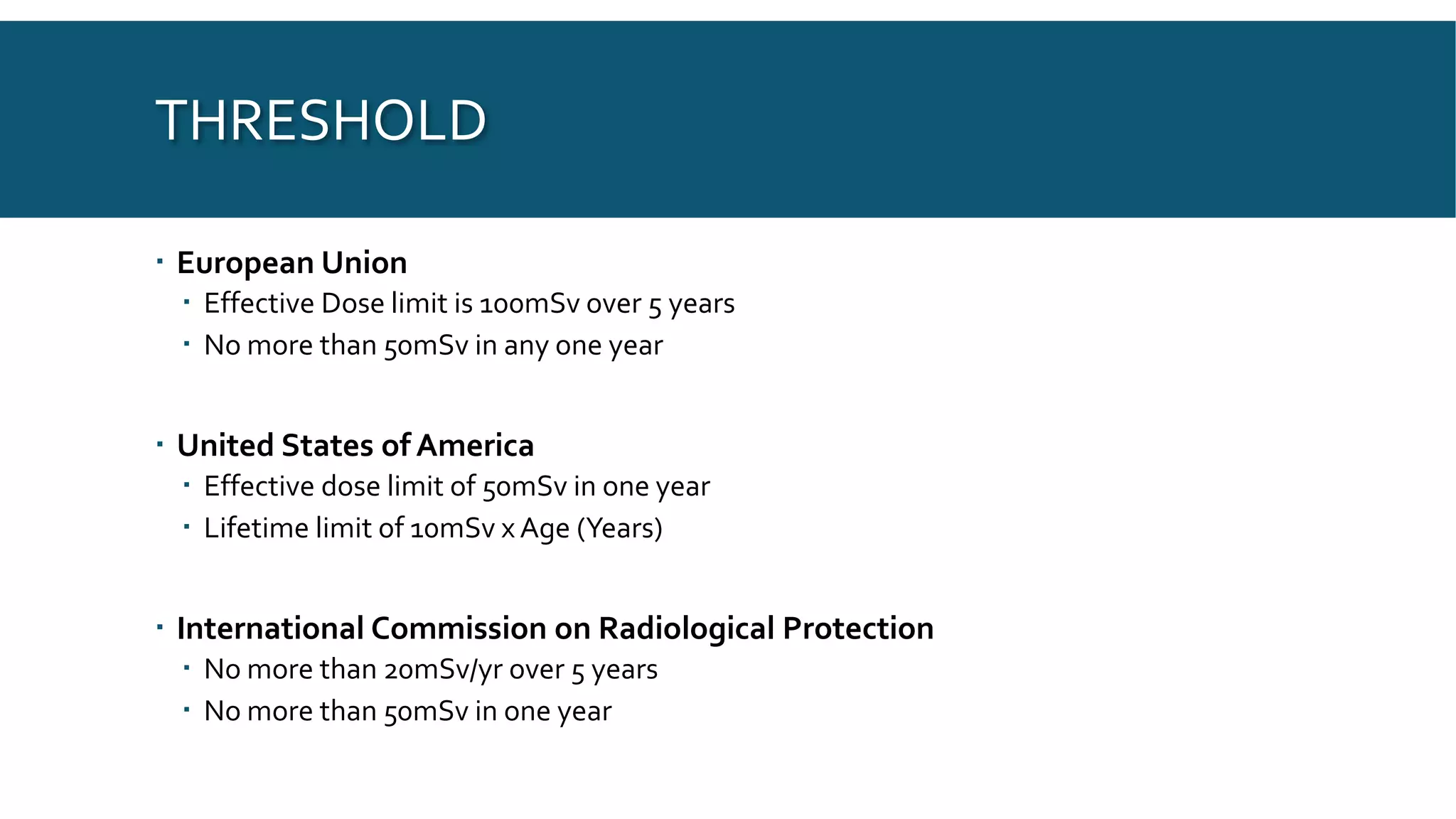
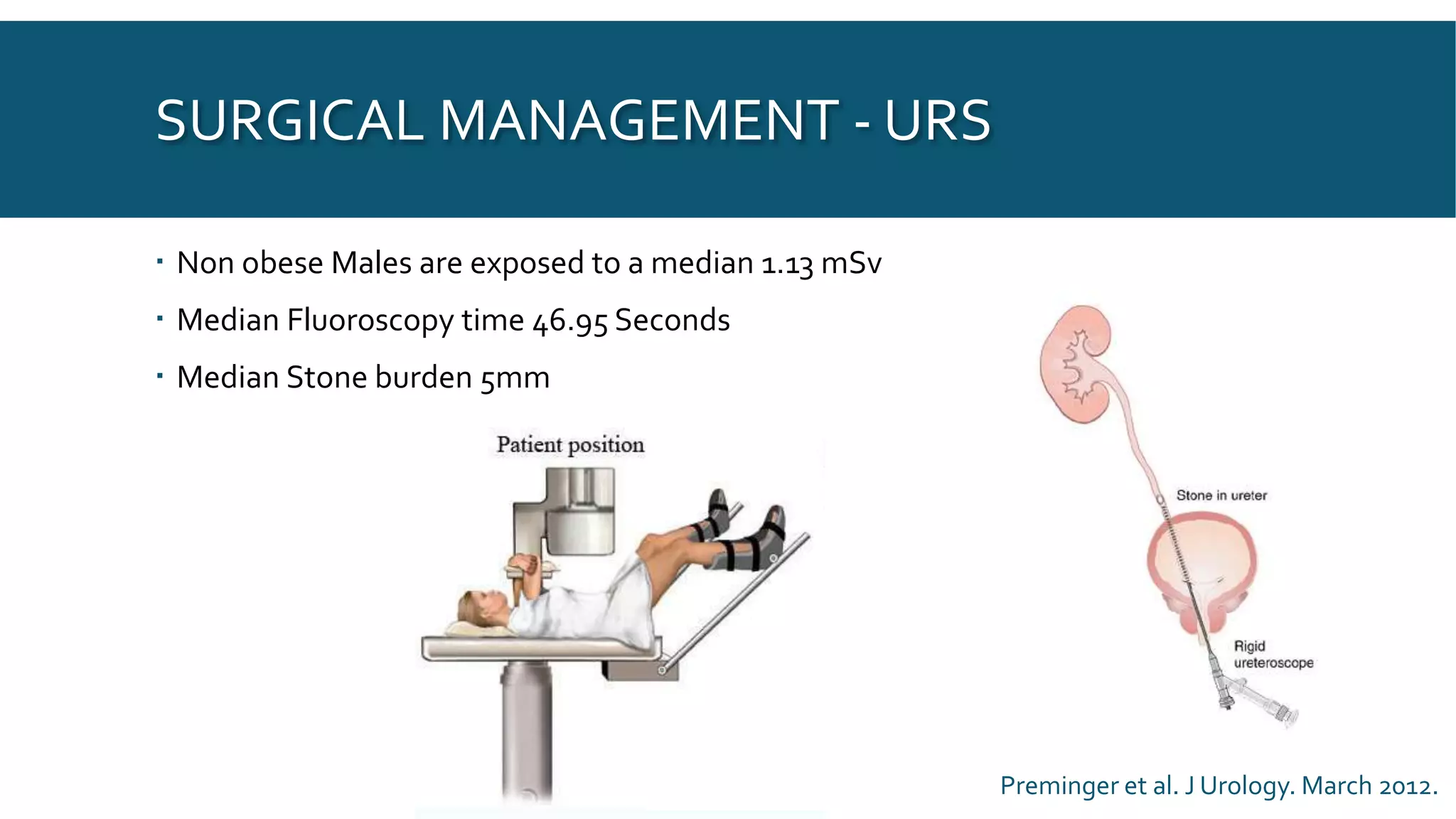
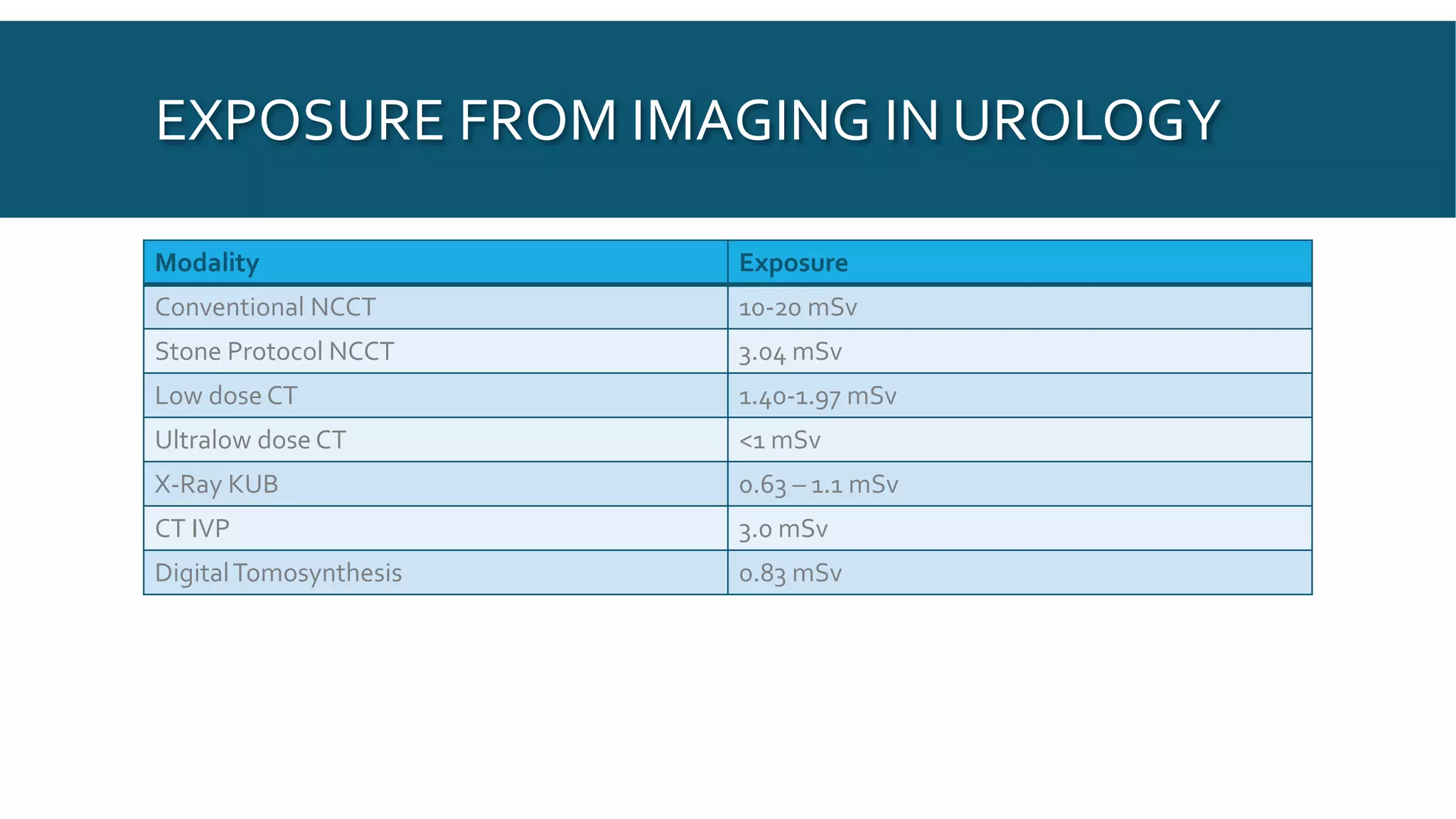
