This document discusses gingival enlargement and its classification and management. It begins by defining gingival enlargement and discussing its classification according to etiological factors, location, and degree. It then covers various indices used to measure gingival enlargement. The document discusses inflammatory enlargement, drug-induced gingival overgrowth, idiopathic enlargement, and enlargements associated with systemic diseases. Management techniques for different types of gingival enlargement such as scaling, surgery, and changing medications are presented.



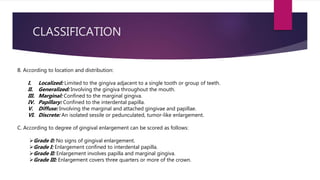


![INDICES
VERTICAL GINGIVAL OVERGROWTH INDEX
[GOI] :
- Originally described by Angelopoulos & Goaz
(1972) & later modified by Miller & Damm
(1992)
- Measures the overgrowth/ht. of gingival
tissues vertically in apico-coronal direction
from CEJ line to free gingival margin.
- The index grades the ht. of enlarged gingiva
covering the clinical crown & the non-visible
crown surface at 6 points around each tooth
acc. to following criterion----
VALUE INFERENCE
0 Normal gingiva
1 Slight, <2 mm increase &
gingiva covering the cervical
1/3 or less of anatomic
crown
2 Moderate, 2-4 mm increase
&/or gingiva extended upto
the middle 1/3 of the clinical
crown
3 Severe, >4 mm increase &/or
gingiva covering more than
2/3 of the clinical crown](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-9-320.jpg)










![ GINGIVAL CHANGES ASSOCIATED WITH MOUTH
BREATHING
- Gingivitis and gingival enlargement are often seen in mouth breathers.
[LITE et al., 1955]
- maxillary anterior region
- red and edematous gingiva
- diffuse surface shininess of the exposed area.
- clearly demarcated from the adjacent unexposed normal gingiva.
- ETIOLOGY : irritation from surface dehydration.
Klingsberg et al., 1961
INFLAMMATORY ENLARGEMENT due to
gingivitis](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-20-320.jpg)


![[BHARTI et al., 2013]](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-23-320.jpg)

![ PHENYTOIN (Anticonvulsant)
- 1st incidence of DIGO: viz., HYDANTOIN used to treat all forms of epilepsy except petit mal. [GLICKMAN et al., 1941]
- Ethotoin [PAGANONE], Mephenytoin [MESANTOIN], ZERONTIN, CELONTIN, DEPAKENE
- Rate of incidence of DIGO = ~50% patients [SEYMOUR et al., 1996]
- Younger patients
- Phenytoin appears in the saliva
- MODE OF ACTION:
- Phenytoin ↠
- May result from genetically determined ability or inability of the host to deal effectively with prolonged administration of phenytoin. [HASSEL & PAGE, 1994]
DRUG-INDUCED GINGIVAL
OVERGROWTH (DIGO)
↑ 𝑛𝑜. 𝑜𝑓 fibroblast-like cells and epithelium
↓
↑ synthesis of sulfated glycosaminoglycans (𝑖𝑛 𝑣𝑖𝑡𝑟𝑜)
++↓
↓ collagen degradation
production of inactive fibroblastic collagenase
↓](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-25-320.jpg)

