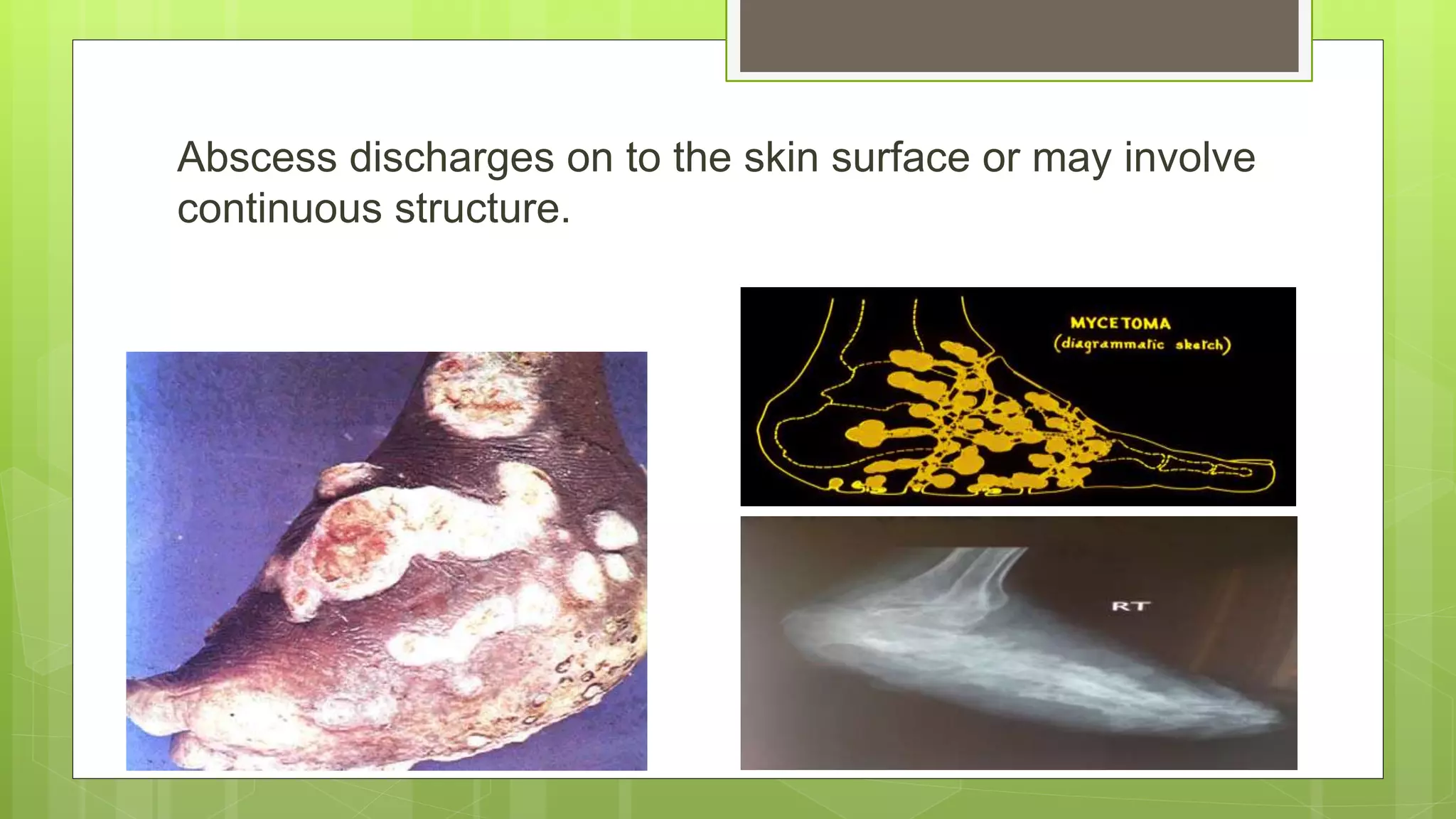
