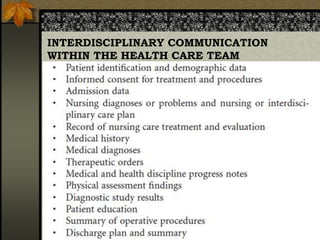
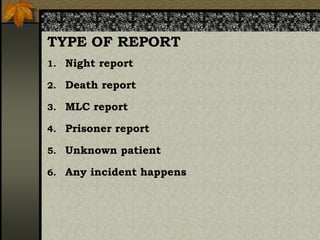
This document outlines the importance of documentation in nursing, emphasizing the need for accurate, comprehensive, and organized records to ensure continuity of care and track patient outcomes. It discusses the challenges of documentation, the principles of record writing, and the purposes of both records and reports in healthcare. Additionally, it provides guidelines for quality documentation and reporting, highlighting their roles in effective communication within the healthcare team.