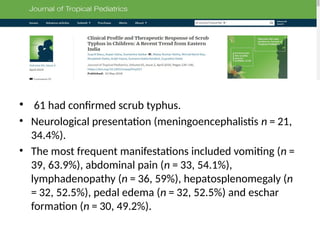
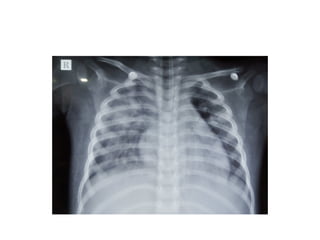
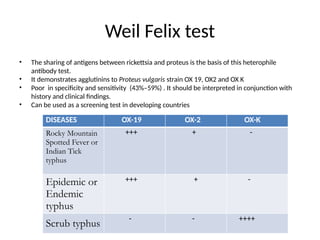
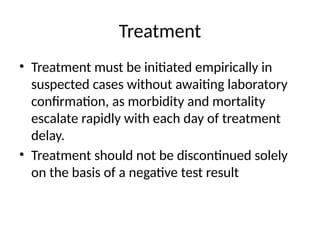
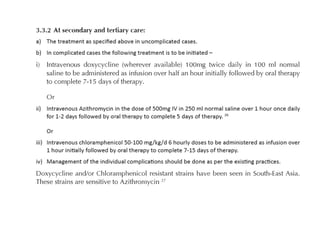
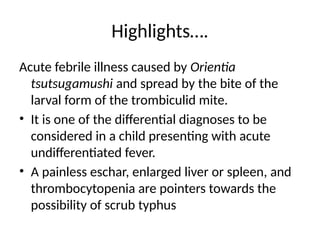
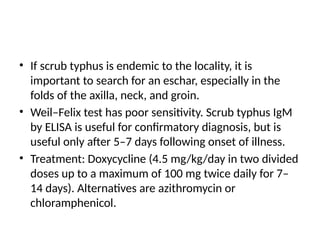
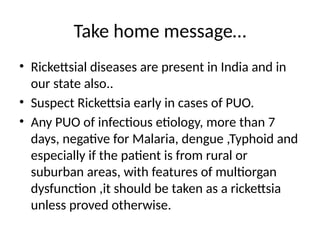
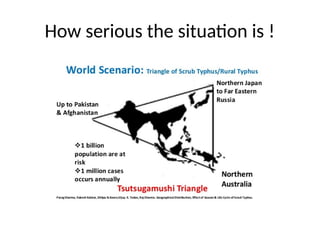
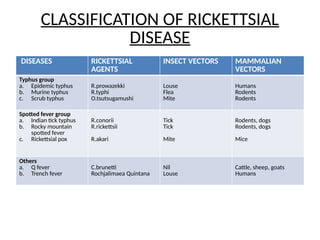
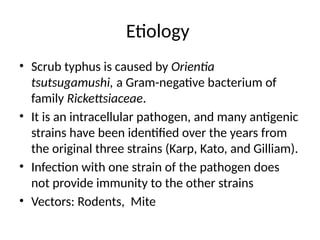
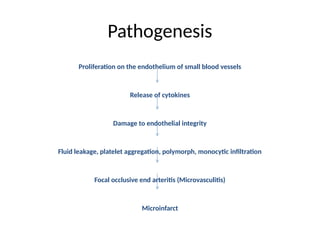
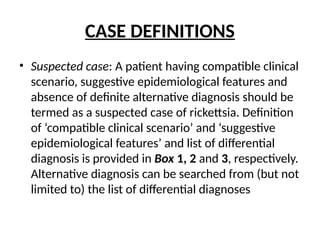
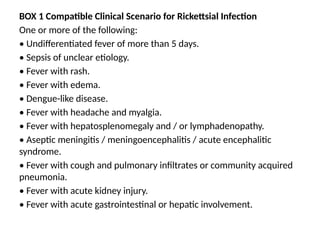
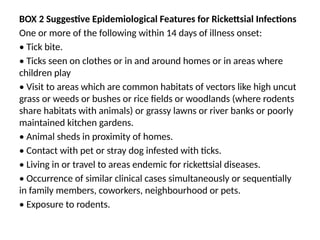
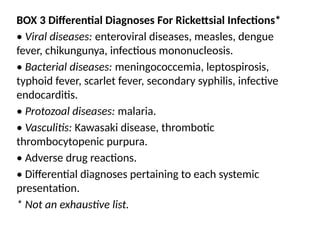
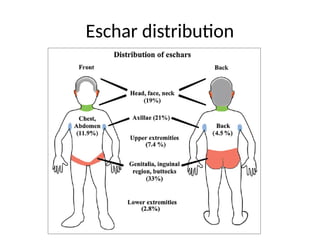
The document discusses rickettsial diseases, specifically focusing on scrub typhus, its etiology, clinical features, diagnostic criteria, and treatment protocols. It emphasizes the importance of early suspicion and empirical treatment to prevent complications, given the challenges in diagnosis due to varying laboratory availability in different regions. Key diagnostic indicators include symptoms like fever with rash, eschar presence, and epidemiological features related to vector exposure.
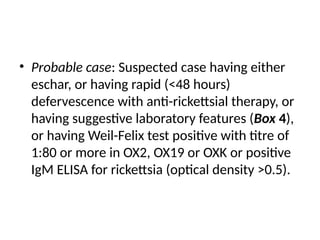
![• Confirmed case: Suspected case having
rickettsial DNA detected in whole blood or tissue
samples, or fourfold rise in antibody titres on
acute and convalescent sera detected by
immunofluorescence assay (IFA) or immuno-
peroxidase assay (IPA) [8]. In countries like India,
where PCR and IFA are not commonly available,
properly performed paired serological tests like
ELISA have high positive predictive value](https://image.slidesharecdn.com/wbiapscrub-241204093937-78d2fd61/85/Scrub-typhus-or-Lousy-Problem-in-Children-pptx-13-320.jpg)