![ PHENYTOIN (Anticonvulsant)
- HISTOPATHOLOGY:
- Hyperplasia and acanthosis of the epithelium
- Densely collagenous connective tissue
- Inflammation in the area adjacent to the gingival sulcus (pocket).
- Extension of deep rete pegs into the connective tissue.
- Increase in the number of fibroblasts and new blood vessels.
- Abundant amorphous ground substance.
- Oxytalan fibers are numerous beneath the epithelium and in areas of inflammation.
- “Mature” phenytoin enlargement-- fibroblast/ collagen ratio equal to that of normal
gingiva
- Recurring phenytoin enlargements-- appear as granulation tissue composed of
young capillaries and fibroblasts and irregularly arranged collagen fibrils with occasional
lymphocytes.
-
DRUG-INDUCED GINGIVAL
OVERGROWTH (DIGO)
ALTERNATIVE TO PHENYTOIN: Valproic acid
- broad spectrum of action
- effective on all forms of absence spells (simple as well as complex)
- useful as an adjunctive therapy for other seizures types when they occur in conjunction with absence spells
- more effective in the generalized than in the partial epilepsies– requires adjunct therapy with primidone to maintain a broad coverage.
- Side effects: transient gastric complaints, weight gain, occasional transient thinning of hair and rare mild thrombocytopenia.
- plasma half-life (8-15 hours) is shorter than phenytoin (13-24 hours)
- may increase the plasma concentration of phenobarbital 30 to 40% which produces ↑sedation
- can displace phenytoin from protein binding sites and provide toxic tissue levels despite measured therapeutic blood levels.
In the process of changing medications from phenytoin to valproic acid, a worsening of hyperplasia might be misconstrued as a direct effect of
valproic acid on the hyperplastic tissue.
- MANAGEMENT OF PHENYTOIN-INDUCED DIGO:
A discontinuation of phenytoin should not be recommended simply on the basis of moderate to severe hyperplasia.
Conservative periodontal measures include vigorous gingival massage coupled with efficient toothbrushing and gum stimulators.[BARATIERI,
1967]
When surgical measures are indicated, the drug treatment plan of the physician managing the epilepsy should be discussed and the date of
surgery postponed if the physician is planning to discontinue the phenytoin.
[Reynolds & Kirkham, 1980]](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-27-320.jpg)
![ Calcium Channel Blockers
- drugs developed for the treatment of cardiovascular conditions
(hypertension, angina pectoris, coronary artery spasms, and cardiac
arrhythmias.
- Prevalence is highly variable: 6- 83% [SLAVIN et al., 1987]
- CLINICAL FEATURES:
- Affects interdental papillae
- GO limited to marginal and attached gingiva
- Typically presents on anterior region
- Nifedipine-induced GO can coexist with periodontitis– different from other
forms of DIGO
- Nifedipine is also used with cyclosporine in kidney transplant recipients,
the combined use of both drugs induces larger overgrowths. [BÖKENKAMP
et al., 1994]
DRUG-INDUCED GINGIVAL
OVERGROWTH (DIGO)
• AMLODIPINE
• NIFEDIPINE
• NICARDIPINE
• FELODIPINE
• NITRENDIPINE
• DILTIAZEM
• VERAPAMIL](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-28-320.jpg)
![ Calcium channel blockers
- MECHANISM OF ACTION:
DRUG-INDUCED GINGIVAL
OVERGROWTH (DIGO)
NON-INFLAMMATORY PATHWAY INFLAMMATORY PATHWAY
- ↓ uptake of folic acid
- blockage of aldosterone
synthesis in adrenal cortex
- feedback ↑ACTH level
- upregulation of keratinocyte
growth factor (KGF)
Defective collagenase activity
- ↑local concentration of drug in
GCF/bacterial plaque
- Upregulation of cytokines viz.,
TGF-β1
- Degradation of periodontal
tissues
Vertical growth of gingiva–
PSEUDOPOCKET formation
Calcium channel blocker-induced
DIGO
[LAFZI et al., 2006]](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-29-320.jpg)
![ Calcium channel blockers
- ALTERNATIVES FOR NIFEDIPINE/AMLODIPINE:
- ISRADIPINE– dihydropyridine derivative; can replace existing drugs for DIGO
- Does not induce gingival overgrowth [WESTBROOK et al., 1997]
DRUG-INDUCED GINGIVAL
OVERGROWTH (DIGO)](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-30-320.jpg)
![[SAMUDRALA et al., 2016]](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-31-320.jpg)
![ CYCLOSPORINE (Immunosuppressant)
- Potent immunosuppressive agent-- prevent organ transplant rejection and to treat several diseases of autoimmune origin
- 1st case reported– 1983 (HEFTI et al.)
- Cyclosporin A (Sandimmune, Neoral)– I.V. or p.o., and dosages >500 mg/day have been reported to induce gingival overgrowth. [DALEY,
1986]
- Cyclosporine-induced gingival enlargement is more vascularized than phenytoin enlargement
- occurrence varies according to different studies from 25% to 70%, [ROMITO, 2004]
- MECHANISM OF ACTION: Cyclosporine A
directly impairs collagen synthesis by gingival fibroblasts+ incr. levels of type I collagen
decreases expression of MMPs 1 and 3
leads to reduced metabolism of glycosaminoglycans
selectively and reversibly inhibit helper T cells, which play a role in cellular and humoral immune responses.
- In addition to gingival enlargement, cyclosporine induces other major side effects, such as nephrotoxicity, hypertension, and hypertrichosis.
DRUG-INDUCED GINGIVAL
OVERGROWTH (DIGO)](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-32-320.jpg)

