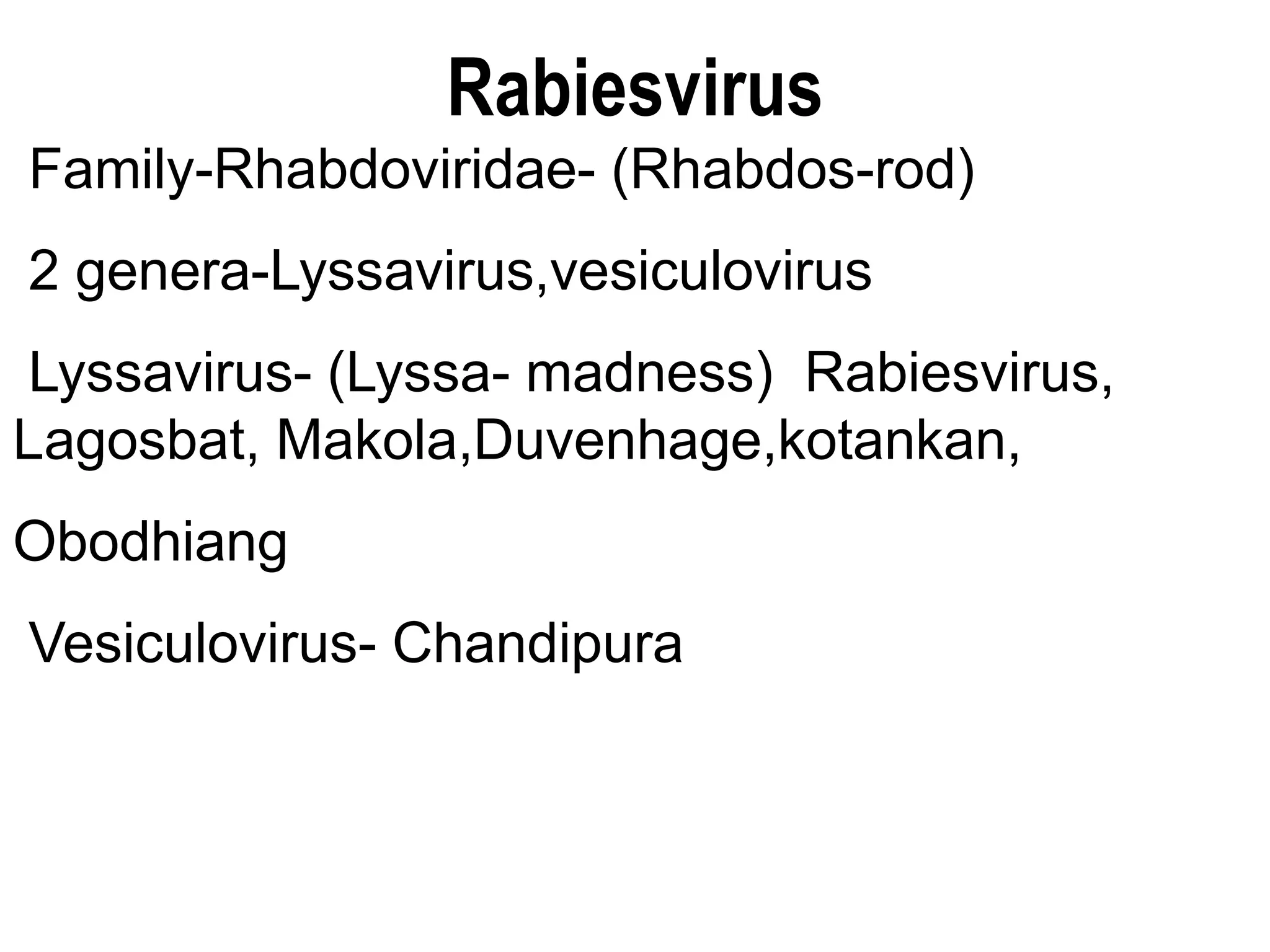
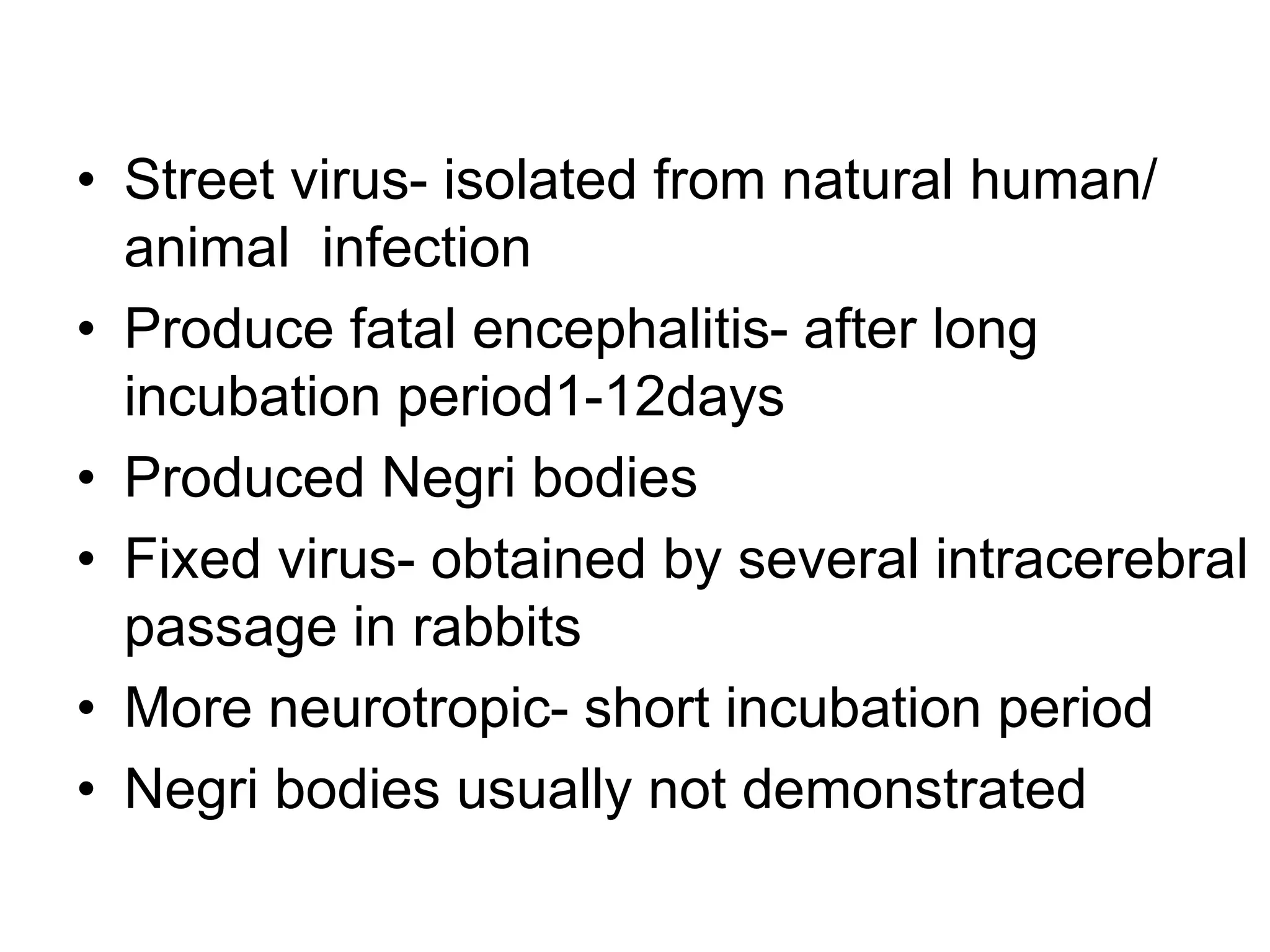
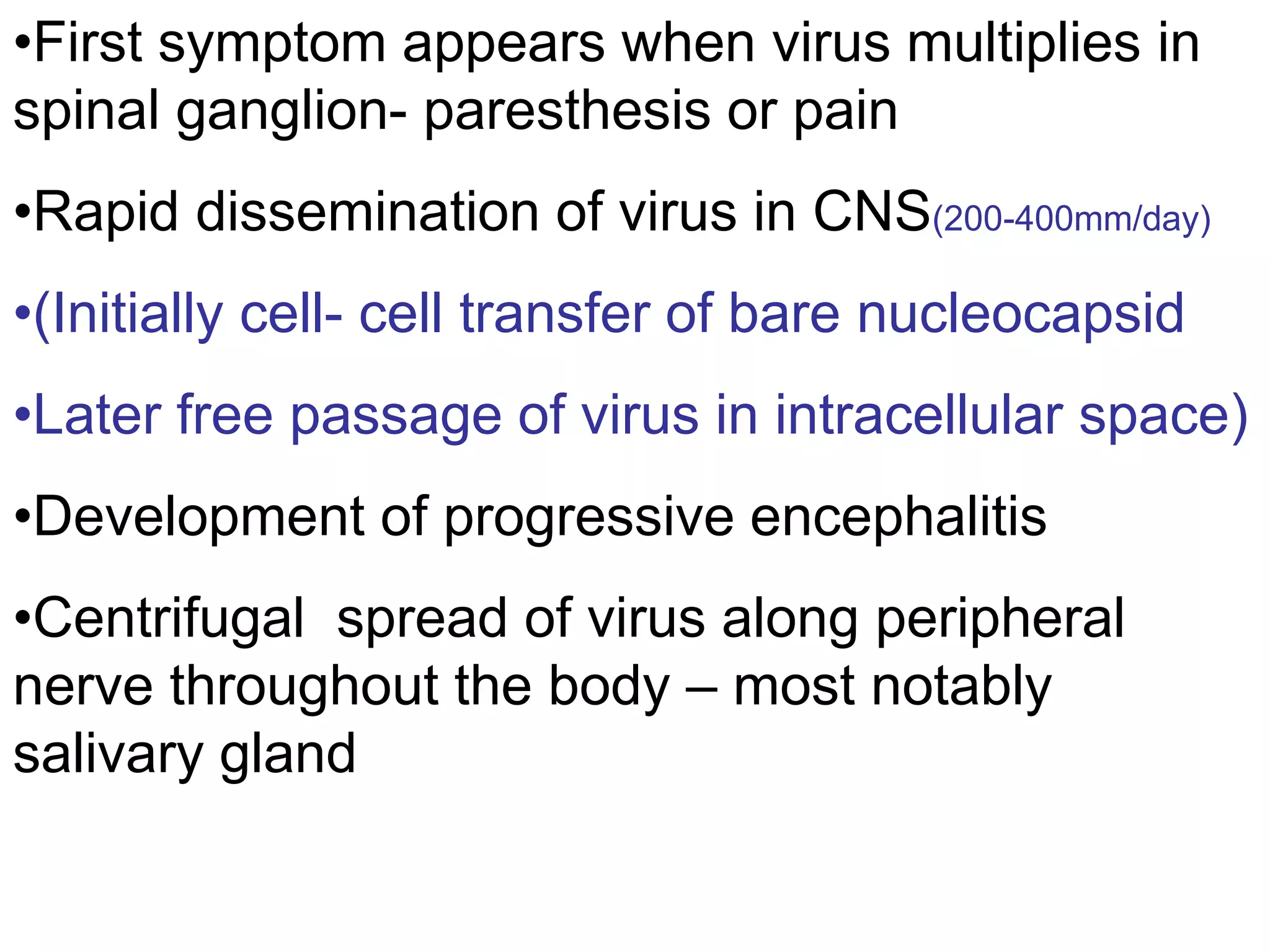
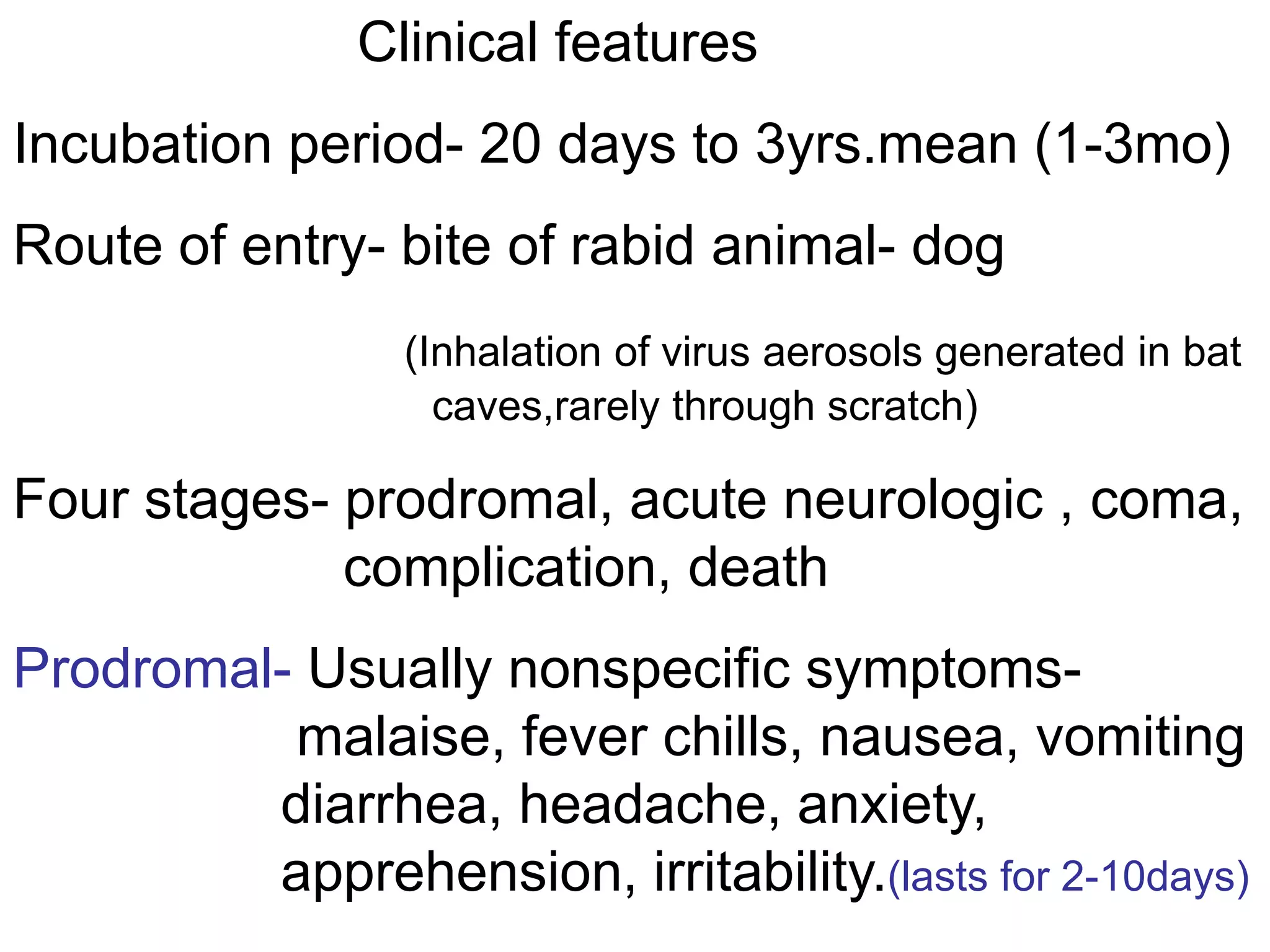
