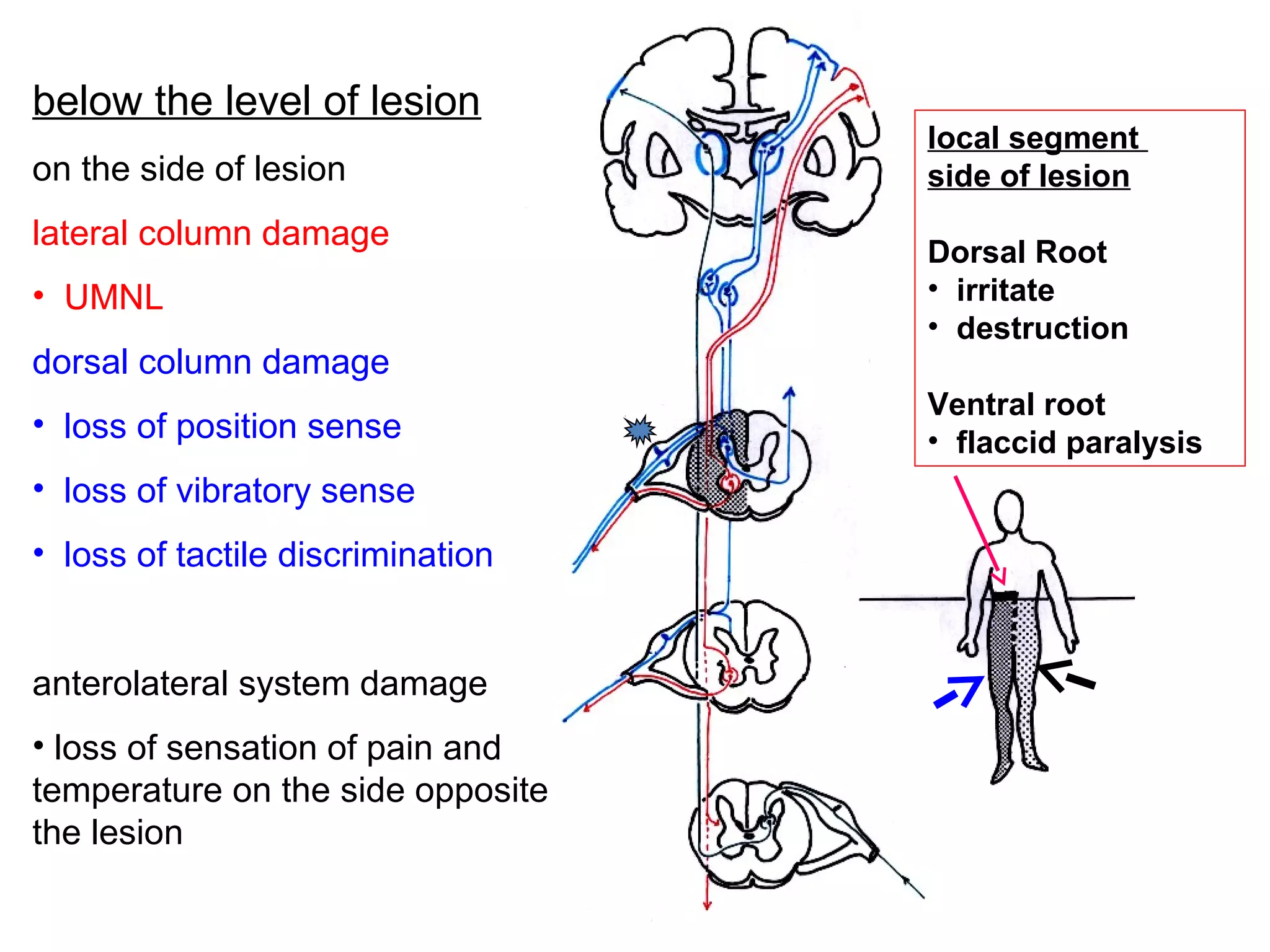
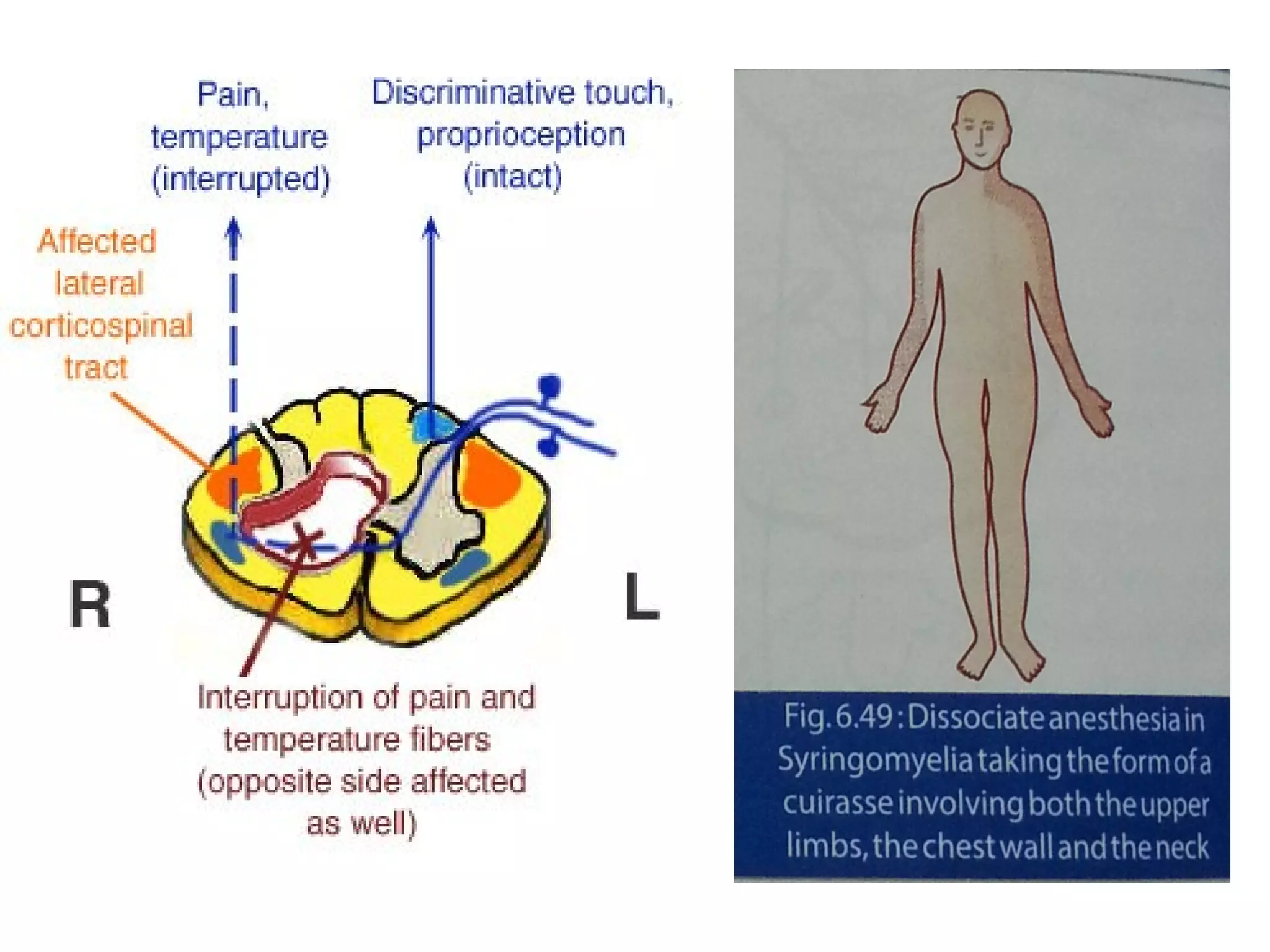
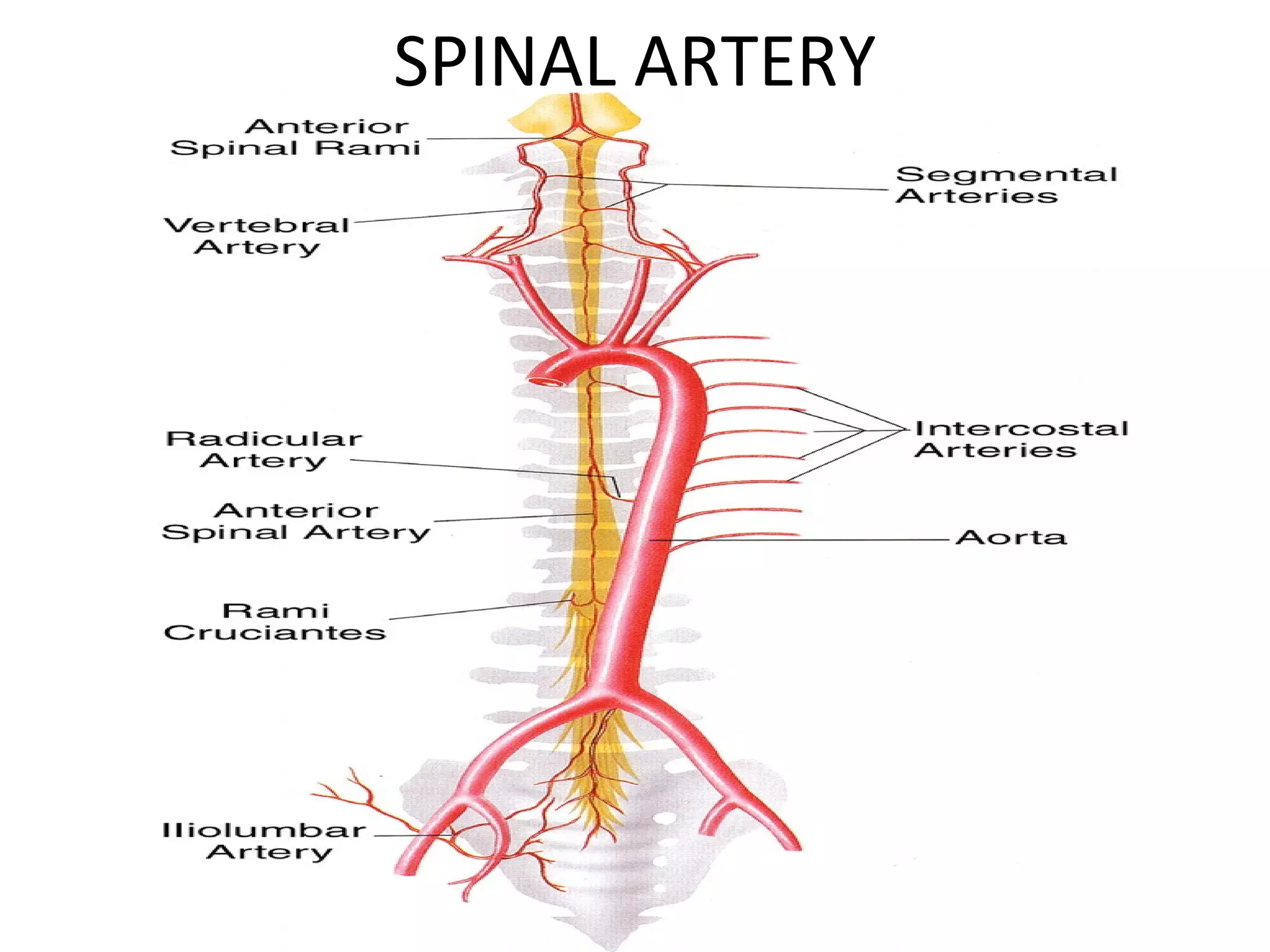