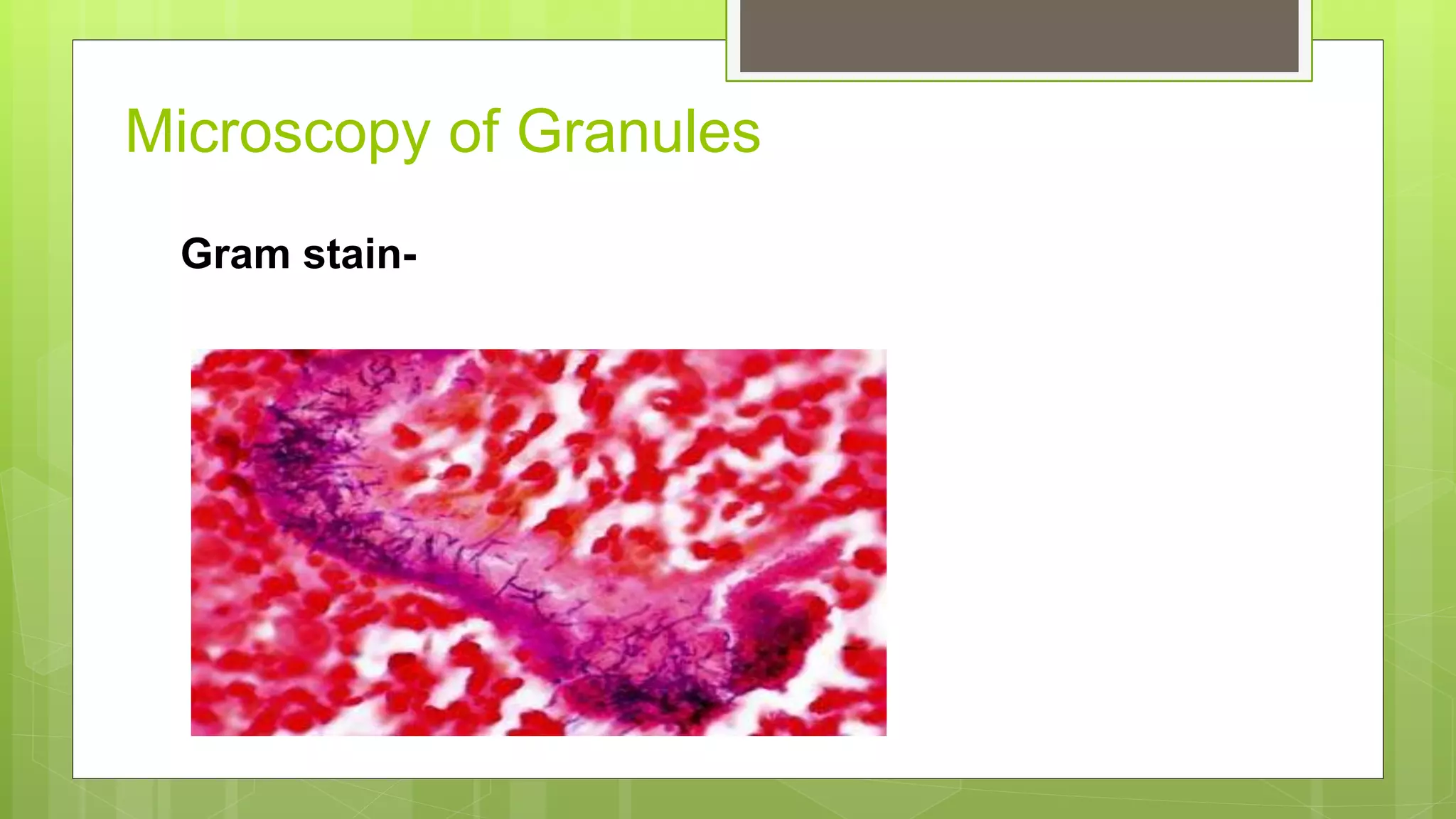
