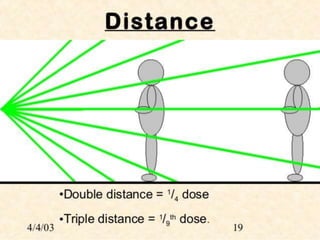
Radiation protection methods are necessary to prevent harmful effects of ionizing radiation exposure. The key methods discussed are: 1) increasing distance from the radiation source to reduce exposure, 2) using protective barriers like aprons and gloves between the body and radiation, and 3) employing principles like reducing unnecessary exposures, proper beam filtration, radiation monitoring, and following ALARA to maintain radiation exposures as low as reasonably achievable. Radiation can damage DNA and create free radicals leading to biological effects so proper safety protocols are important.