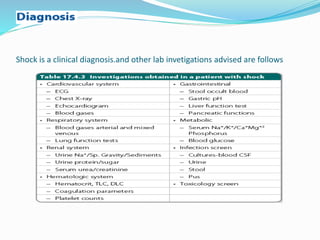
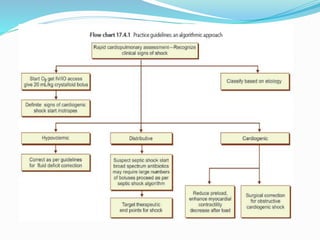
This document discusses shock in children, defining it as impaired tissue perfusion resulting from an imbalance between oxygen demand and supply. Shock can be classified as hypovolemic, cardiogenic, or distributive based on the underlying cause. Signs of shock in children may be more subtle than in adults since children can maintain blood pressure through compensatory mechanisms even as tissue perfusion decreases. Early signs include tachycardia and signs of poor peripheral perfusion rather than hypotension. Management involves rapid fluid resuscitation and vasoactive drugs to support circulation as needed based on the type of shock present. The goal is to restore adequate organ perfusion and oxygen delivery.