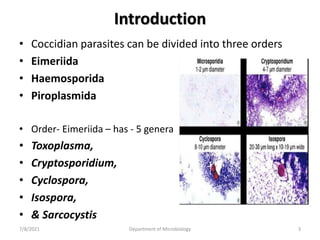
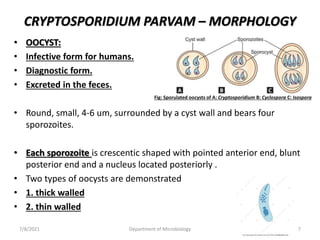
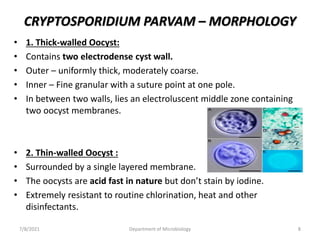
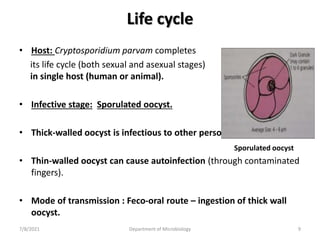
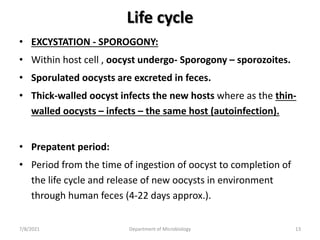
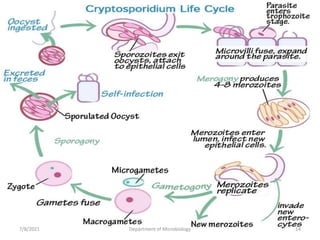
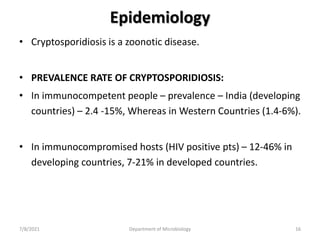
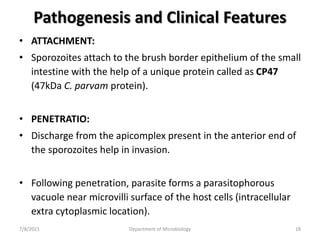
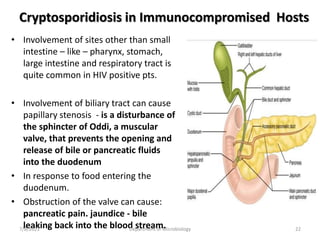
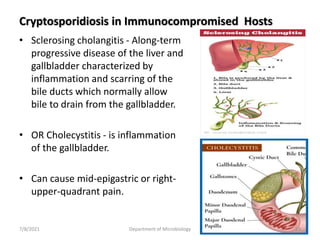
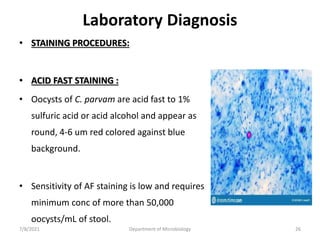
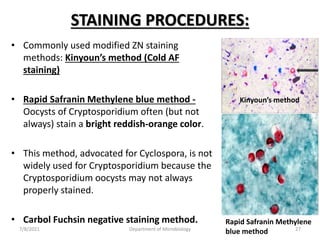
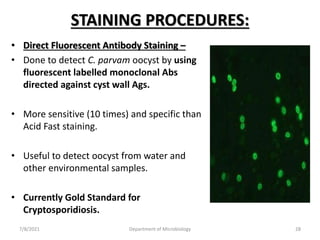
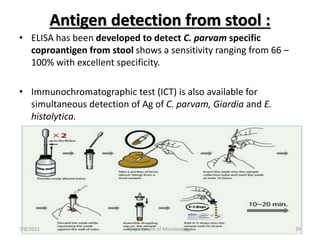
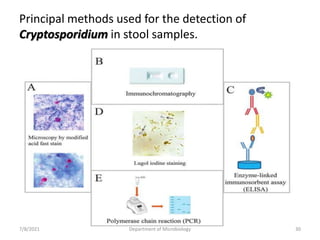
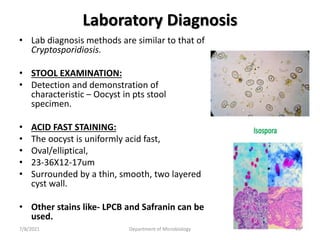
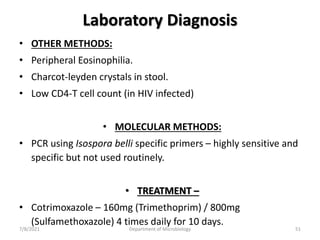
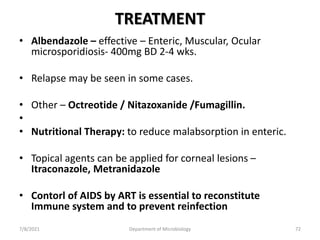
The document discusses coccidian parasites, with a focus on Cryptosporidium parvum. It describes the parasite's morphology, life cycle, epidemiology, pathogenesis, and clinical features. Cryptosporidium parvum causes cryptosporidiosis, an intestinal illness that typically results in self-limiting diarrhea but can cause serious, chronic diarrhea in immunocompromised patients like those with HIV/AIDS. Laboratory diagnosis involves examining stool samples microscopically to identify the parasite's oocysts.