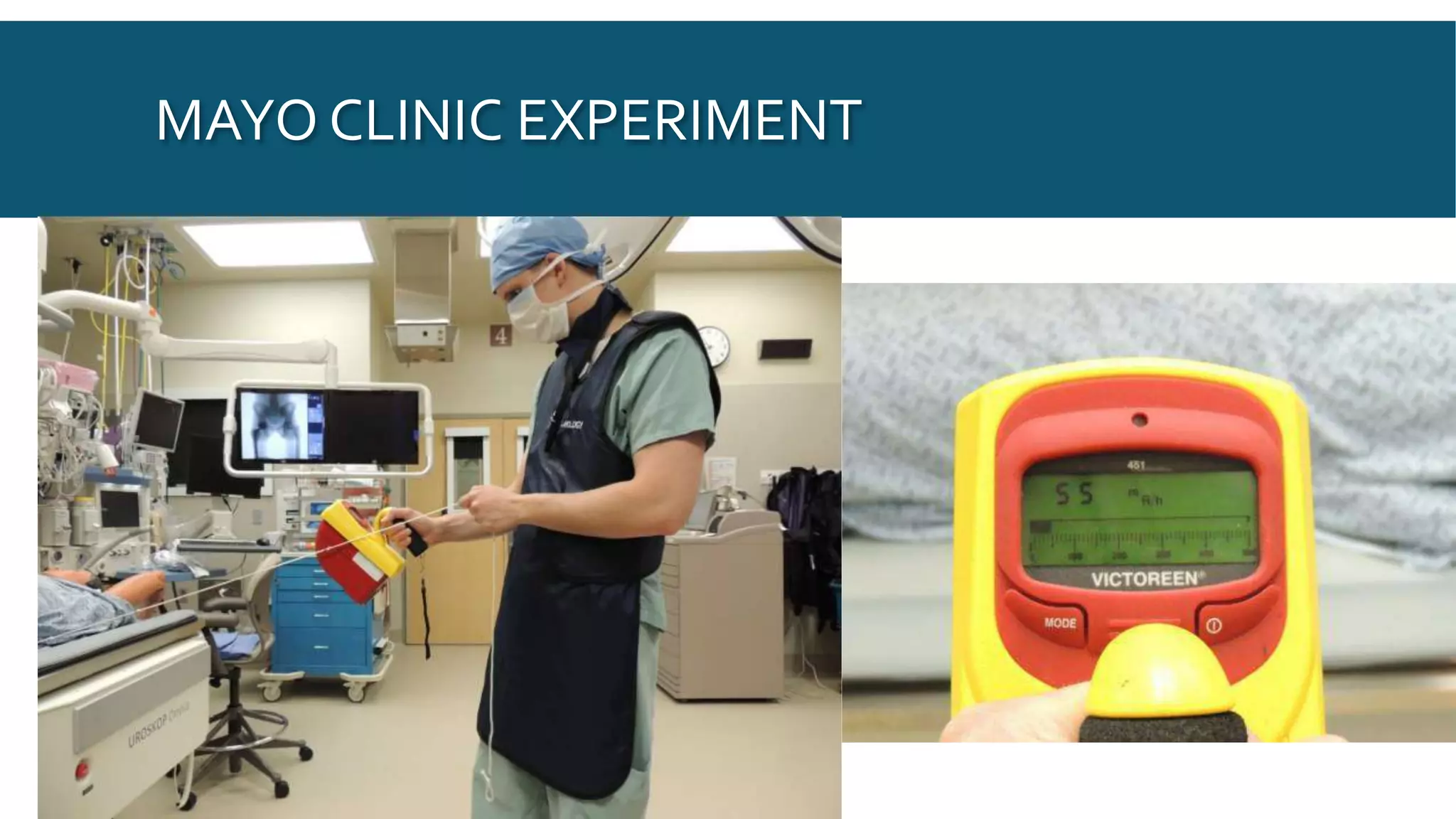
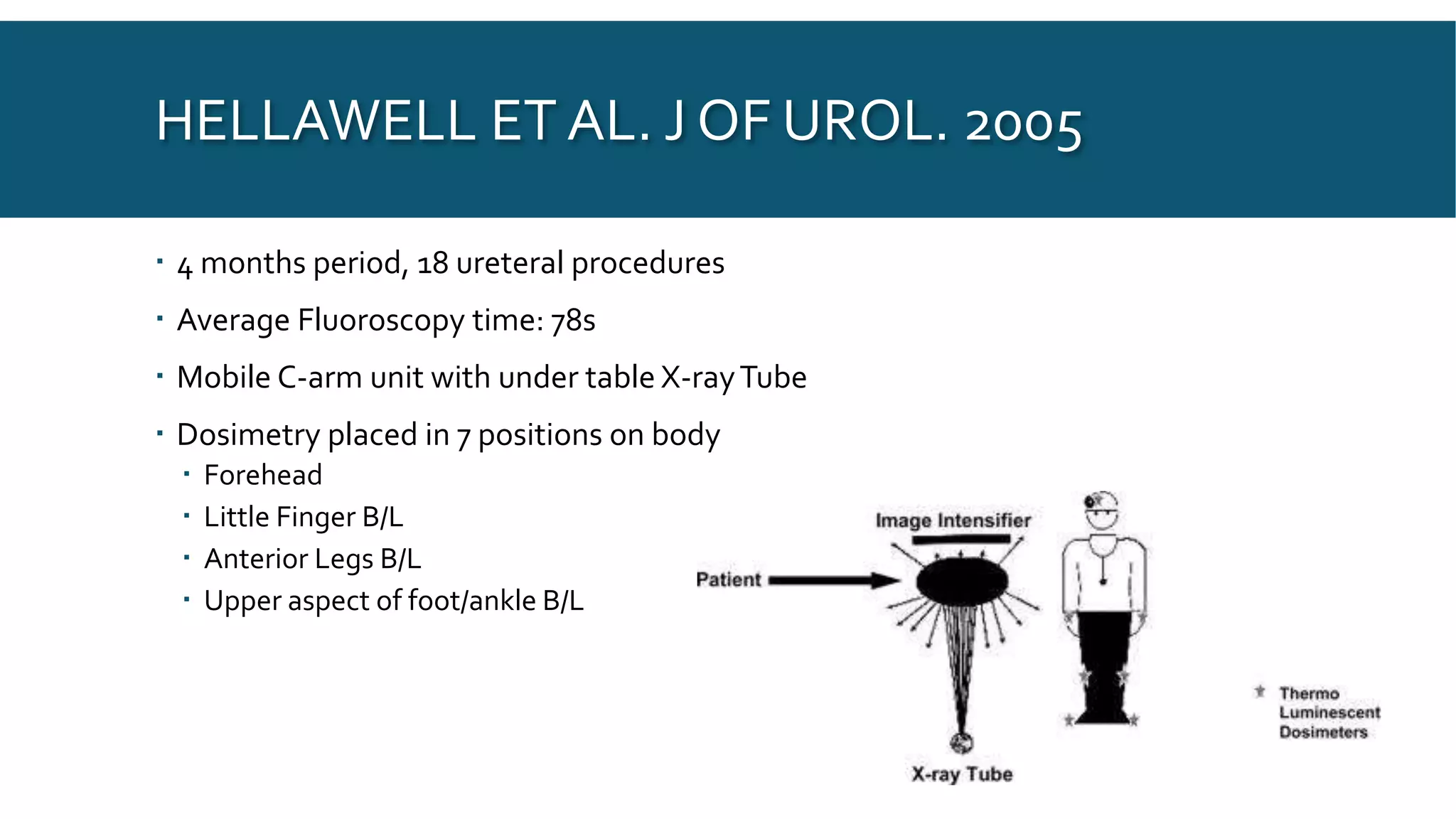
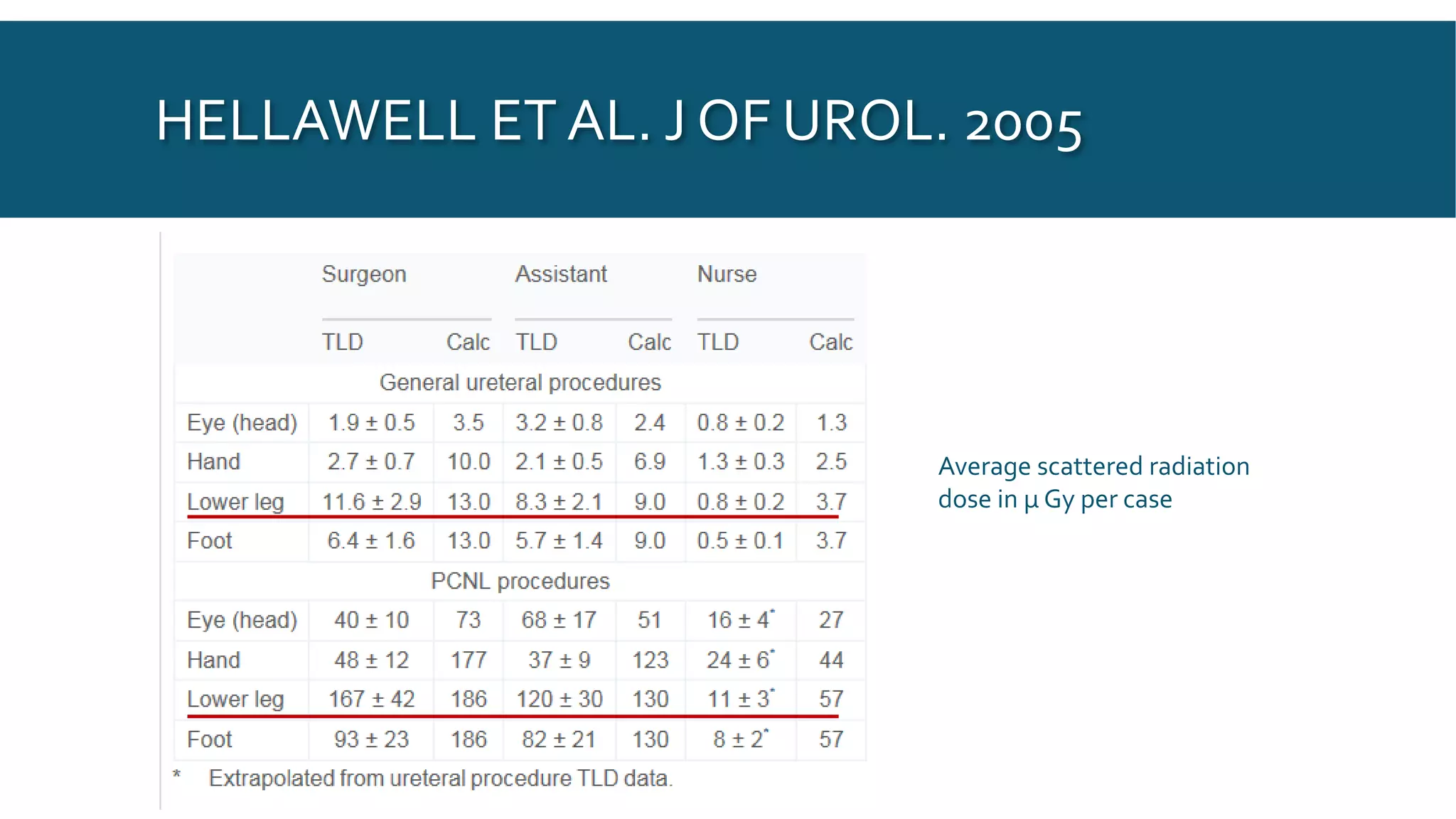
