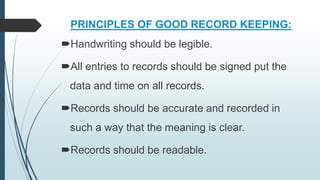
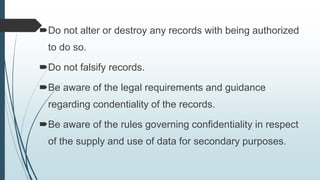
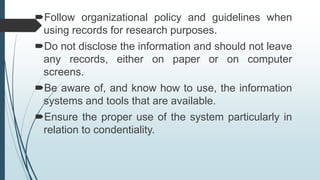
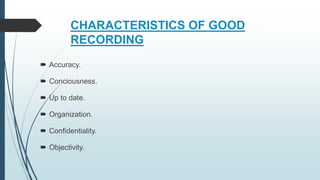
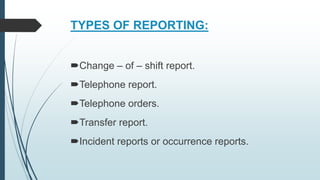
The document discusses nursing records and reports. It defines records as written documentation used for specific purposes that permanently documents patient care information. Reports are defined as oral, written, or computer-based communications intended to convey information. Accurate documentation is important for patient care and treatment. Records must be accurate, complete, confidential, and timely. Effective reporting includes accuracy, organization, and confidentiality. The roles, types, purposes, and principles of nursing records and reports are explained.