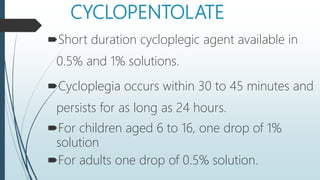
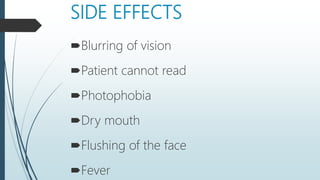
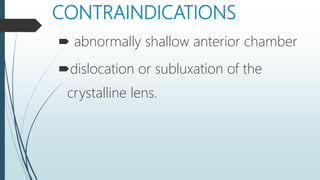
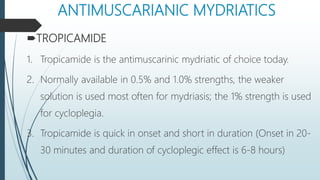
This document discusses ophthalmic diagnostic medications including cycloplegics, mydriatics, and anesthetics. Cycloplegics paralyze the ciliary muscle to induce cycloplegia for examinations and treatments requiring loss of accommodation. Common cycloplegics are atropine, cyclopentolate, and tropicamide. Mydriatics dilate the pupil for fundus exams using antimuscarinic drugs like tropicamide or sympathomimetics like phenylephrine. Anesthetics like proparacaine, benoxinate, and tetracaine are used to numb the eye during procedures.