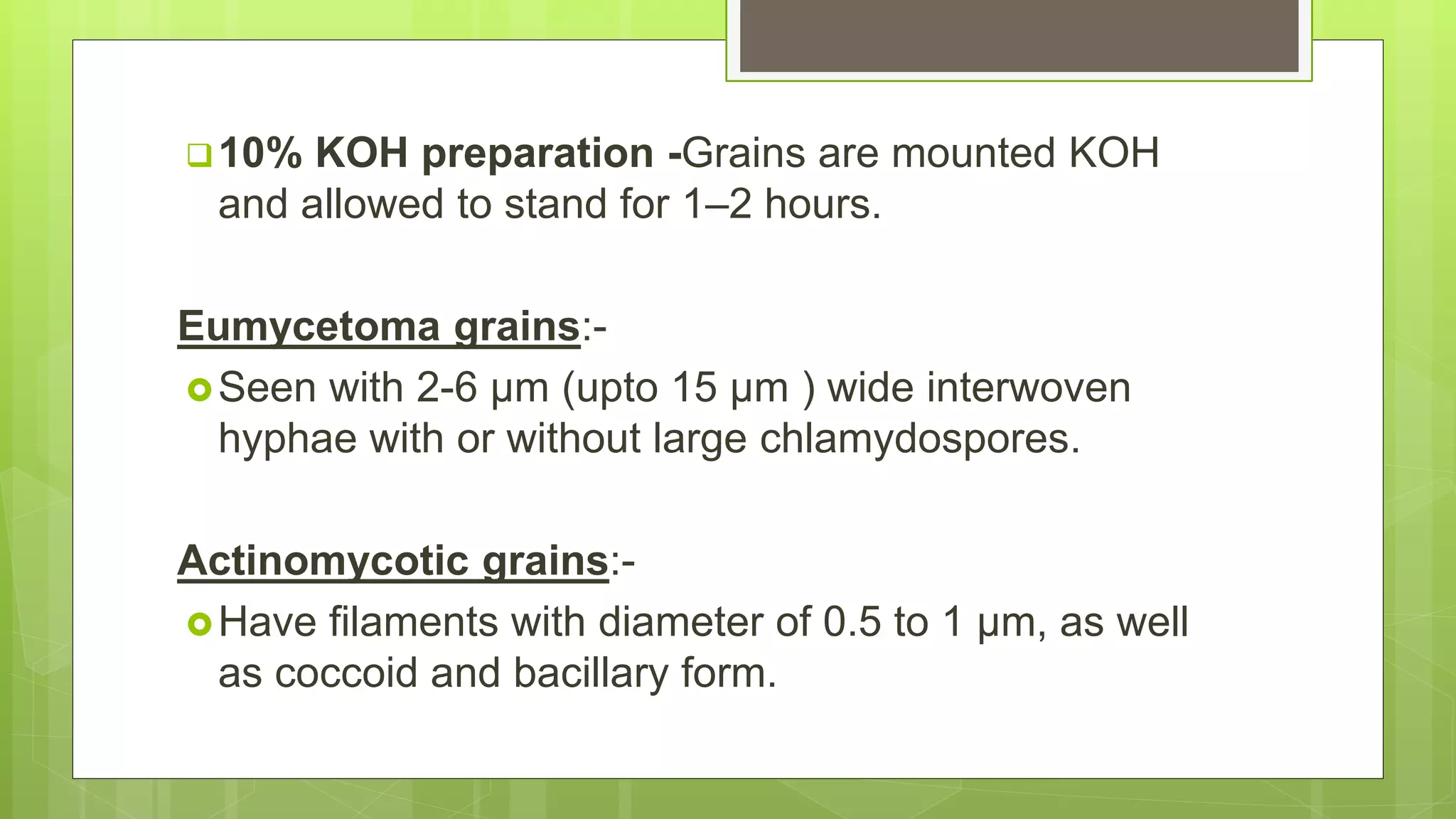