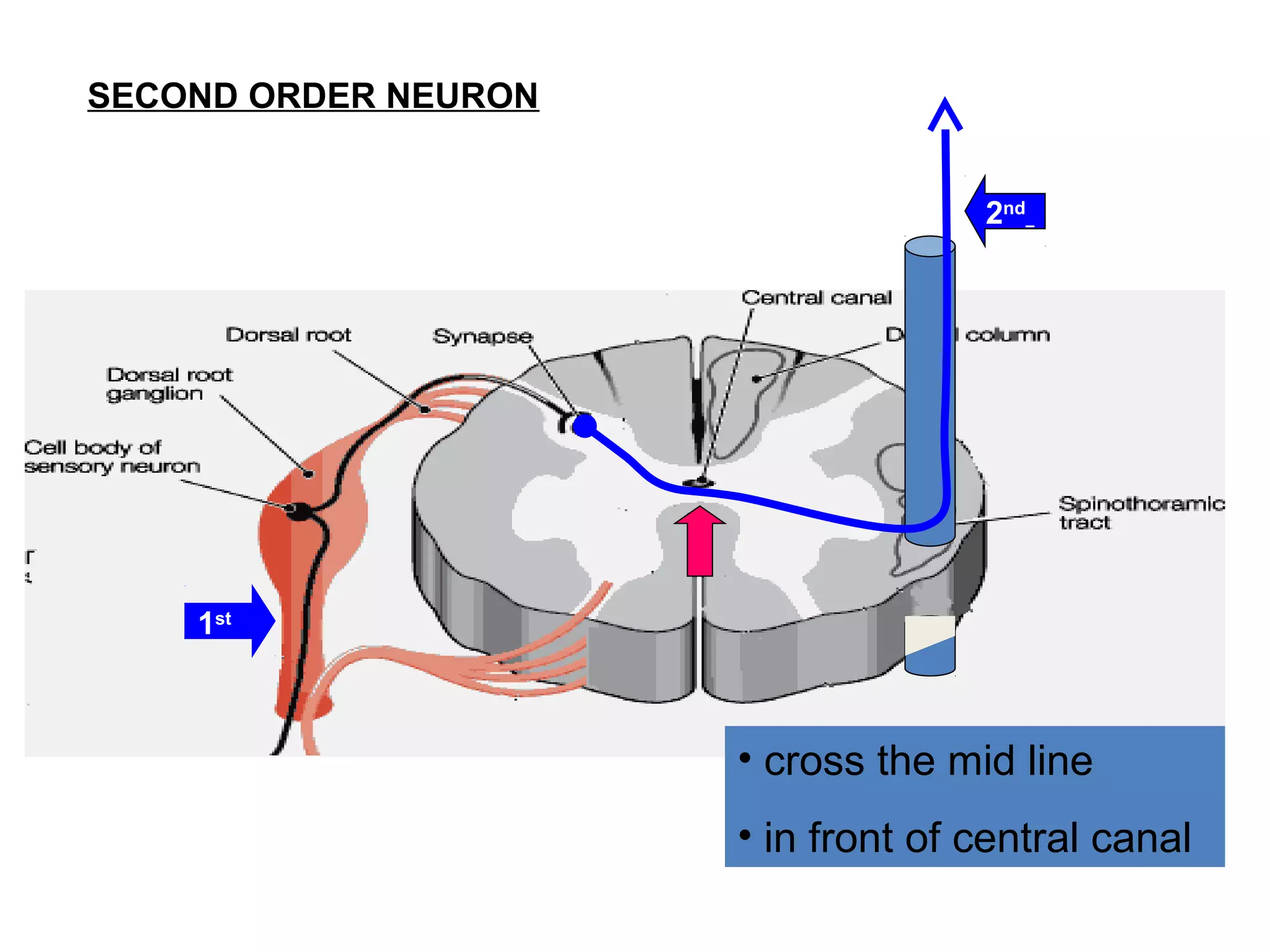
1) The pathways for different sensory modalities from receptors to the spinal cord and brain, including