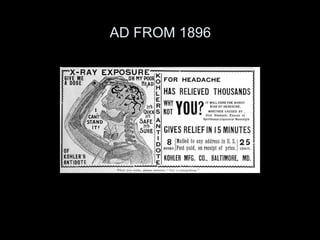
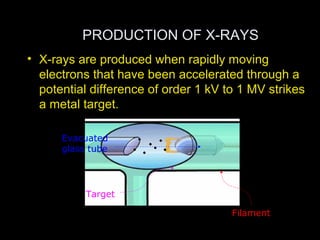
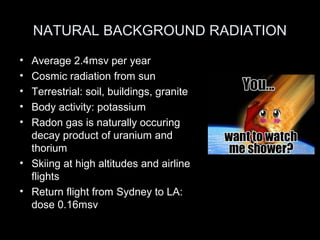
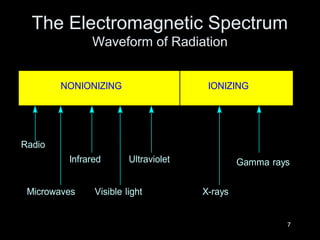
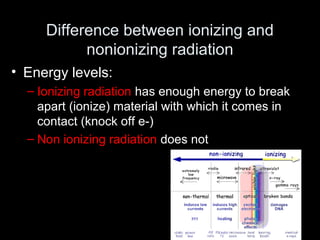
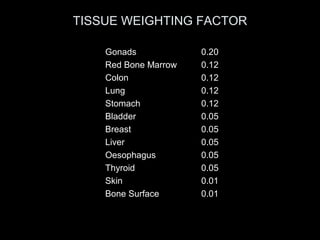
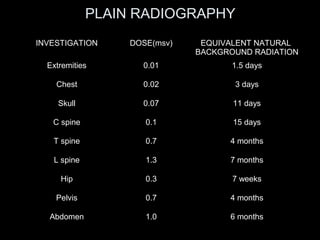
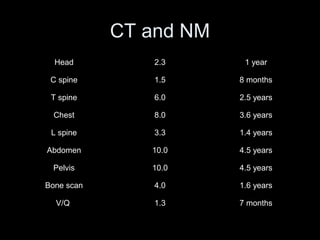
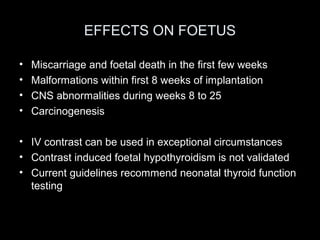
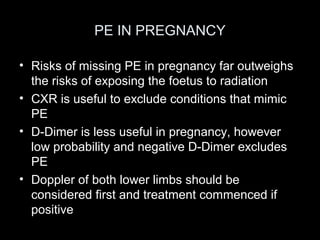
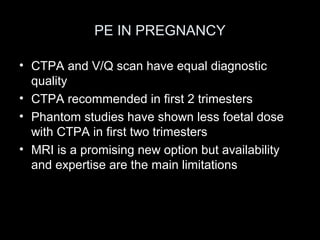
This document discusses the risks of radiation from medical imaging. It begins with a brief history of x-rays and their discovery. It then explains how x-rays and other ionizing radiation are produced, types of radiation, and the difference between ionizing and non-ionizing radiation. The biological effects of radiation exposure are described as either somatic (impacting exposed cells) or genetic (impacting future generations). While low levels of radiation from diagnostic exams pose uncertain risks, current models suggest that any exposure increases cancer risk. The document provides radiation doses from various medical imaging tests and their equivalent natural background radiation doses. It stresses justifying exams, using the lowest possible doses, and alternative non-ionizing tests when possible.