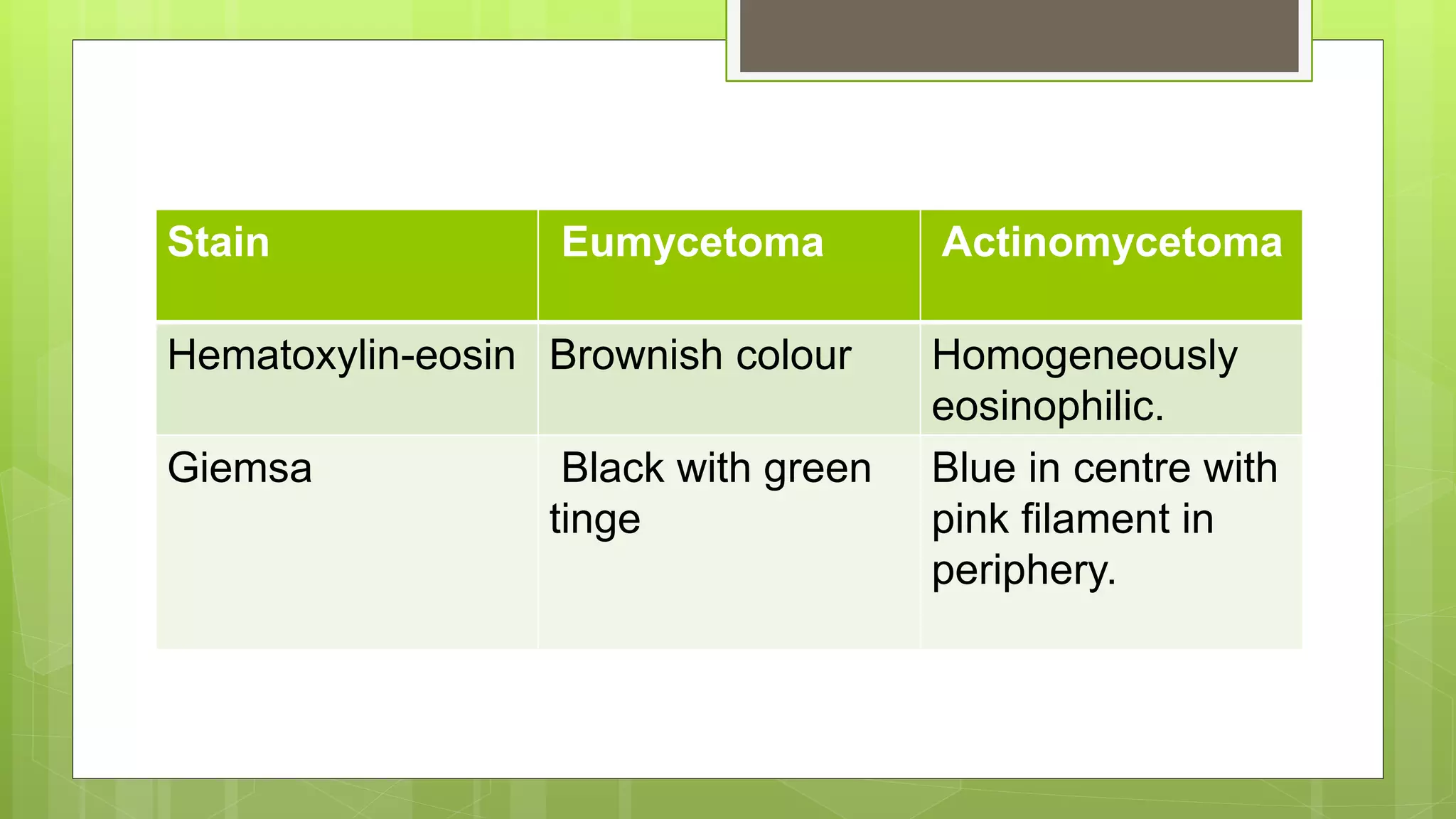