pain/temperature, touch, and proprioception.
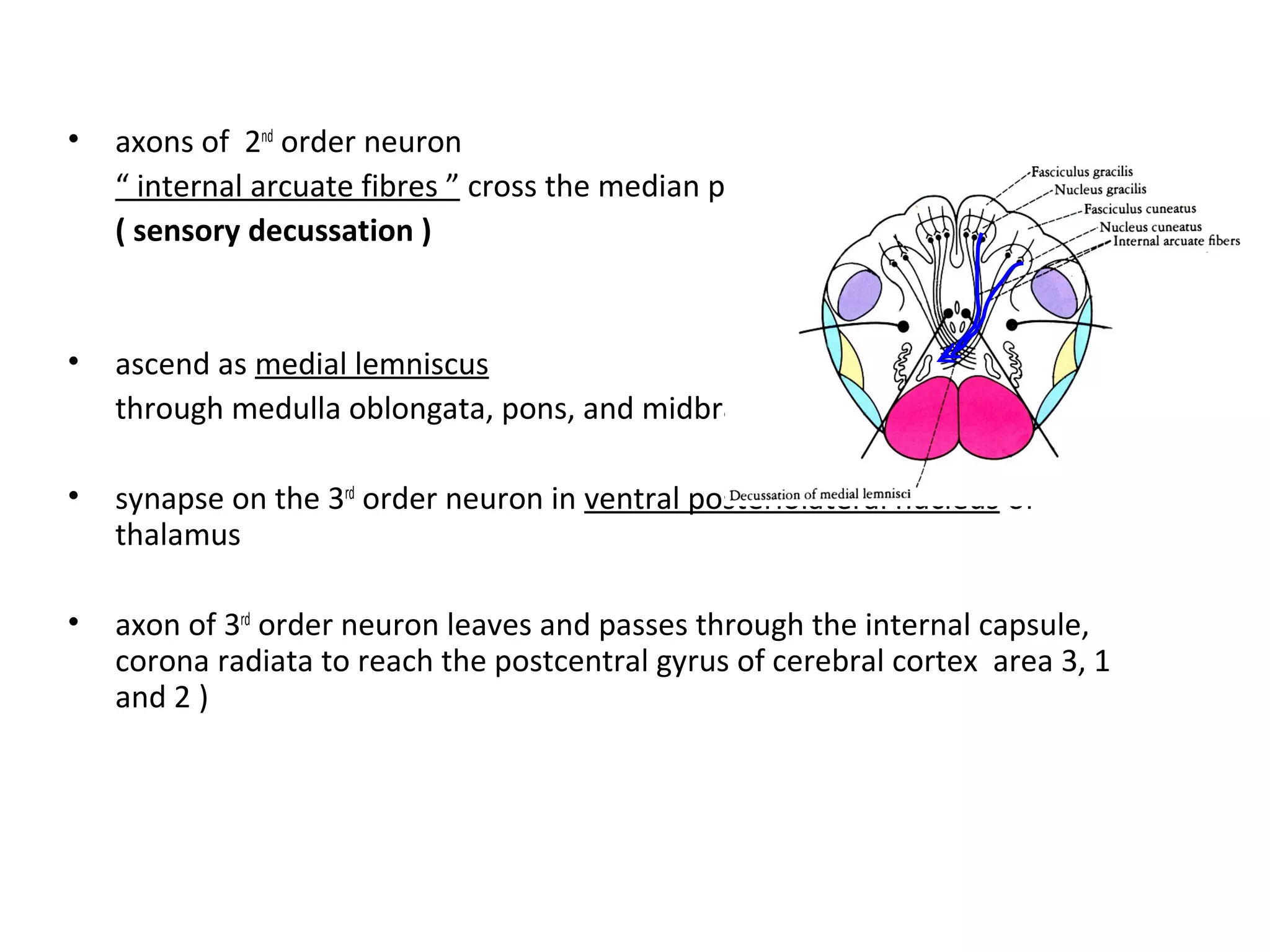
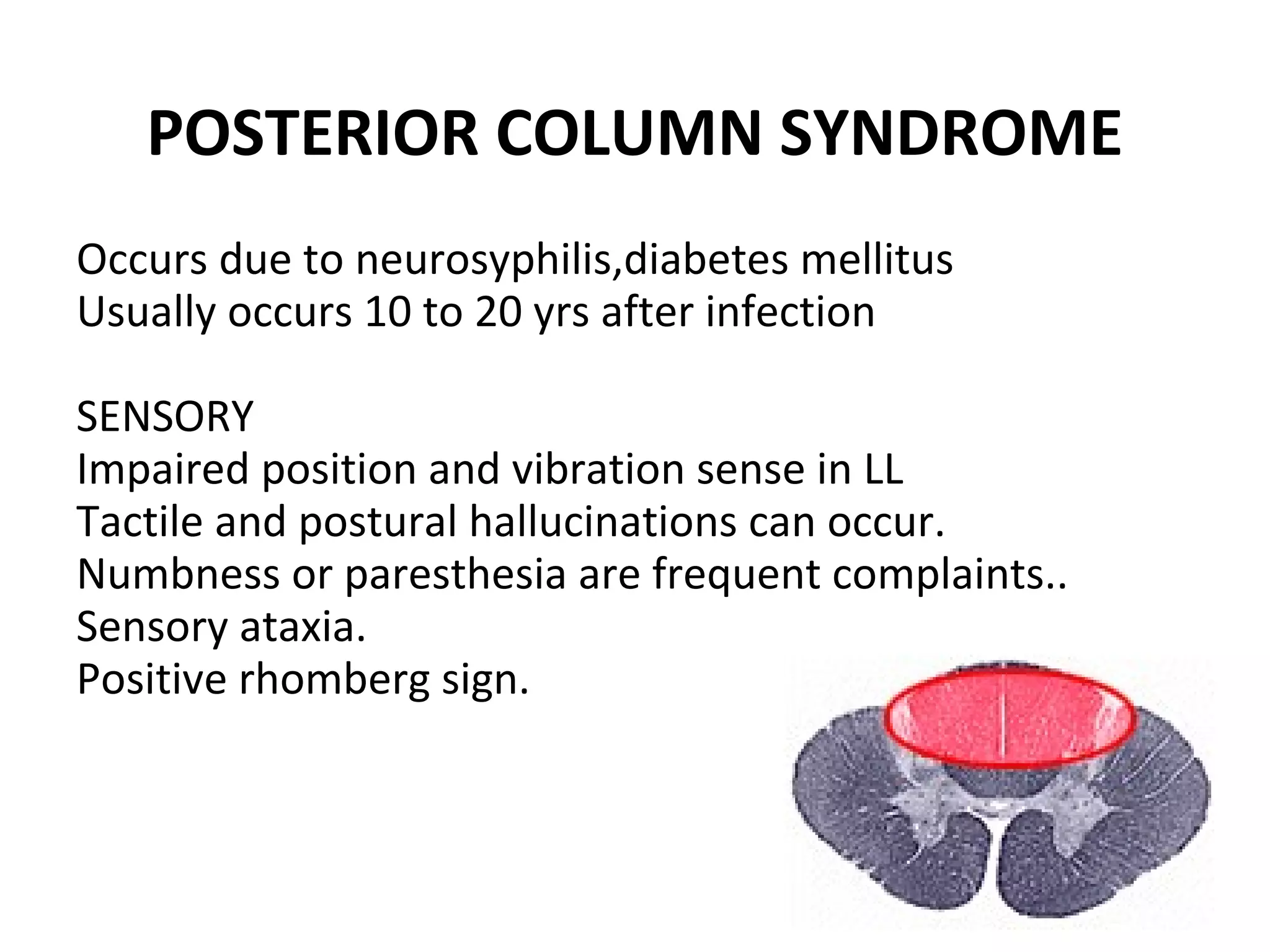
