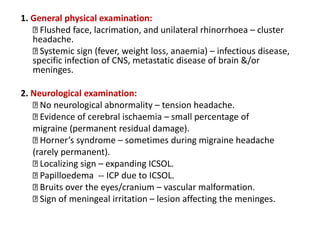
This document provides information on different types of headaches, including their causes, symptoms, and characteristics. It discusses primary headaches like tension headaches, which most commonly affect women, and migraines, which often affect younger females. It also covers secondary headaches that can result from issues like infections, head injuries, or vascular disorders. Specific headache types like clusters headaches that predominantly impact adolescent males are also outlined. The document details factors like headache location, duration, frequency, and associated symptoms that can provide clues to determining the underlying headache type and cause.















![• Brain tumours / raised ICP: headaches that disturb sleep/ early
morning headaches
• Early morning headache on waking up and again at the end of day is
due to Maxillary sinusitis (diurnal variation)
• Office headache: due to Frontal sinusitis [patient wakes up mostly
without pain due to overnight drainage, develops pain after a few
hours that lasts throughout the day]
• Vacuum headache: the headache on waking up that may occur in
Frontal sinusitis due to over night drainage.](https://image.slidesharecdn.com/headache-191026210610/85/Headache-17-320.jpg)