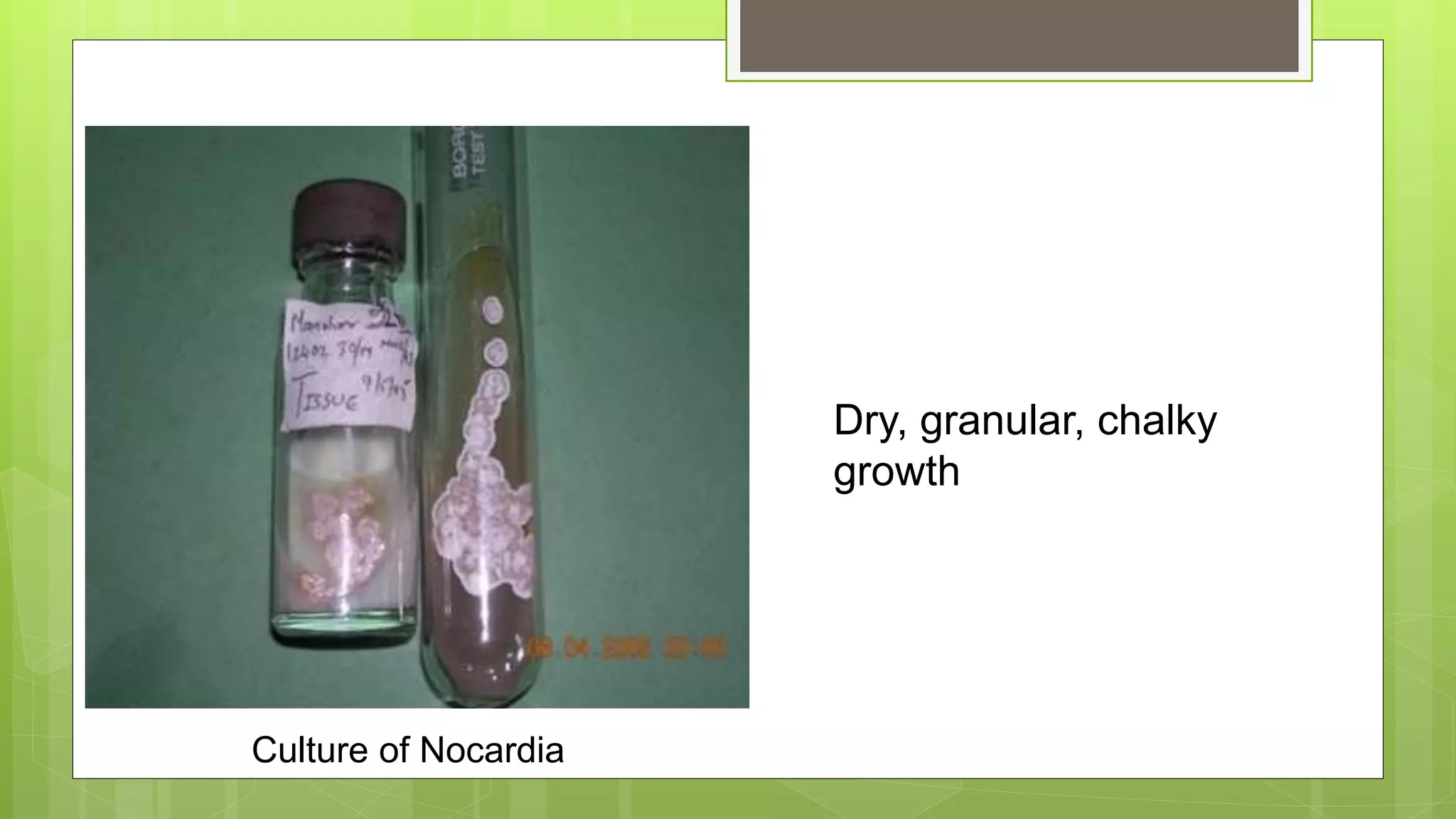