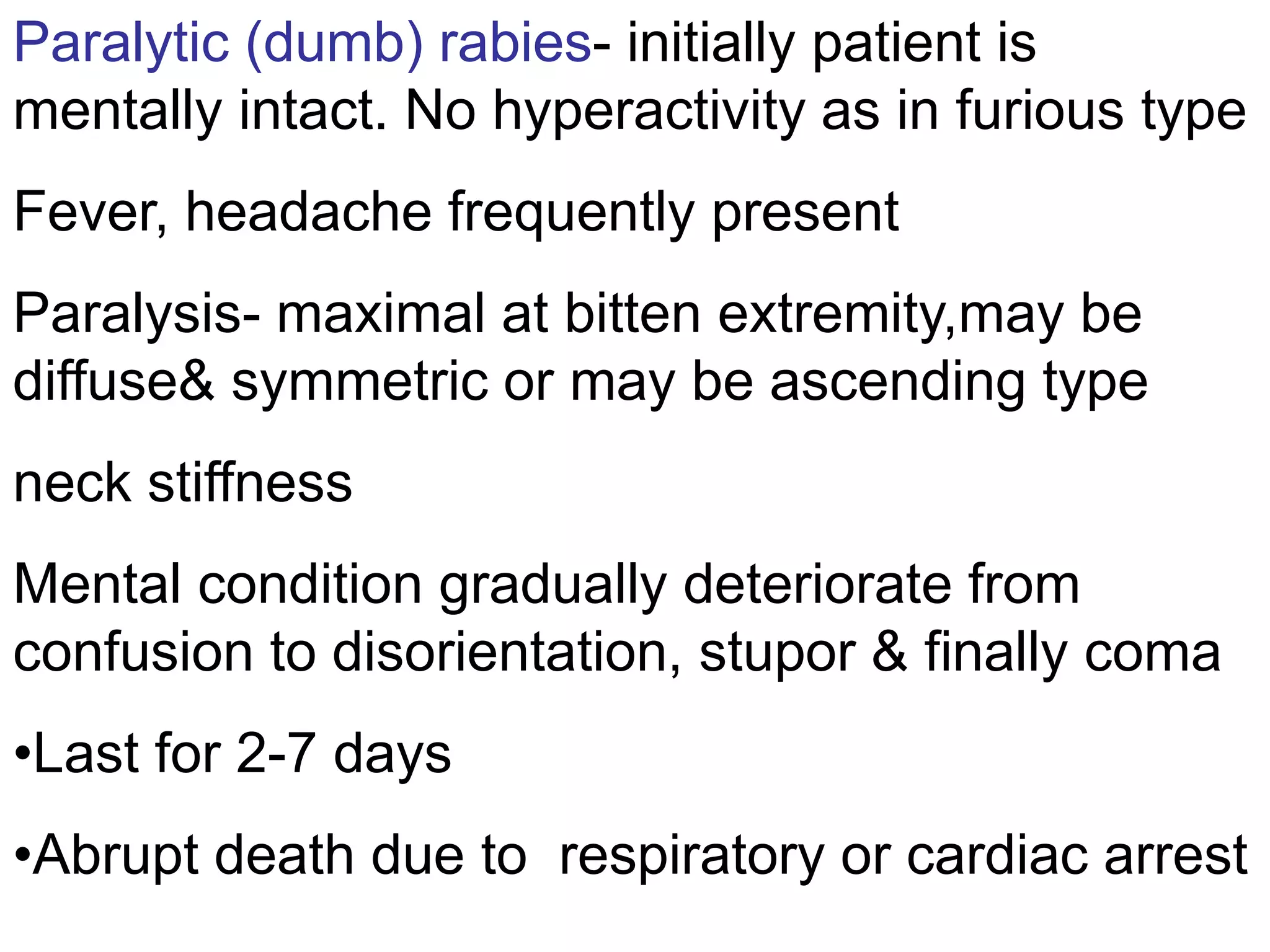
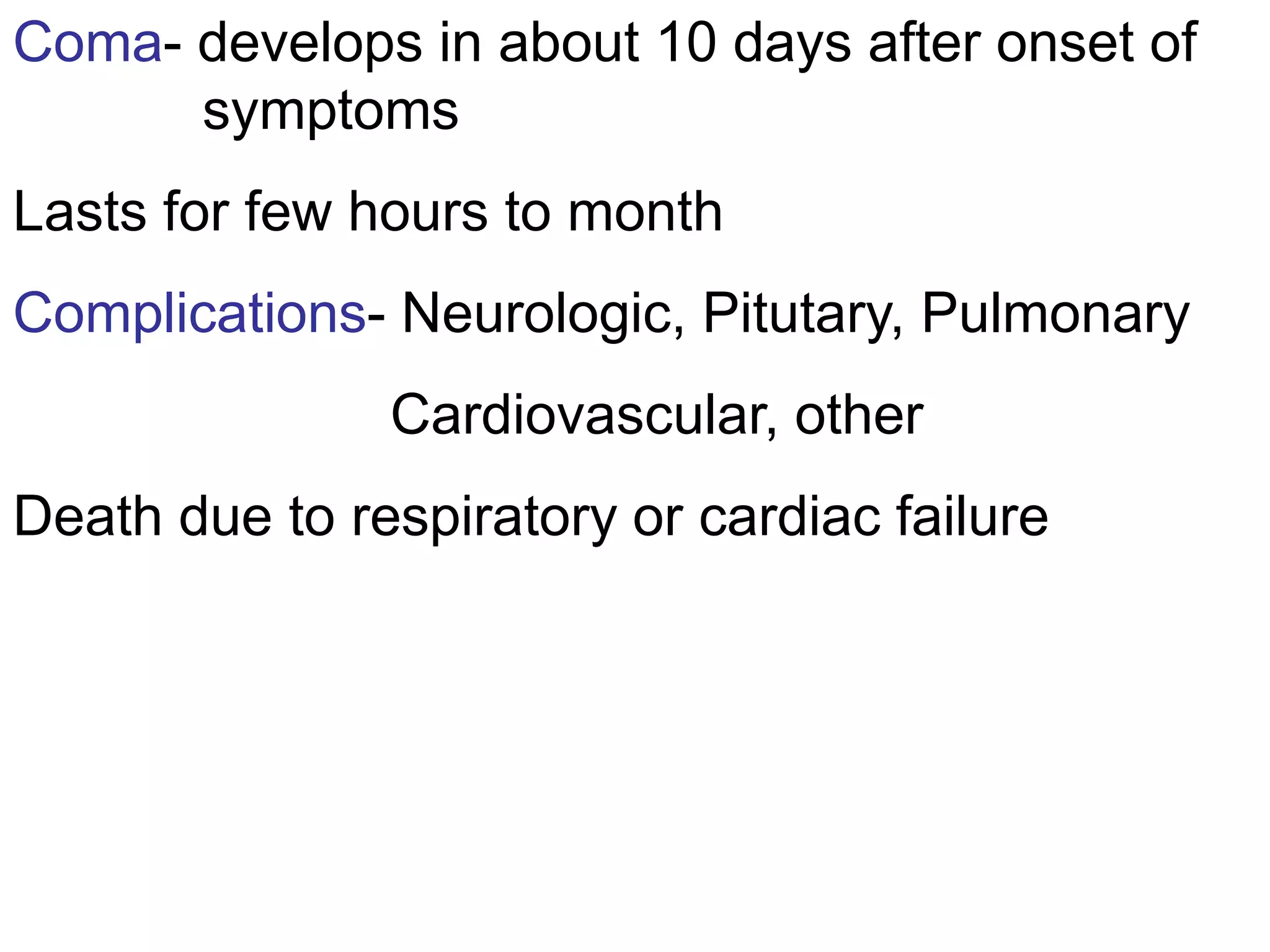
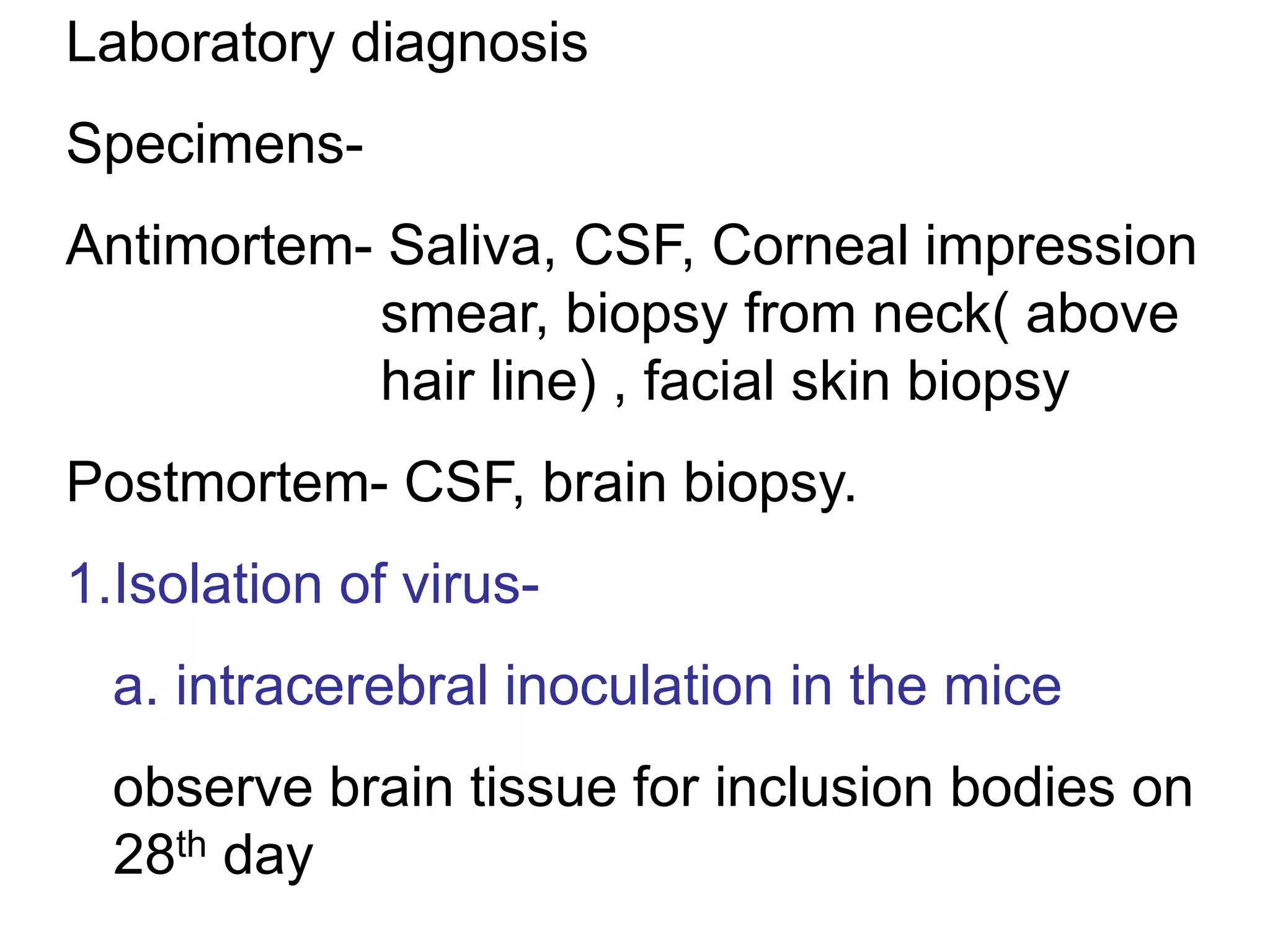
