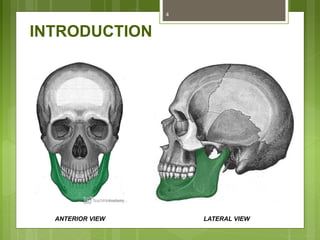
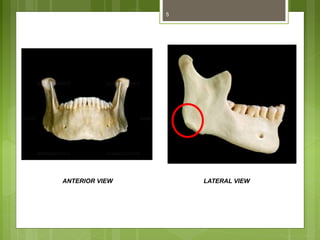
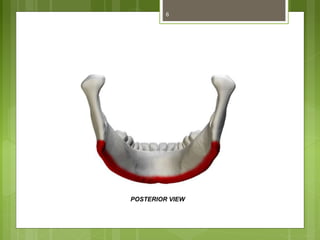
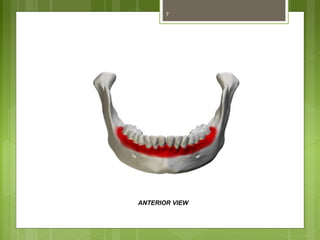
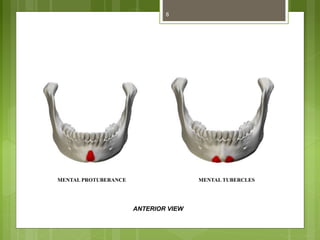
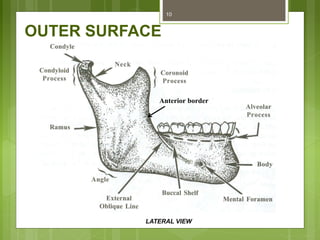
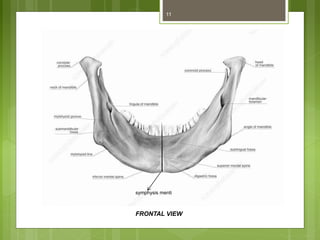
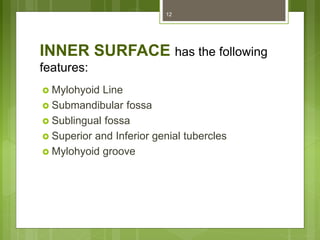
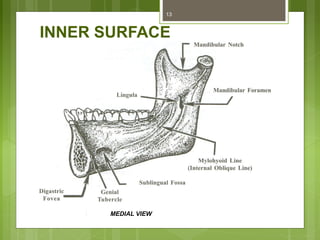
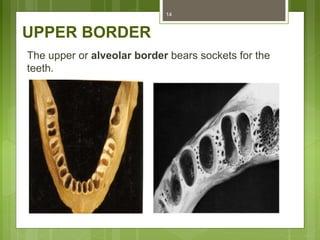
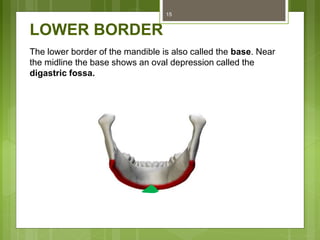
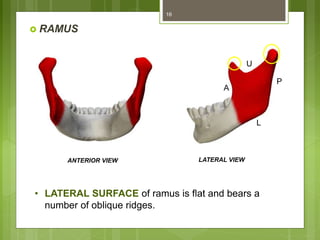
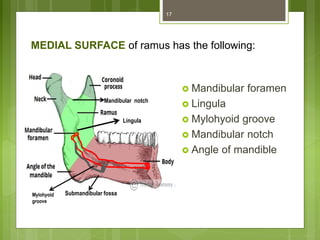
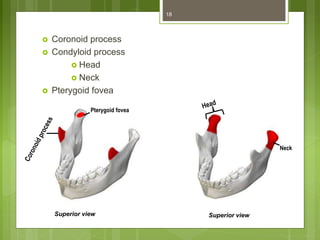
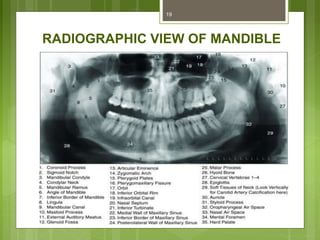
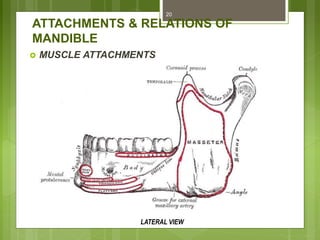
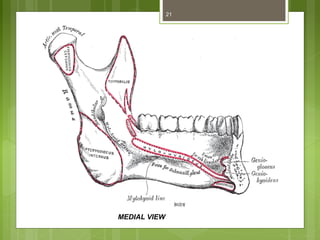
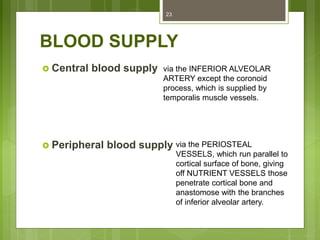
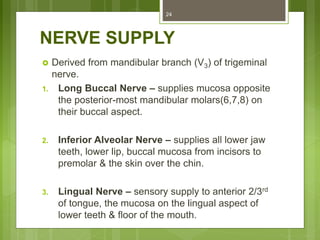
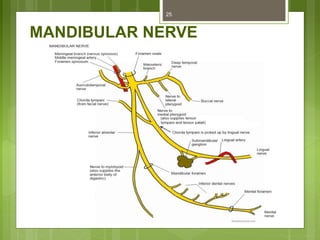
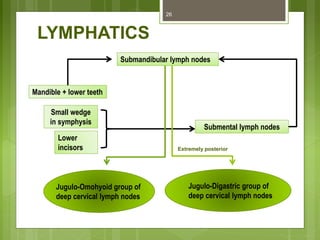
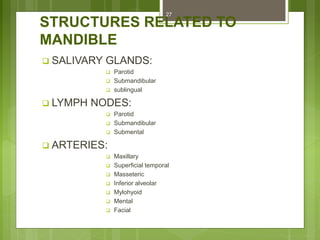
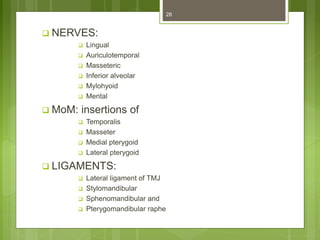
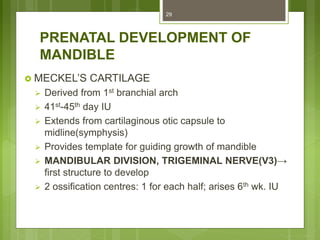
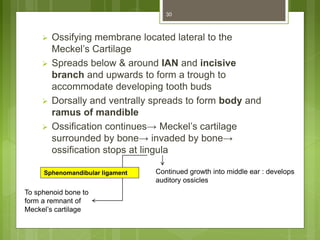