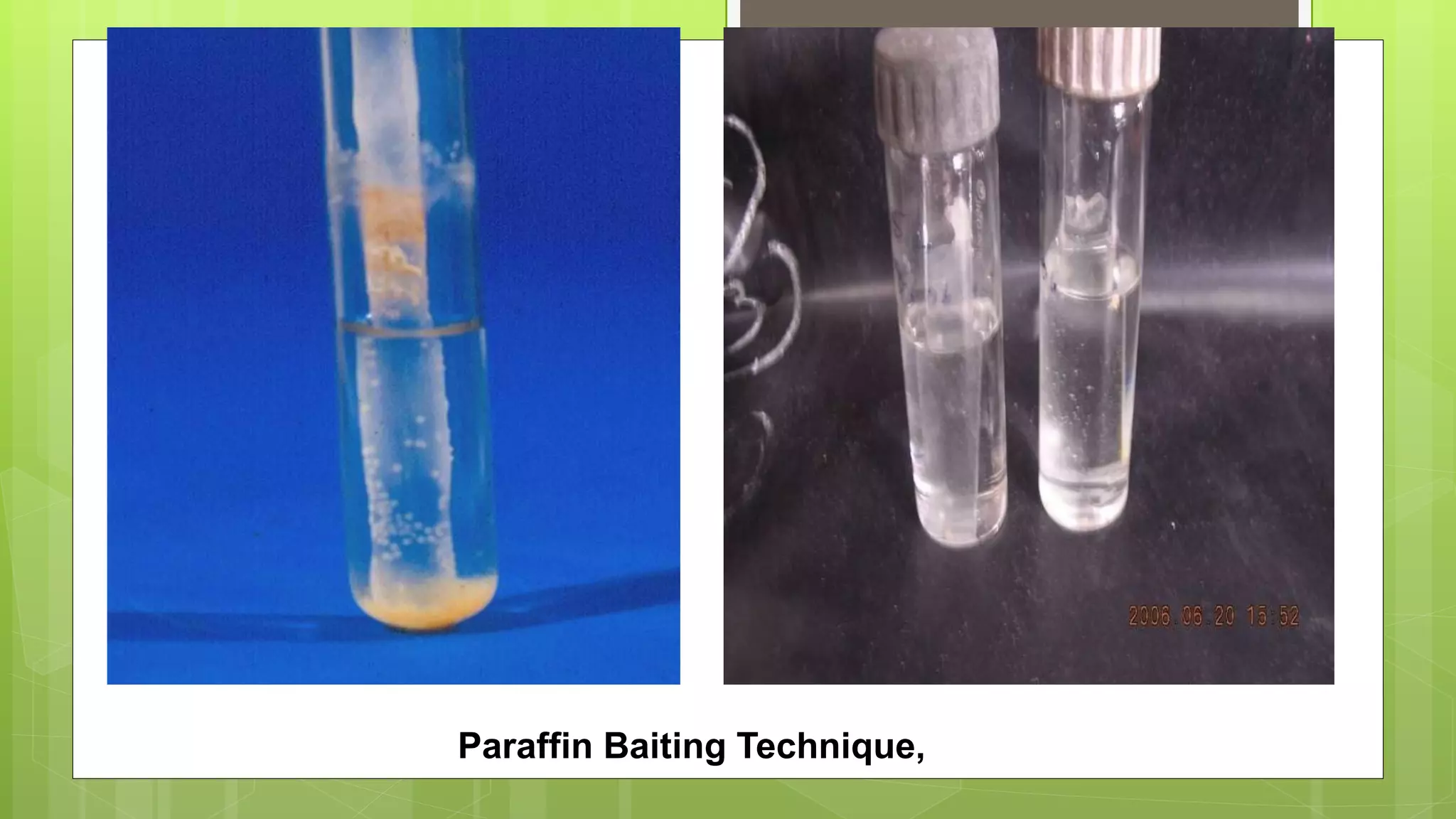