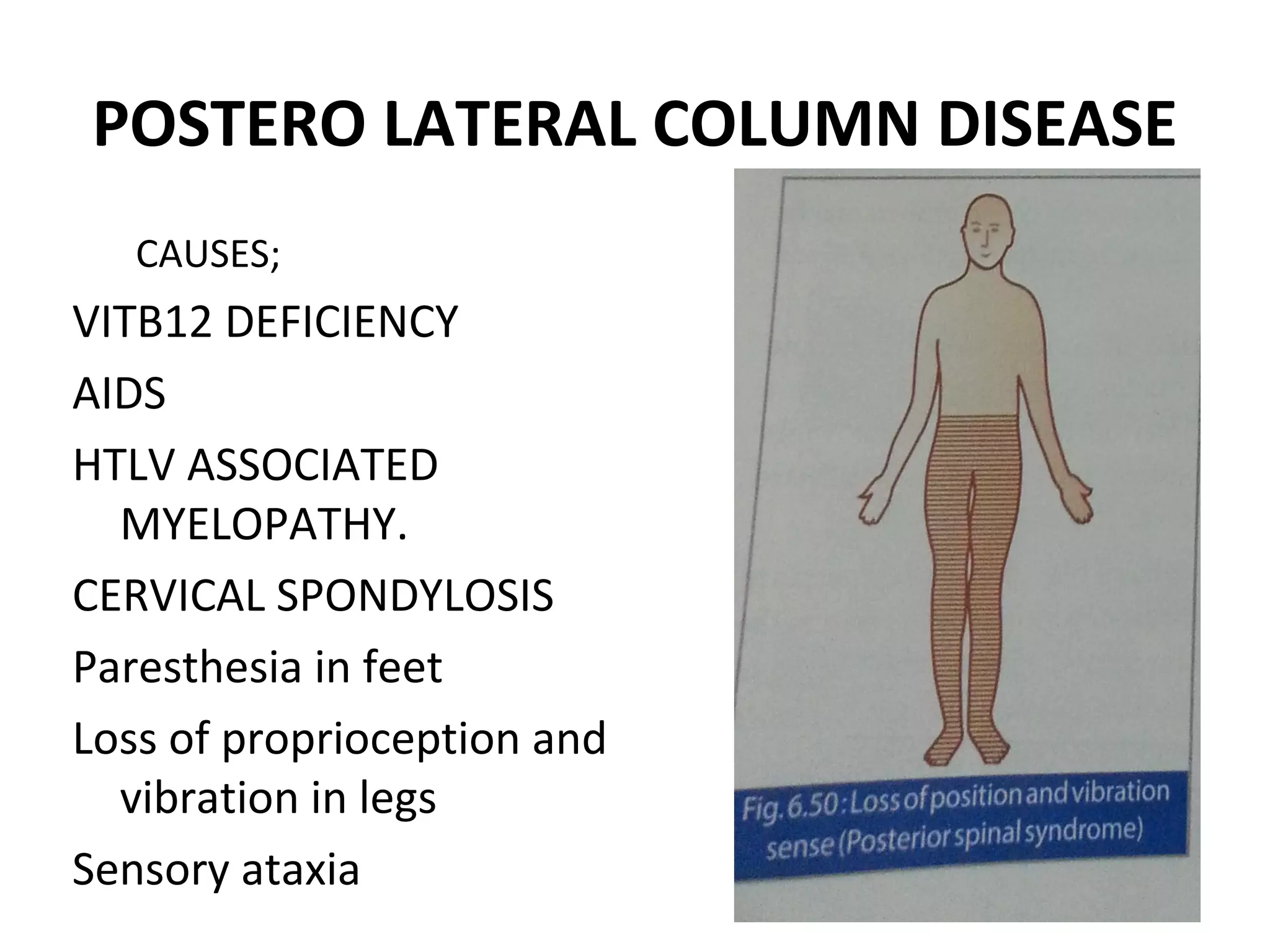
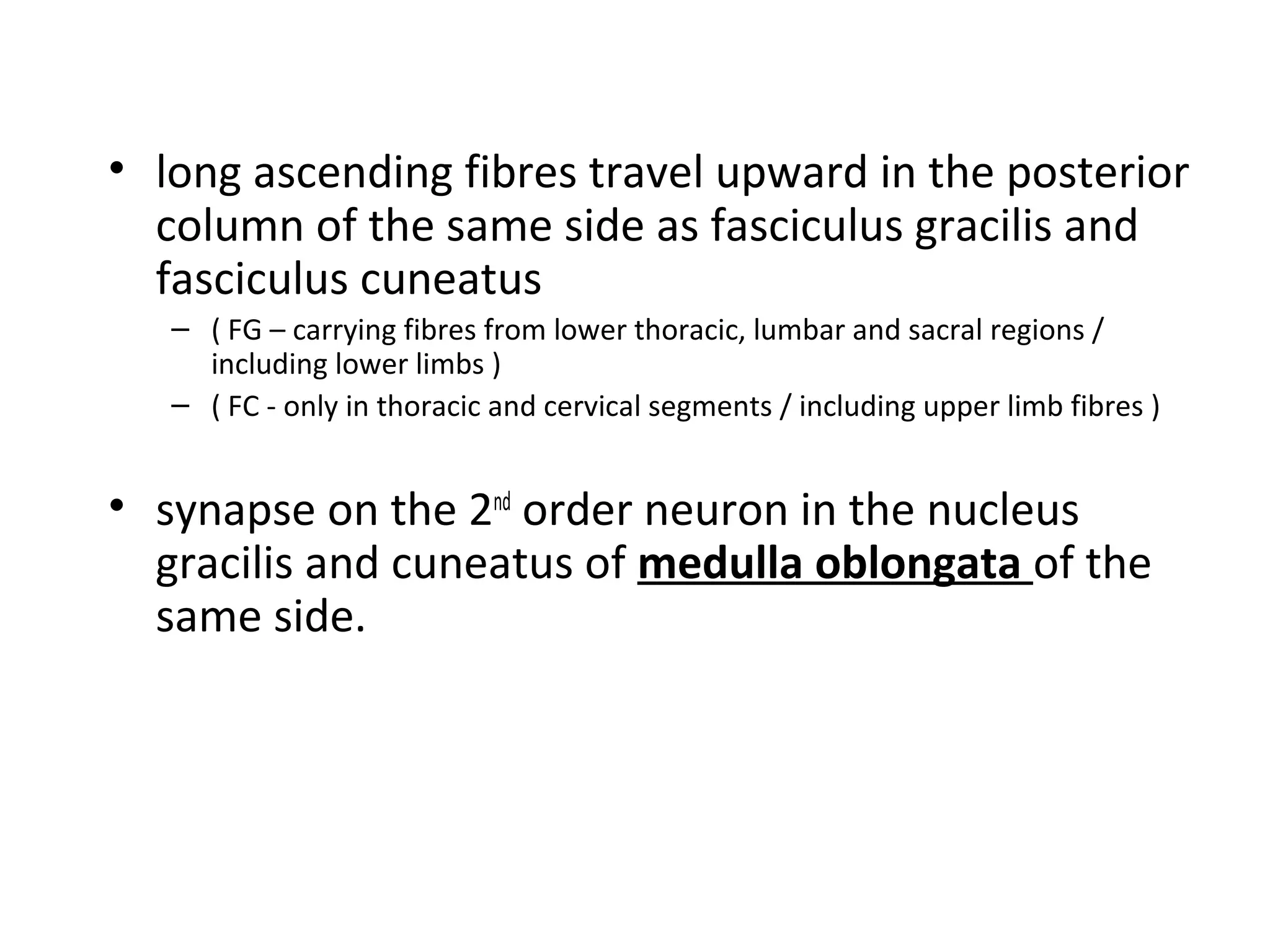
2) The ascending tracts that transmit sensory information from the spinal cord to the brain, such as the lateral spinothalamic, anterior spinothalamic, and posterior columns.
