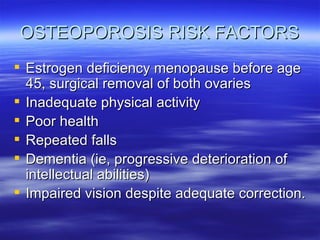
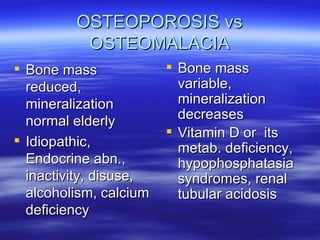
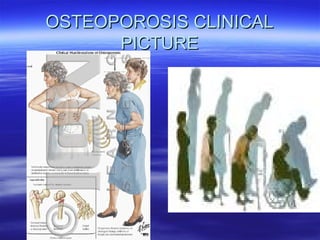
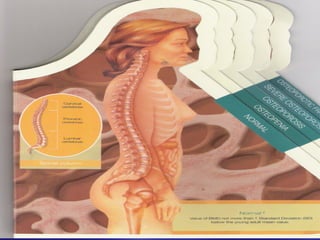
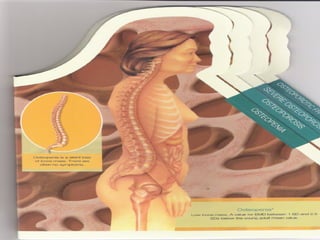
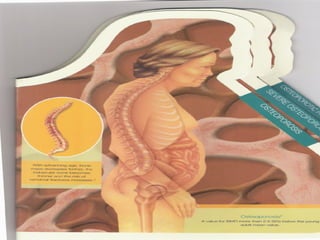
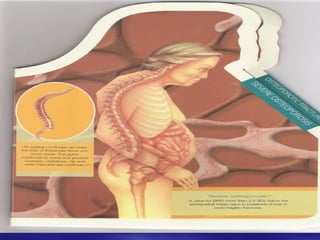
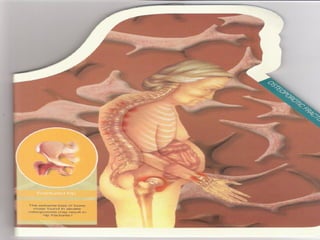
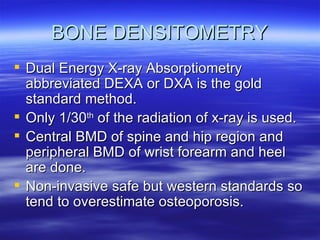
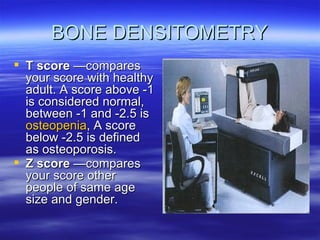
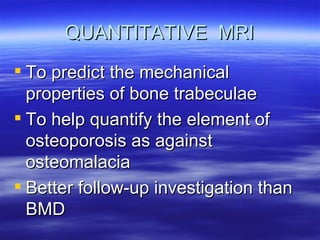
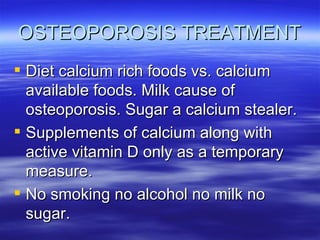
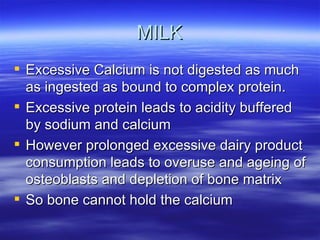
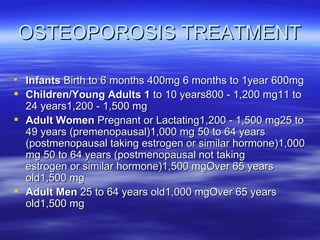
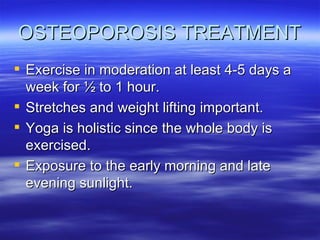
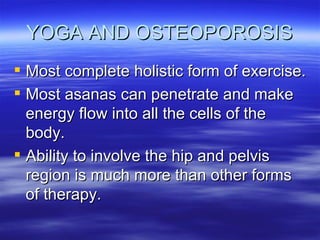
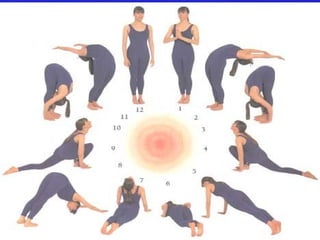
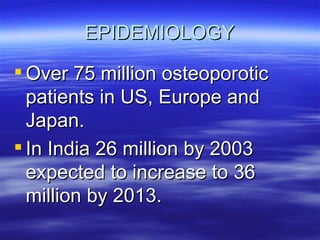
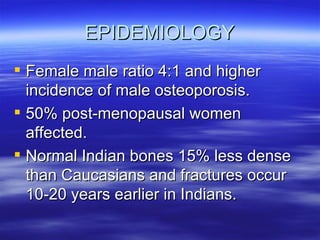
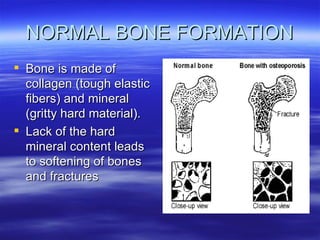
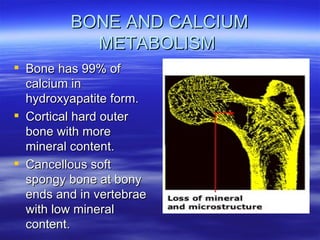
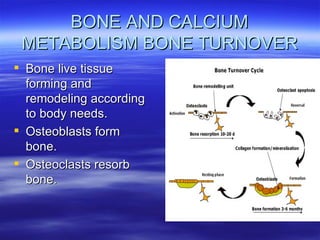
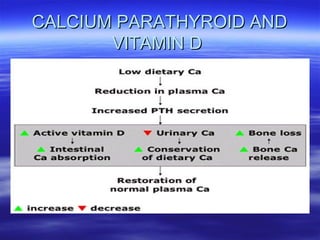
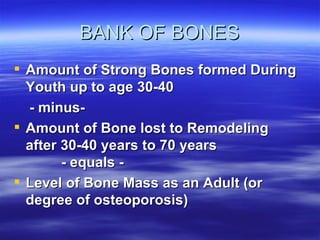
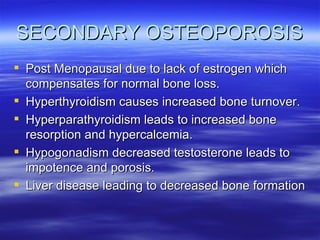
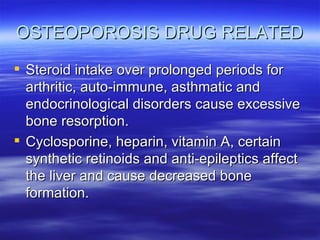
Osteoporosis is a bone disorder characterized by low bone density and mass, leading to an increased risk of fractures. It is a growing epidemic, with over 75 million cases in the US, Europe and Japan expected to increase further. Risk factors include age, gender, family history, lifestyle factors like smoking, sedentary lifestyle, and certain medical conditions or medications. Diagnosis involves clinical evaluation, bone density scans, and biochemical markers. Treatment focuses on lifestyle changes like exercise, calcium intake, and vitamin D; medications include hormones, biphosphonates, and teriparatide injections in severe cases. Preventing osteoporosis requires modifiable lifestyle changes and responsible self-care.
![OSTEOPOROSIS RISK FACTORS History of fracture as an adult and in an immediate (first-degree) relative Low body weight (less than 127 lb [58 kg]) or weight loss Lifelong low calcium intake Current cigarette smoking Alcoholism Advanced age](https://image.slidesharecdn.com/osteoporosis-1231837262836417-3/85/Osteoporosis-13-320.jpg)