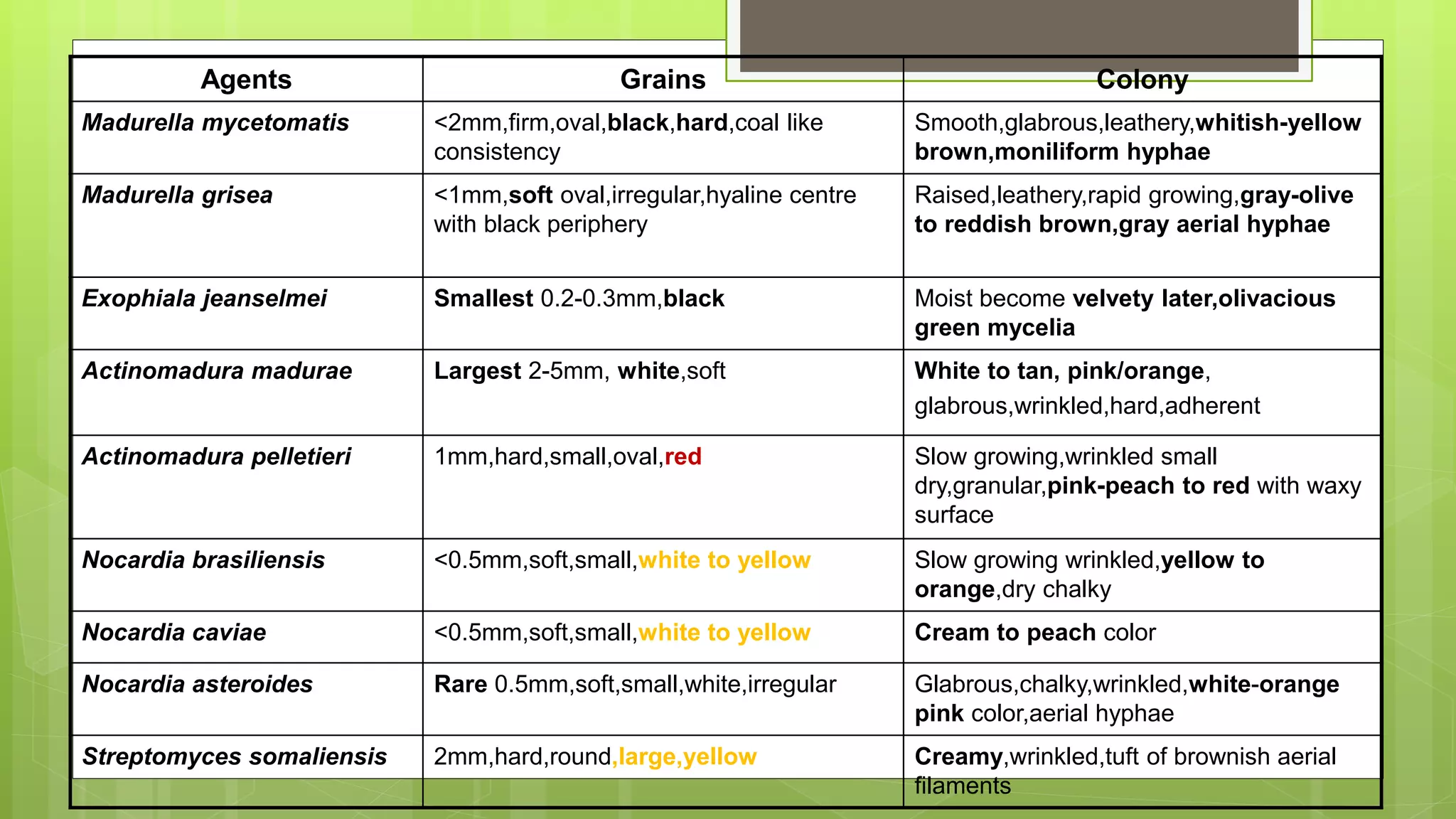