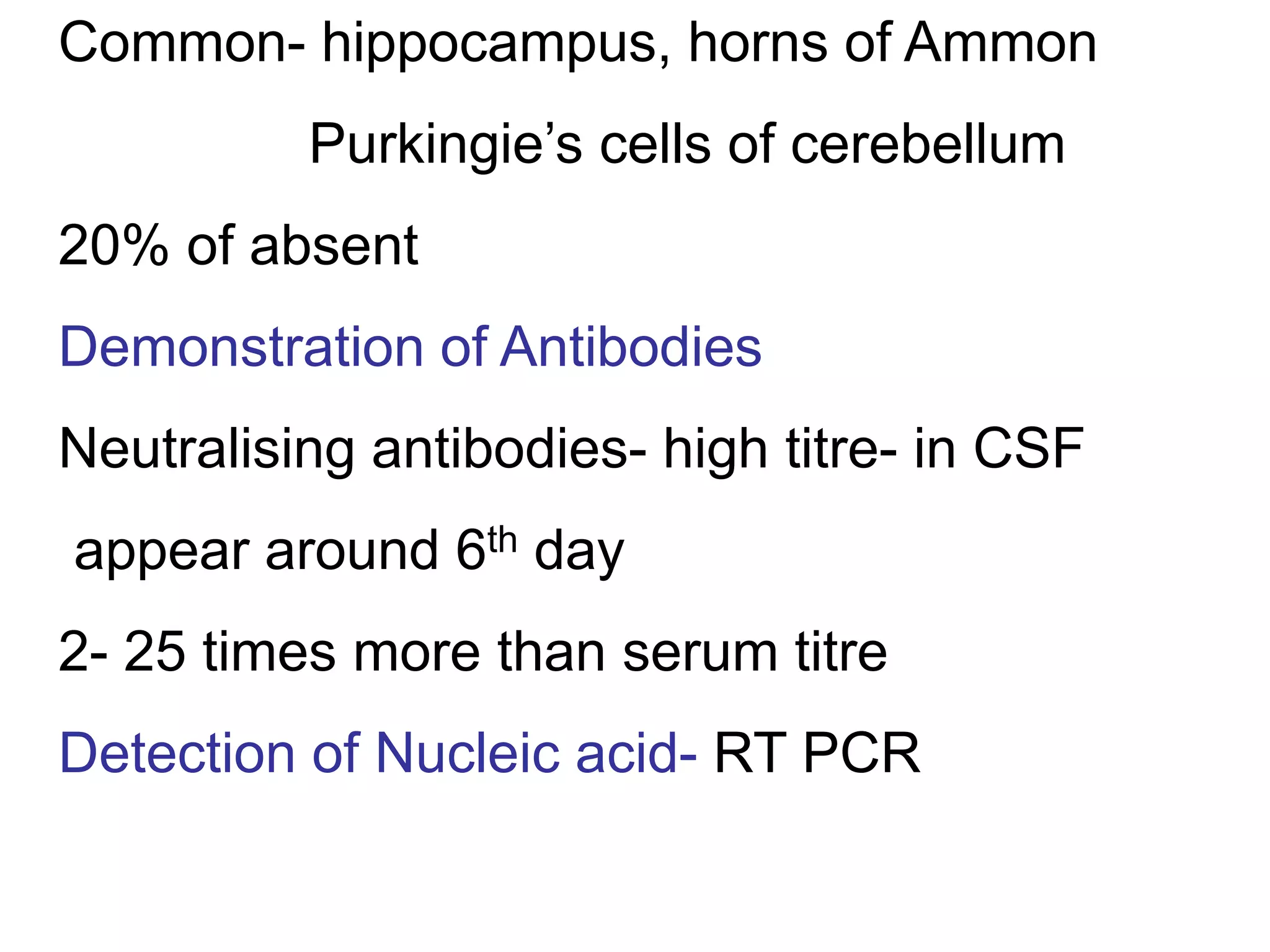
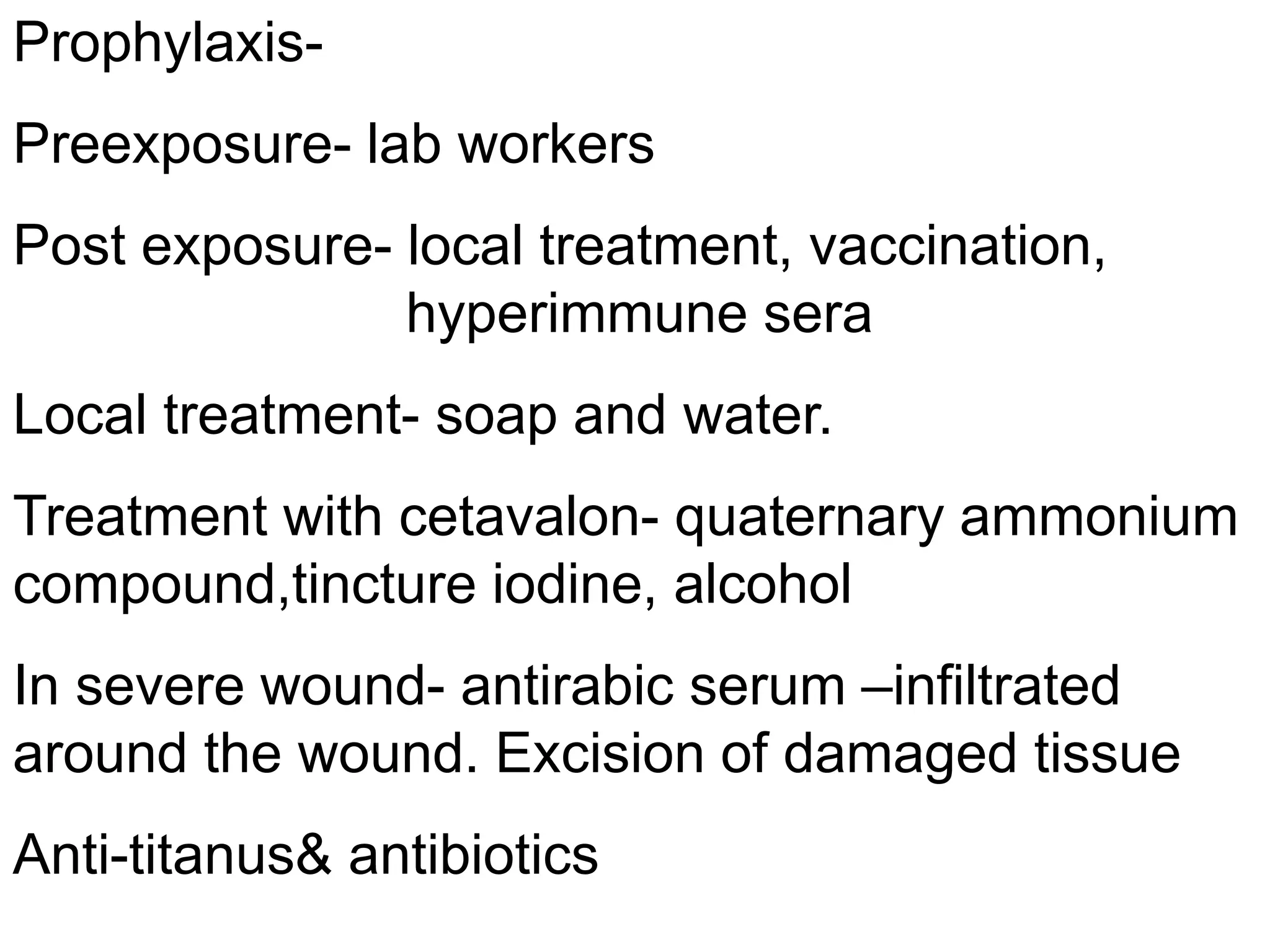
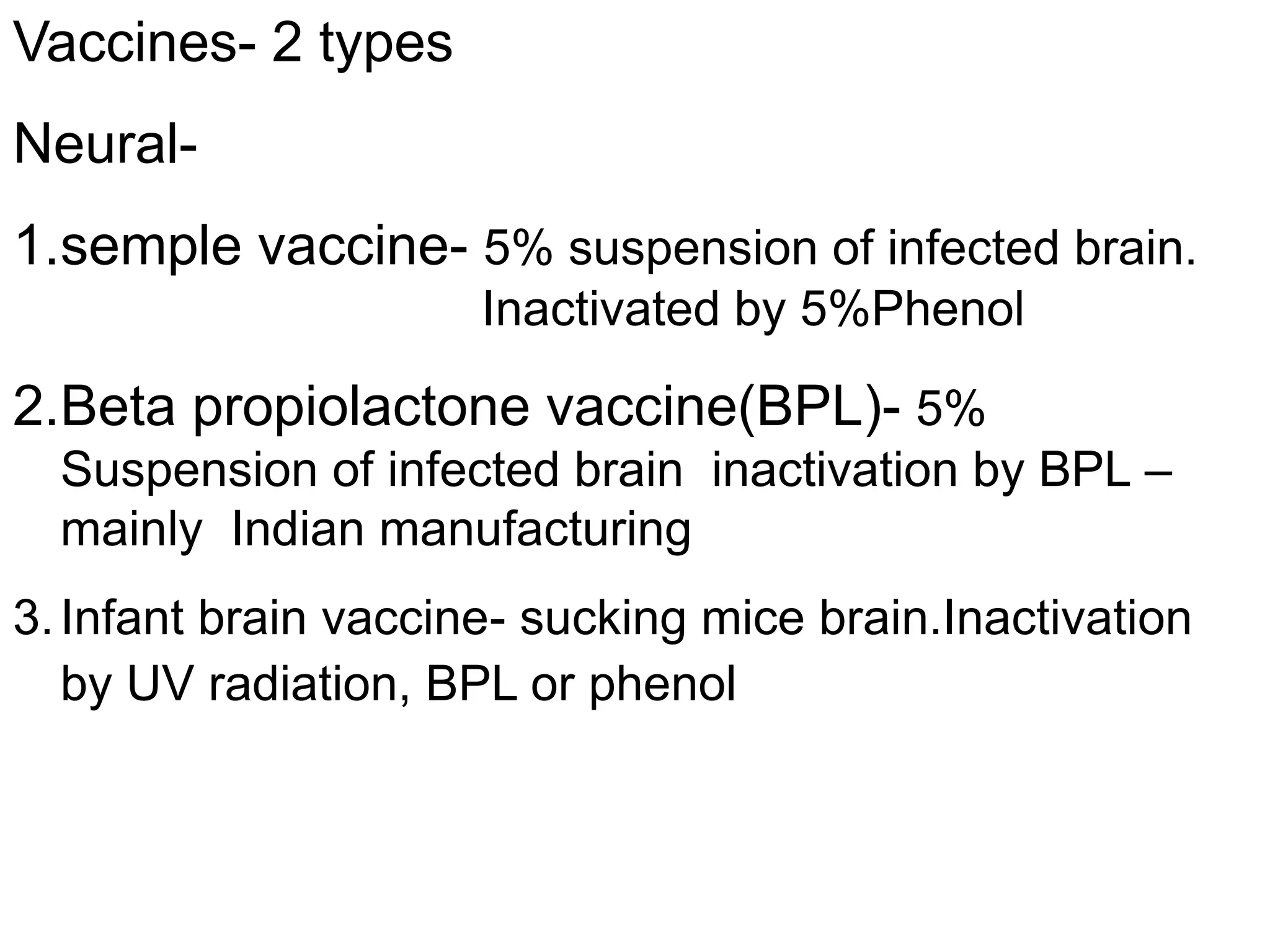
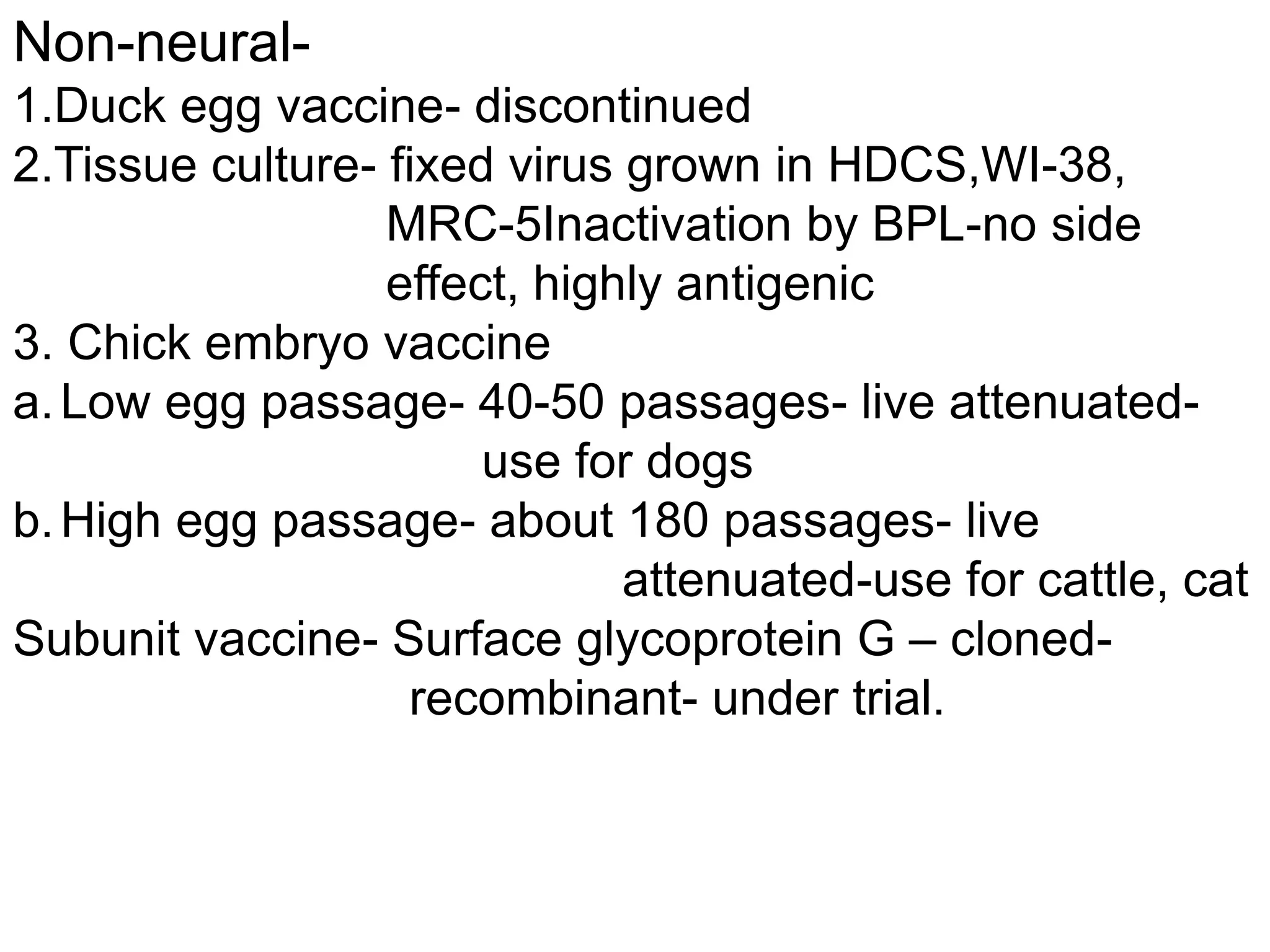
