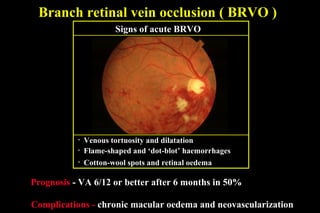
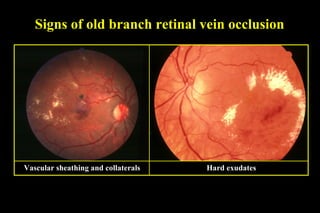
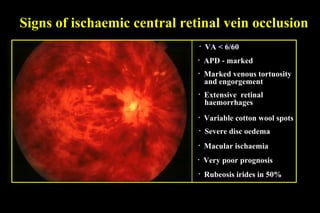
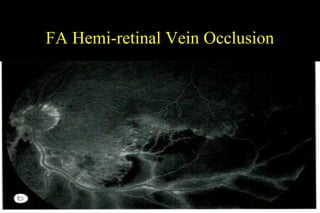
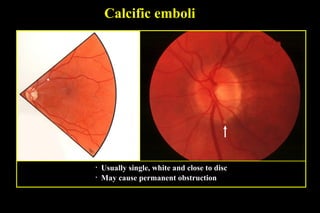
Retinal vascular occlusions can be retinal vein occlusions such as branch, central, or hemi-retinal vein occlusions or retinal artery occlusions such as branch, cilio-retinal, hemi-retinal, or central artery occlusions. Branch retinal vein occlusions are the most common type and present with flame-shaped and dot-blot hemorrhages, cotton-wool spots, and retinal edema. Central retinal vein occlusions can be non-ischemic or ischemic depending on retinal perfusion and have varying prognoses depending on vision outcome and complications. Retinal artery occlusions generally have a poorer prognosis and can be caused by emboli, presenting with retinal whitening and arteriolar