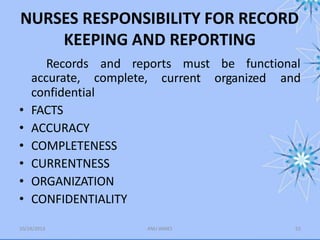
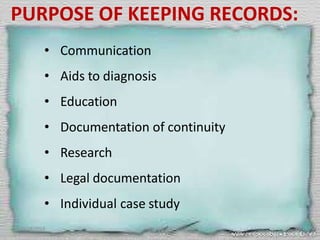
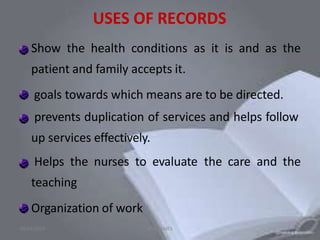
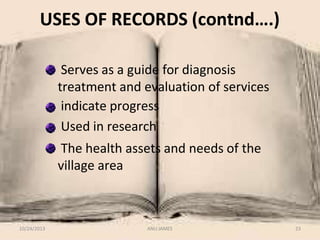
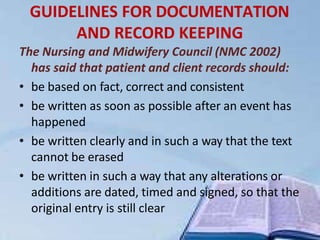
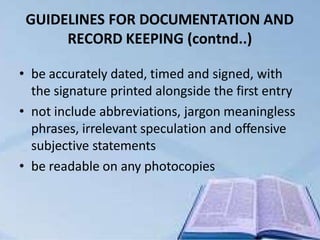
The document outlines 14 principles of documentation for nursing records: 1) Date and time, 2) Legibility, 3) Correct spelling, 4) Permanence, 5) Accepted terminology, 6) Factual, 7) Accurate, 8) Appropriateness, 9) Completeness, 10) Current, 11) Conciseness, 12) Organized, 13) Signature, and 14) Confidentiality. It also describes different types of records including patient clinical records, individual staff records, ward records, and administrative records. The purposes of record keeping are also discussed.


![DEFINITION:
◾ Records the memory of the internal and external
transactions of an organization. Records contain a
written evidence of the activities of an organization in
the form of letters, circulars, reports, contracts,
invoices, vouchers, minutes of meeting, books of
account etc.
[S.L.Geol, 2001 ]
1
2](https://image.slidesharecdn.com/recordsandreports-230608100640-eba50016/85/records-and-reports-pptx-12-320.jpg)
![◾ It is a written communication that
permanently documents information relevant
to a client’s health care management. It is a
continuing account of the client’s health care
needs
[Sr. Mary lucita ]
1
3](https://image.slidesharecdn.com/recordsandreports-230608100640-eba50016/85/records-and-reports-pptx-13-320.jpg)
![DEFINITION
A report containing information
against in a narrative graphic or tabular
form, prepared on periodic, receiving,
regular or as a required basis. Reports may
refer to specific periods, events,
10/24/2013 ANU JAMES 43
occurrence, or subject and may be
oral or
communicated or presented in
written form
[ Basvanthappa bt.2009 ]](https://image.slidesharecdn.com/recordsandreports-230608100640-eba50016/85/records-and-reports-pptx-43-320.jpg)
![DEFINITION (contnd..)
10/24/2013 ANU JAMES 44
Reports are oral or written
exchanges of information shared between
care givers of workers in a number of ways.
A report summarises the service of the
personnel and of the agency
[ Jean b. 2002 ]](https://image.slidesharecdn.com/recordsandreports-230608100640-eba50016/85/records-and-reports-pptx-44-320.jpg)