1) Managing patient radiation dose involves controlling medical equipment settings and imaging procedures to limit unnecessary radiation exposure.
2) Common metrics for estimating patient radiation dose include entrance skin exposure, bone marrow dose, and gonadal dose. Entrance skin exposure is widely used due to ease of measurement.
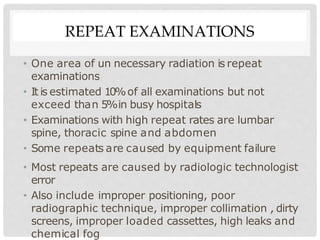
3) Reducing unnecessary radiation can be achieved by restricting unnecessary examinations, using proper technique like higher kVp settings, collimation, and shielding of sensitive areas. Repeated examinations and errors should be minimized.