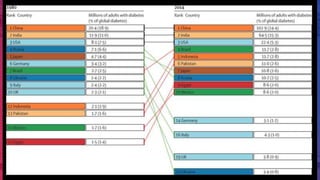
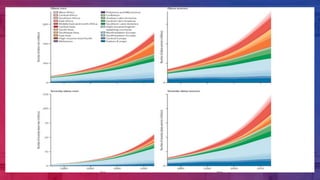
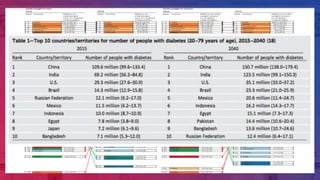
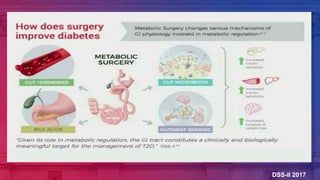
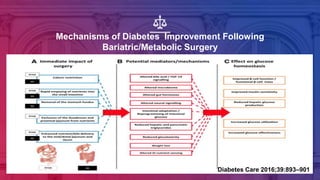
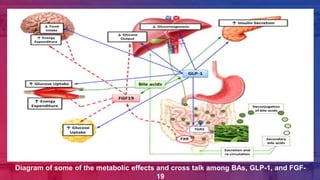
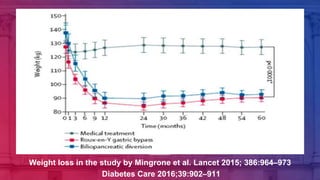
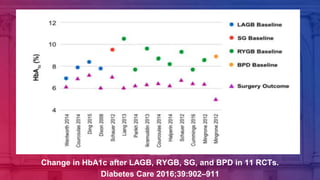
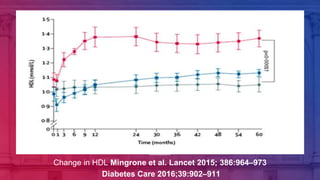
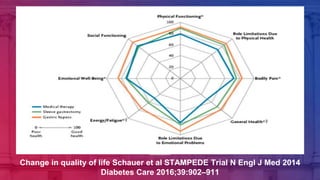
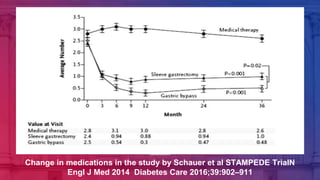
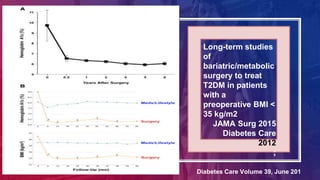
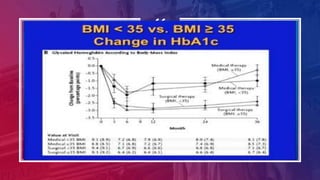
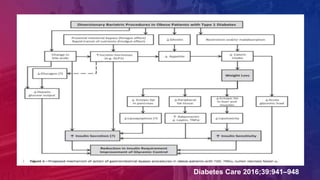
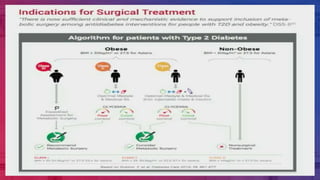
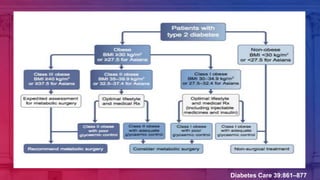
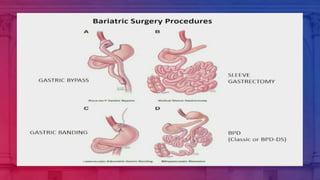
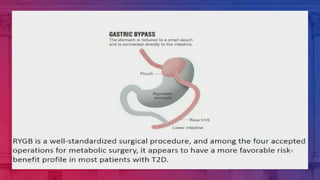
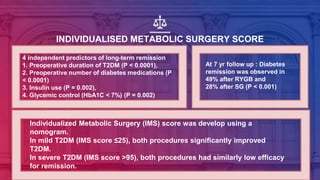
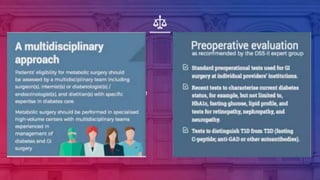
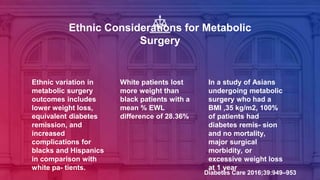
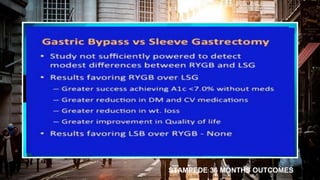
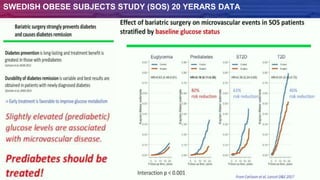
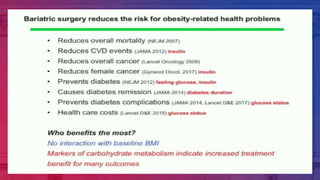
The document discusses metabolic surgery as a treatment for type 2 diabetes. It notes that gastric bypass surgery was found to result in diabetes remission in 78% of patients in early studies. This catalyzed research into the mechanisms by which bariatric surgery improves glucose control. Worldwide obesity and diabetes prevalence is increasing significantly. Metabolic surgery is the most effective means of substantial and durable weight loss, and results in better glycemic control and reduced cardiovascular risk factors compared to medical therapy alone. The mechanisms of diabetes improvement after surgery extend beyond just weight loss and include effects on incretin hormones, insulin secretion, and insulin sensitivity.