This document discusses iron deficiency anemia (IDA), including:
1. Iron is an important bioactive element involved in oxygen transport, oxidative metabolism, and cellular growth. The majority of iron is found in hemoglobin and myoglobin, with smaller amounts in various enzymes.
2. Iron is absorbed in the small intestine and transported by transferrin in plasma. It is stored in ferritin and hemosiderin. Iron requirements vary between men and women.
3. IDA is common and caused by low dietary iron intake, increased demands, blood loss, or malabsorption. Common causes of blood loss include gastrointestinal issues, menstruation, and pulmonary or urinary problems.
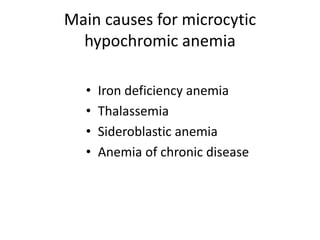
4.