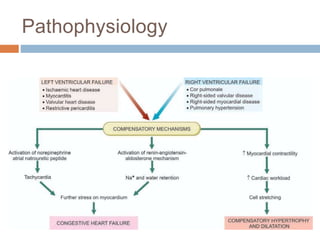
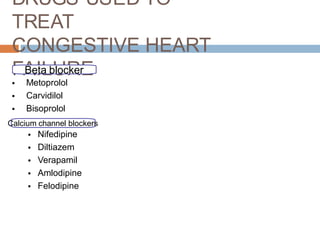
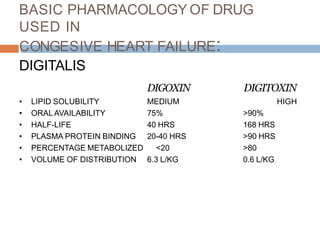
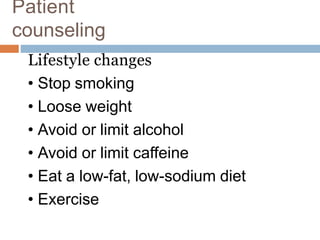
Congestive heart failure occurs when the heart muscle is weakened and cannot pump blood strongly, reducing oxygen delivery to organs and tissues. It can result from conditions that damage the heart muscle or overwork the heart. Symptoms include shortness of breath, fatigue, swelling, and cough. Treatment focuses on managing symptoms with medications like ACE inhibitors, beta-blockers, diuretics, and lifestyle changes including diet, exercise, stress reduction, and fluid intake limits. Making adjustments based on monitoring for changes is important for patient counseling in congestive heart failure management.