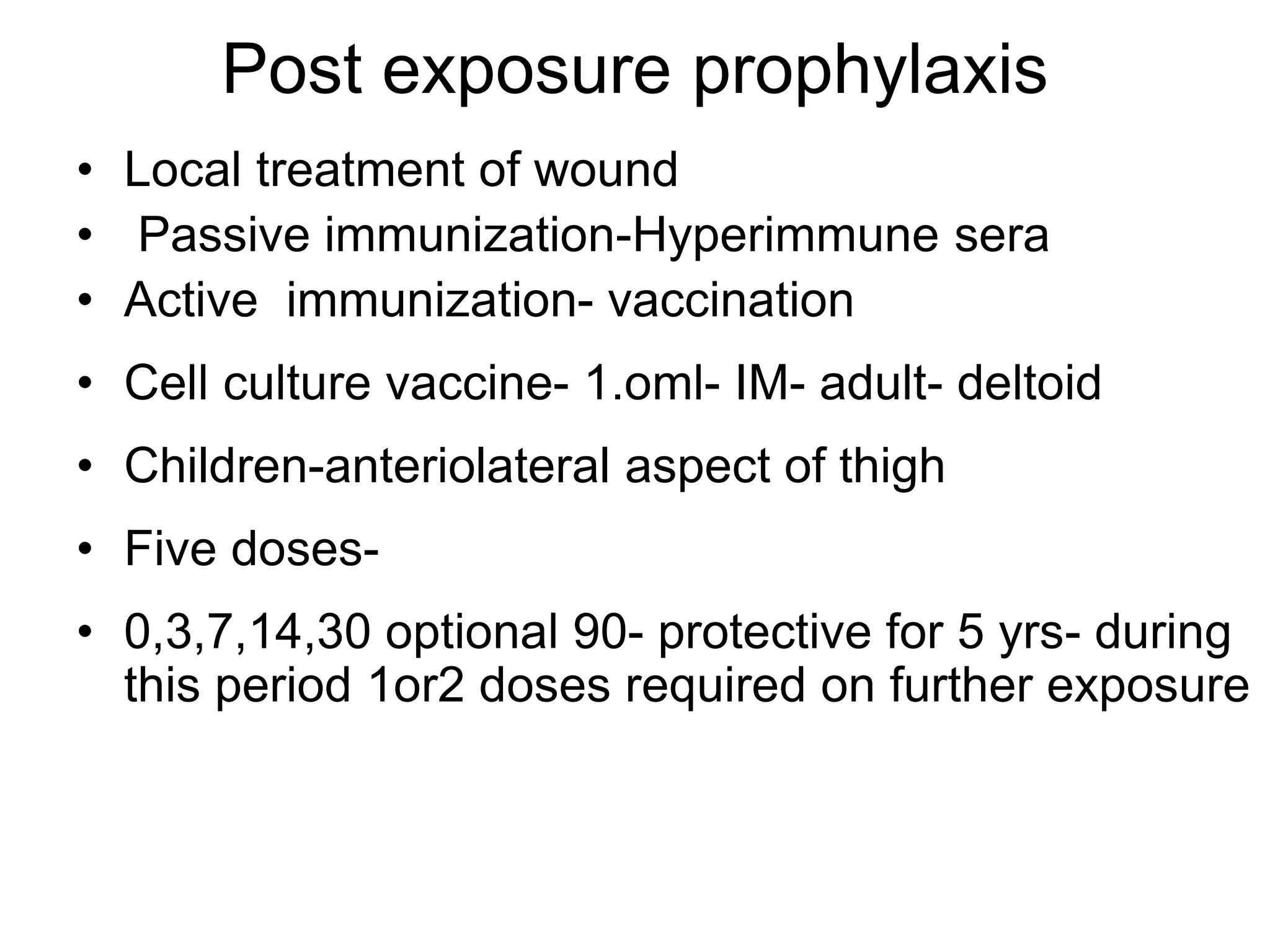
Rabies virus is a neurotropic virus in the Rhabdoviridae family. It is bullet-shaped and enveloped with glycoprotein spikes. It has a single-stranded RNA genome that encodes five proteins. Rabies virus is highly resistant in the environment and transmitted through bites from infected animals. It travels through peripheral nerves to the central nervous system. Clinical features include an incubation period of 1-3 months followed by neurological symptoms such as hyperactivity, paralysis, and eventually coma. Laboratory diagnosis involves virus isolation, antigen detection, antibody detection, and PCR. Prophylaxis includes vaccination both pre- and post-exposure, as well as administration of rabies immunoglobulin.