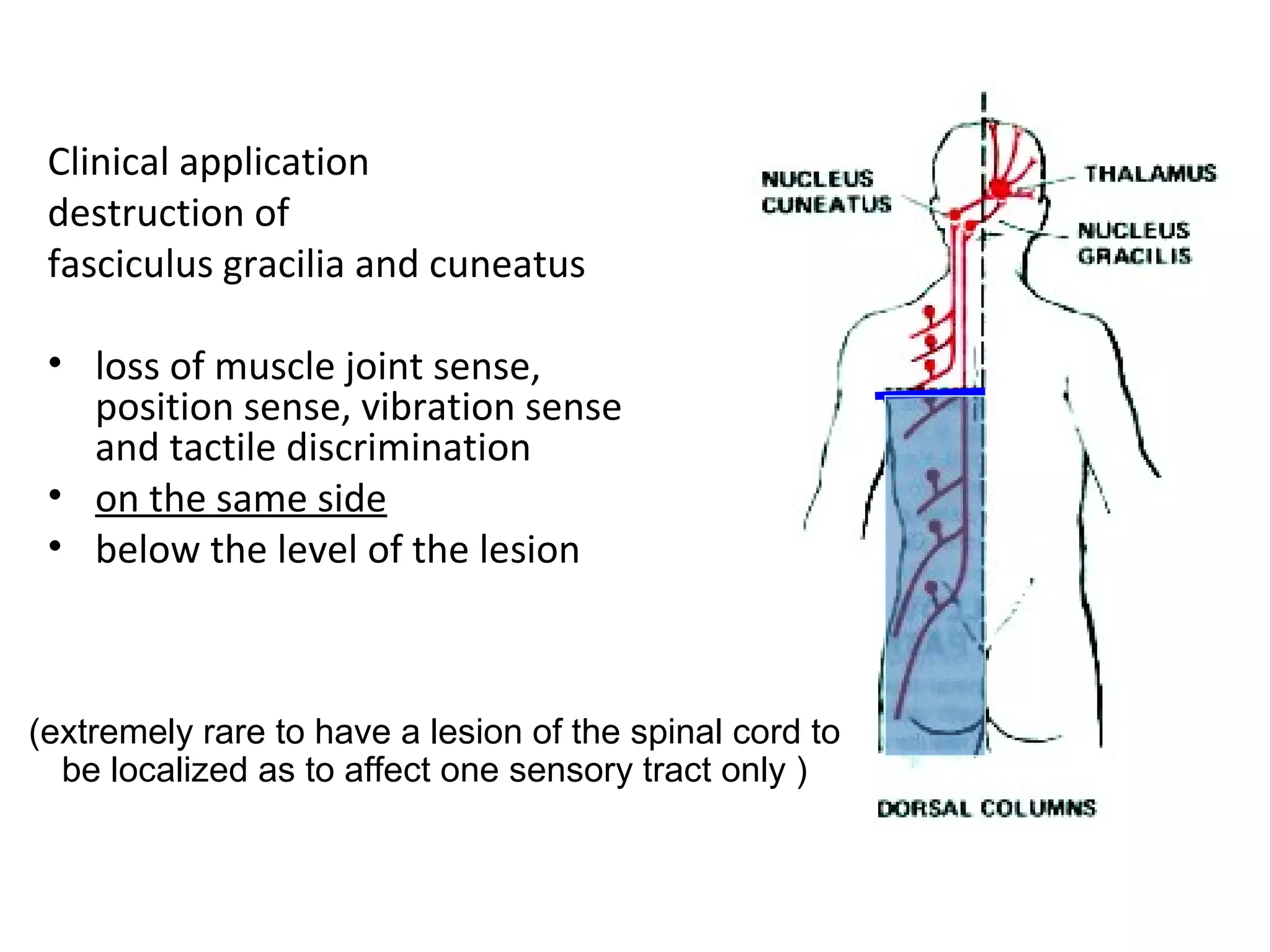
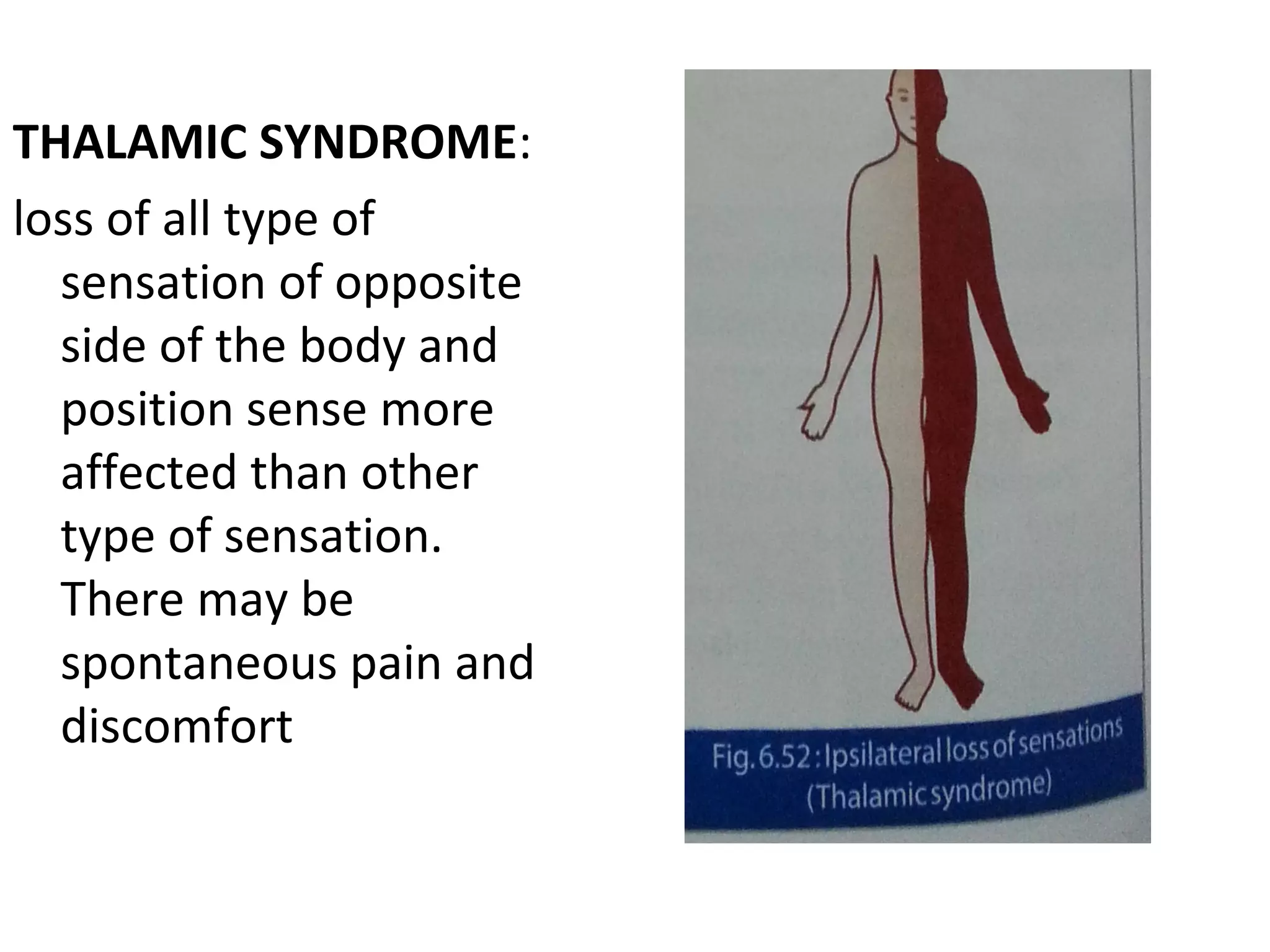
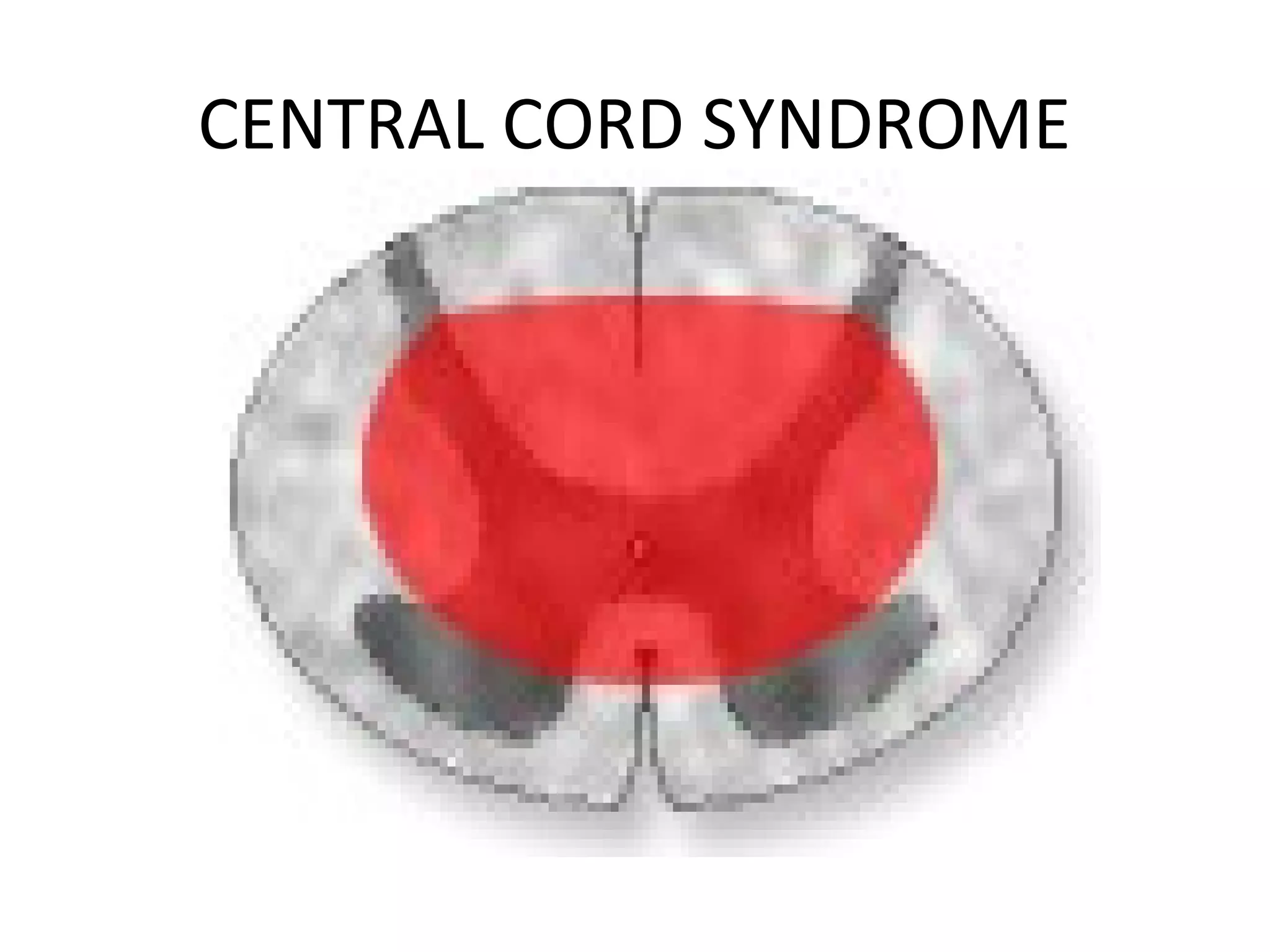
3) Common lesions that affect sensory pathways and how they impact sensation, such