![- HISTOPATHOLOGY:
- microscopic finding of many plasma cells
- abundant amorphous extracellular substance
- suggests that the enlargement is a hypersensitivity response to the
cyclosporine. [MARIANI et al., 1993]
- Thickened epithelium
- Formation of retepegs
- Irregular collagen formation
Another immunosuppressive drug, TACROLIMUS, has been used effectively and is also nephrotoxic, but it results in
much less severe hypertension, hypertrichosis, and gingival overgrowth. [SPENCER et al., 1997]
DRUG-INDUCED GINGIVAL
OVERGROWTH (DIGO)](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-34-320.jpg)
![[SAMUDRALA et al., 2016]](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-35-320.jpg)

![IDIOPATHIC GINGIVAL ENLARGEMENT
aka gingivomatosis, elephantiasis, idiopathic fibromatosis, hereditary gingival hyperplasia, and congenital familial fibromatosis
rare condition
undetermined cause
ETIOLOGY:
- Unknown
- hereditary basis [ZISKIN et al., 1943] but the genetic mechanisms involved are not well understood.
- mode of inheritance to be autosomal recessive in some cases and autosomal dominant in others [RAESTE et al, 1978]
CLINICAL FEATURES:
- Affects the attached gingiva, as well as the gingival margin and interdental papillae
- Affects the facial and lingual surfaces of the mandible and maxilla
- Involvement may be limited to either jaw
- The enlarged gingiva is pink, firm, and almost leathery in consistency and has a characteristic minutely pebbled surface
- Severe cases – teeth are almost completely covered, and the enlargement projects into the oral vestibule.
- The jaws appear distorted because of the bulbous enlargement of the gingiva.
- Secondary inflammatory changes are common at the gingival margin.](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-37-320.jpg)




![ PREGNANCY-ASSOCIATED GINGIVAL OVERGROWTH
- common pathology in pregnancy
- marginal and generalized
- single or multiple tumor-like masses
- ETIOLOGY:
Marginal Enlargement
- results from the aggravation of previous inflammation – does not occur without the presence of bacterial plaque
- clinical picture varies considerably-- usually generalized
- tends to be more prominent interproximally than on the facial and lingual surfaces
- bright red or magenta, soft, and friable and has a smooth, shiny surface.
- Bleeding occurs spontaneously or on slight provocation.
GO associated with SYSTEMIC CONDITIONS/
CONDITIONED ENLARGEMENT
- ↑ levels of PROGESTERONE (10x) and ESTROGEN (30x) by the end of the third trimester
- These hormonal changes induce changes in vascular permeability-- gingival edema, ↑ inflammatory response
to dental plaque.
- changes in subgingival microbiota -- ↑ Prevotella intermedia [RABER-DURLACHER et al., 1994]
Susceptibility to periodontal infection increases during early gestation due to:
- suppressed T-cell activity
- decreased neutrophil chemotaxis and phagocytosis
- altered lymphocyte response
- depressed antibody production
- chronic maternal stress
- down- regulation of IL-6 production, rendering the gingiva less efficient at resisting the
inflammatory challenges produced by the bacteria
- decreased levels of IgG](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-42-320.jpg)



![ PUBERTY- ASSOCIATED GINGIVAL OVERGROWTH
- occurs in both male and female adolescents – areas of plaque accumulation.
CLINICAL FEATURES:
- size of the gingival enlargement greatly exceeds that usually seen in association with
comparable local factors
- marginal and interdental
- characterized by prominent bulbous interproximal papillae
- Capnocytophaga and P. intermedia [MOMBELLI et al., 1990; WOJCICKI CJ, 1987]
- mechanical action of the tongue and the excursion of food prevent a heavy
accumulation of local irritants on the lingual surface.
- tendency to develop massive recurrence in the presence of relatively scant plaque
deposits
- undergoes spontaneous reduction but does not disappear until plaque and calculus
are removed.
GO associated with SYSTEMIC CONDITIONS/
CONDITIONED ENLARGEMENT
HISTOPATHOLOGY
- chronic inflammation
- prominent edema
- associated degenerative changes
MANAGEMENT
- Scaling and oral hygiene instructions.
- Surgical removal may be performed in severe cases.](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-46-320.jpg)






























![CONCLUSION
[AGRAWAL et al., 2015]](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-78-320.jpg)
![CONCLUSION
[BHATNAGAR et al., 2018]](https://image.slidesharecdn.com/10gingivalenlargementitsmgmt04420-200410195446/85/GINGIVAL-ENLARGEMENT-MGMT-79-320.jpg)

