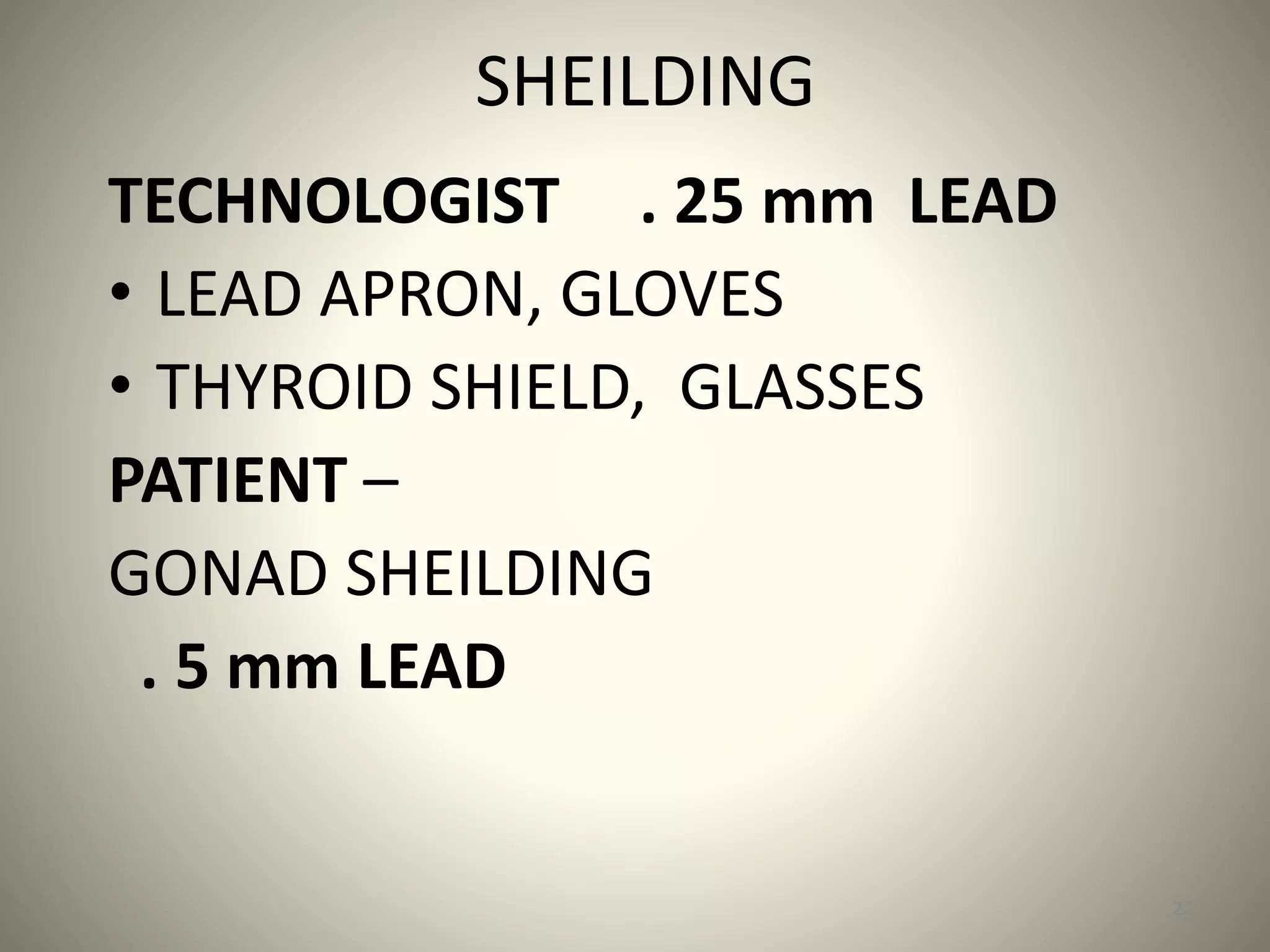
This document discusses radiation protection for medical workers. It explains that radiologists, radiographers and other medical staff are subject to some radiation exposure through their work, so radiation protection aims to keep doses as low as possible to prevent health risks. It describes different types of radiation effects and dose limits for workers. Various methods of radiation monitoring are outlined, including use of dosimeters like film badges, pocket ionization chambers and thermoluminescent dosimeters to measure individual radiation exposures.