as hemisection of the spinal cord or damage to











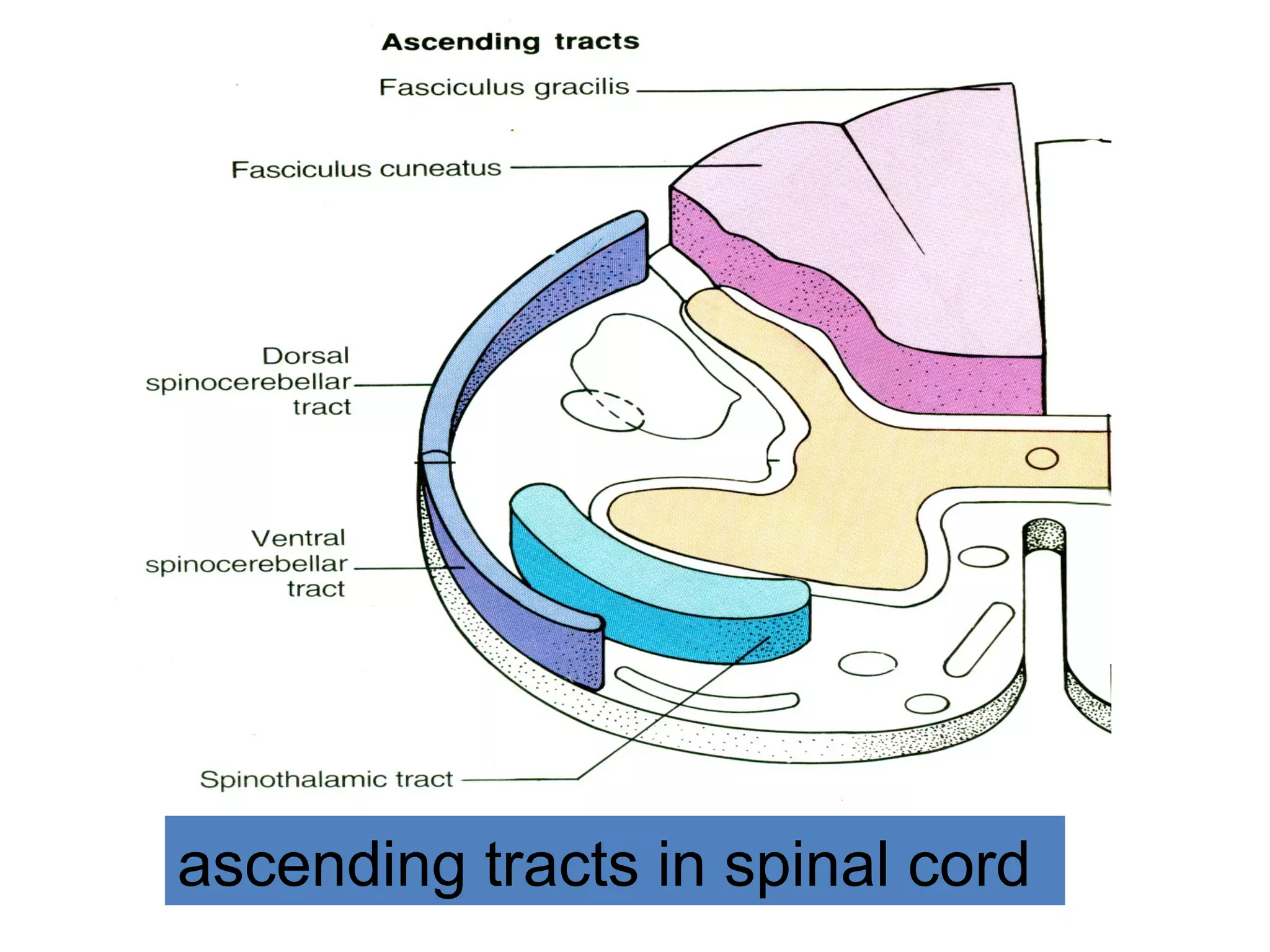





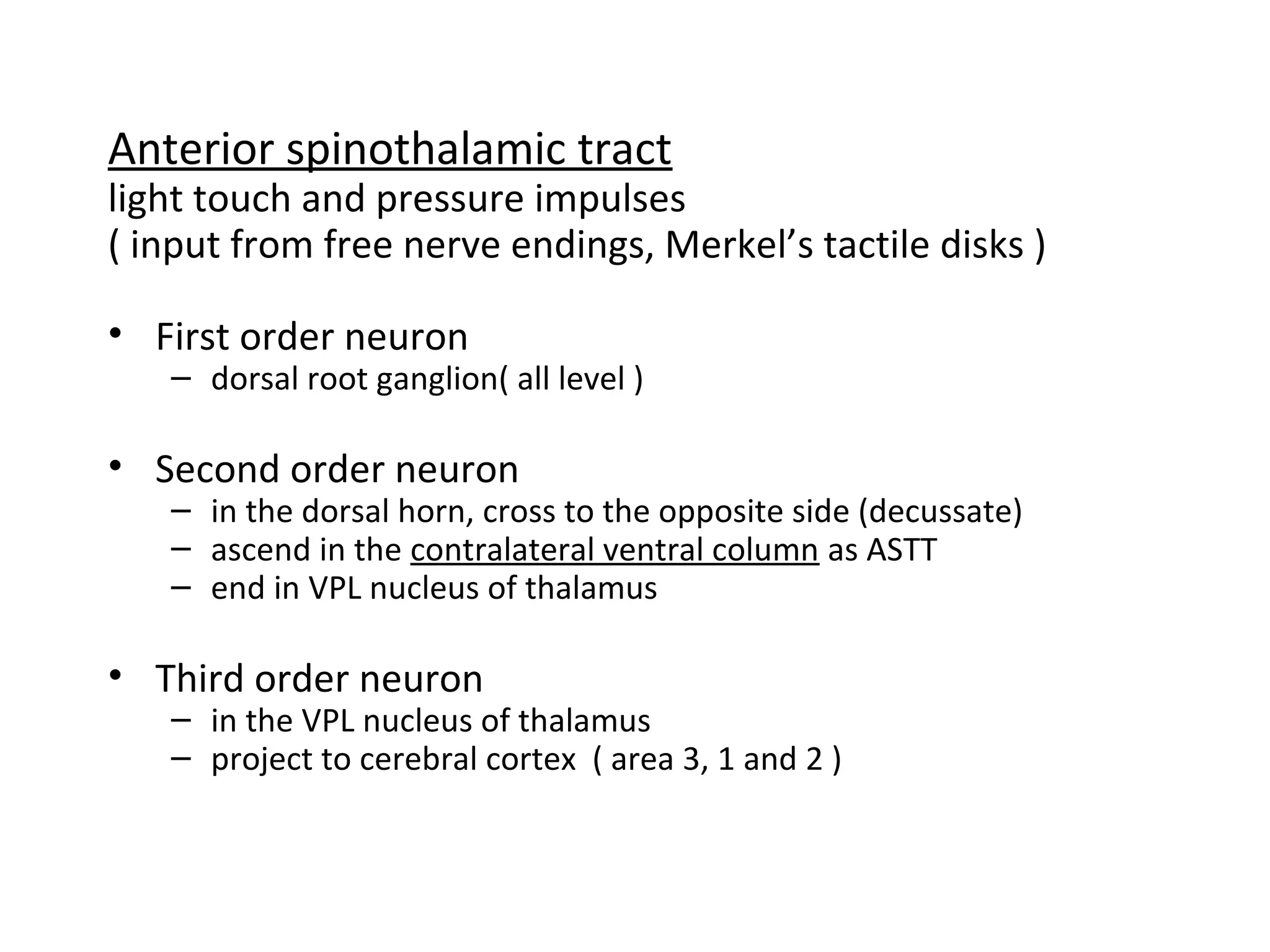



![lower 6 thoracic segments
lumbar segments
sacral segments
cervical segments
upper 6 thoracic segments
fasciculus gracilis
fasciculus cuneatus
[ nucleus G & C ]
in medulla
G
C](https://image.slidesharecdn.com/sensorysystem-171220190401/75/Sensory-system-34-2048.jpg)