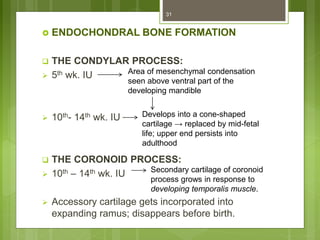
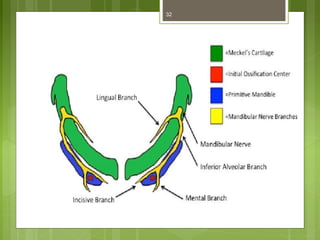
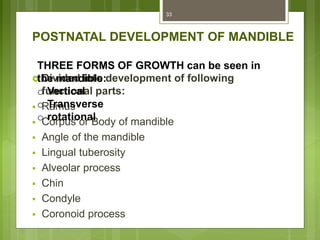
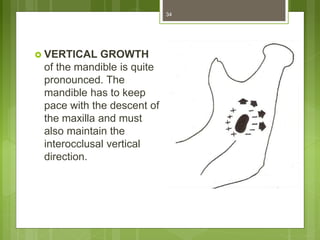
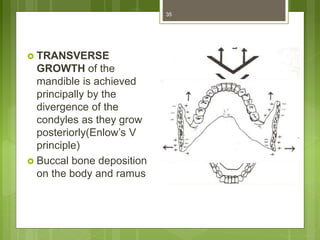
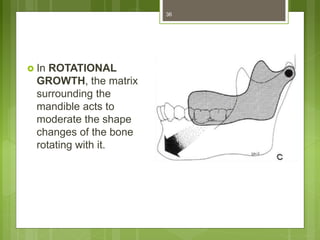
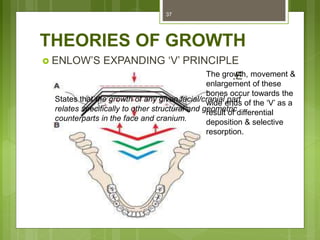
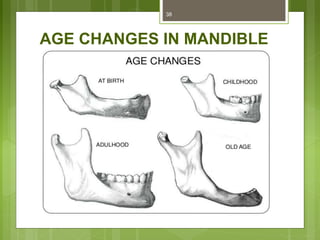
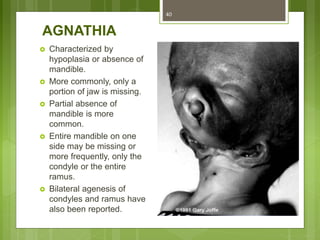
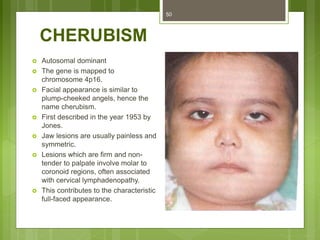
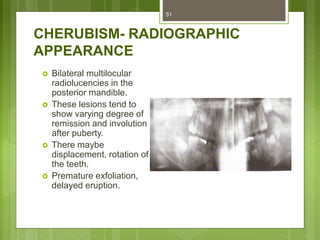
This document provides an overview of the mandible, including its anatomy, development, growth, age-related changes, and anatomical considerations. It describes the mandible's body, ramus, coronoid process, condylar process, attachments, foramina, blood supply, and related structures. It discusses the mandible's prenatal development from Meckel's cartilage and endochondral bone formation. It also addresses the postnatal development and growth of the mandible's various parts, as well as theories of mandibular growth. Common anatomical variations and conditions involving the mandible are described.