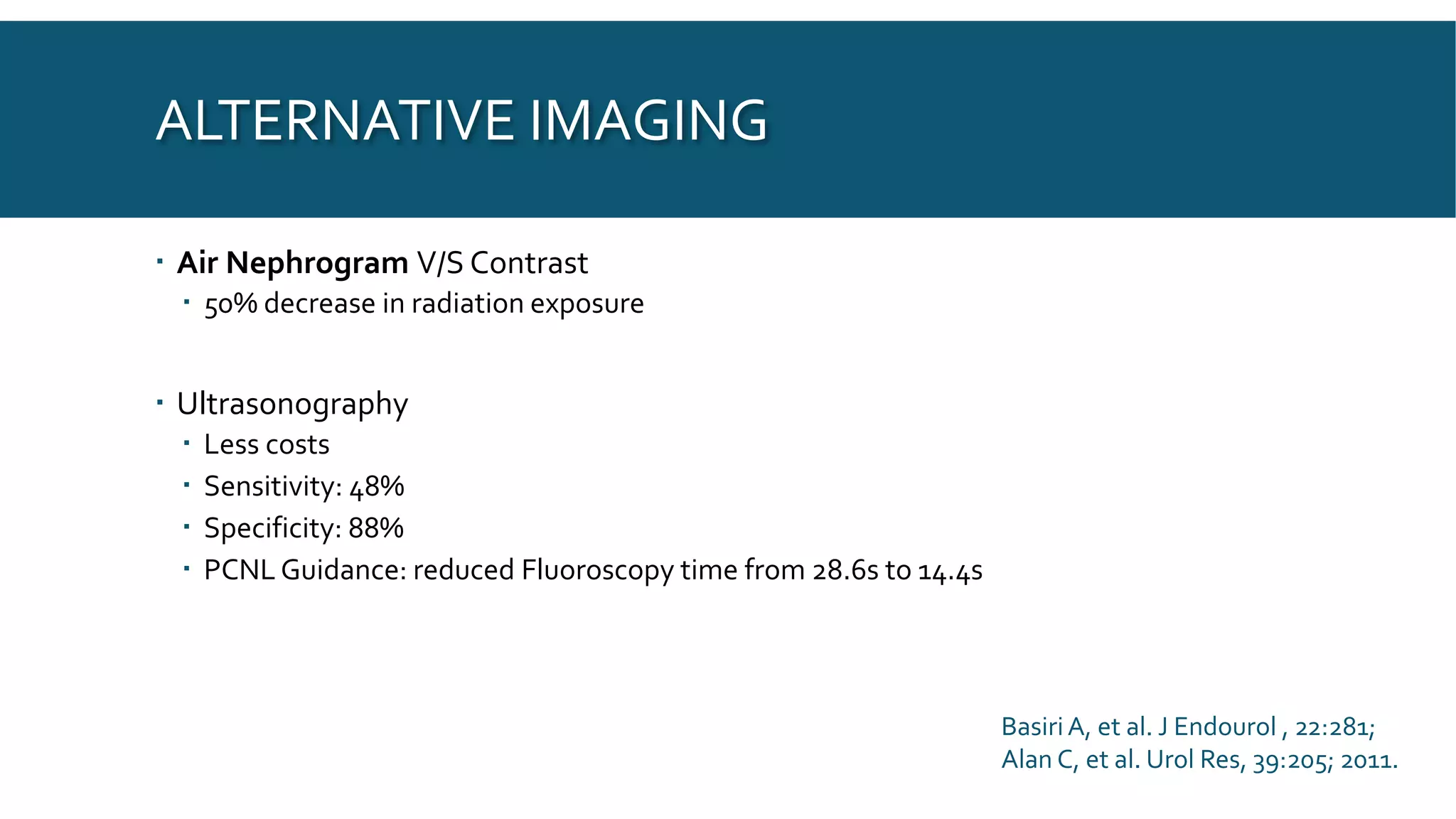
This document discusses radiation exposure in urology. It defines different types of radiation and their effects on the body. Radiation exposure can be a risk for both patients and surgeons in urology procedures like PCNL, URS, and ESWL that use fluoroscopy. The risks of radiation exposure include acute radiation syndrome and increased risk of cancer induction. The document provides recommendations for minimizing radiation exposure through principles like ALARA, protective equipment, procedural controls, alternative imaging techniques, and understanding radiology equipment settings.