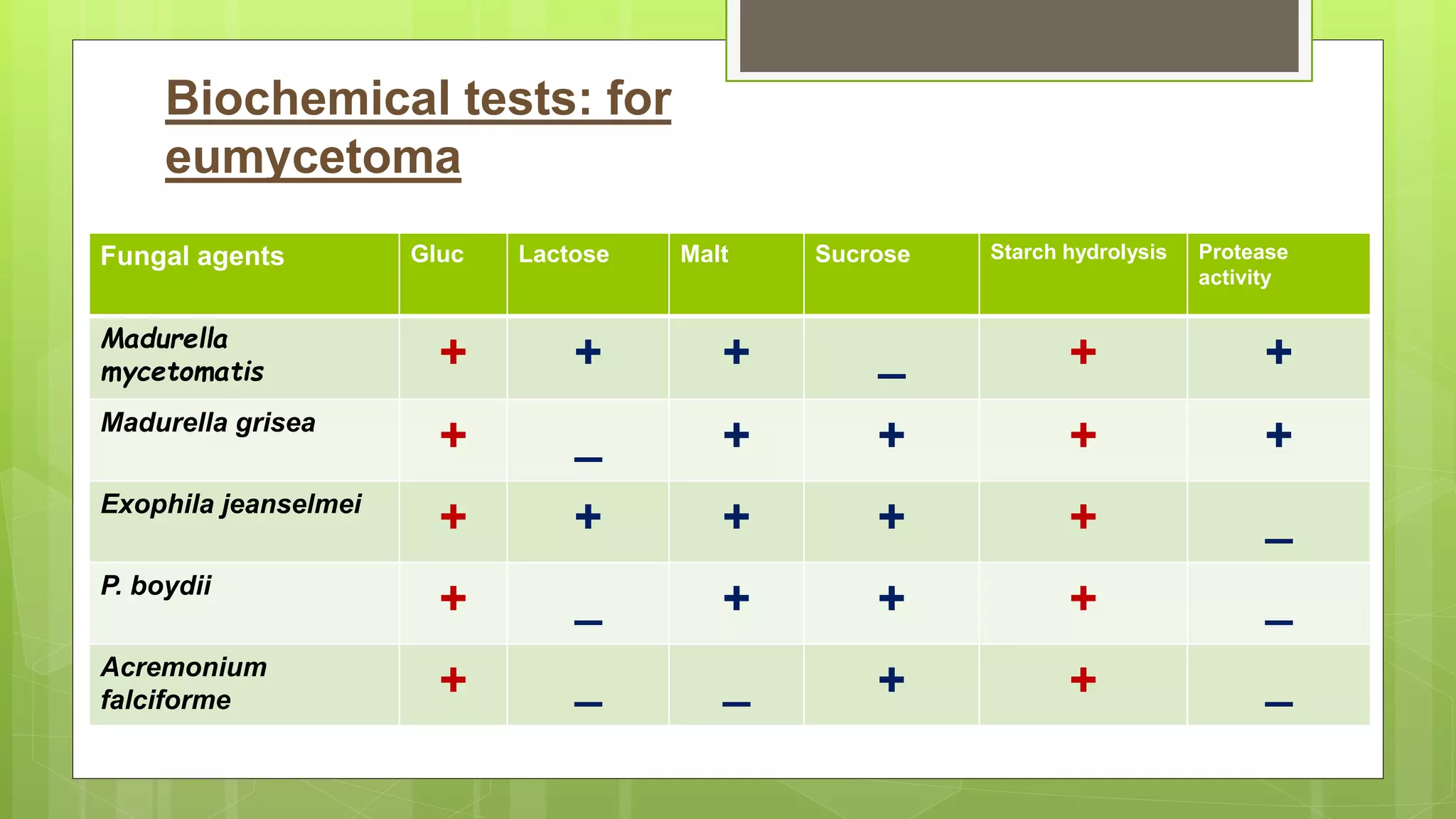
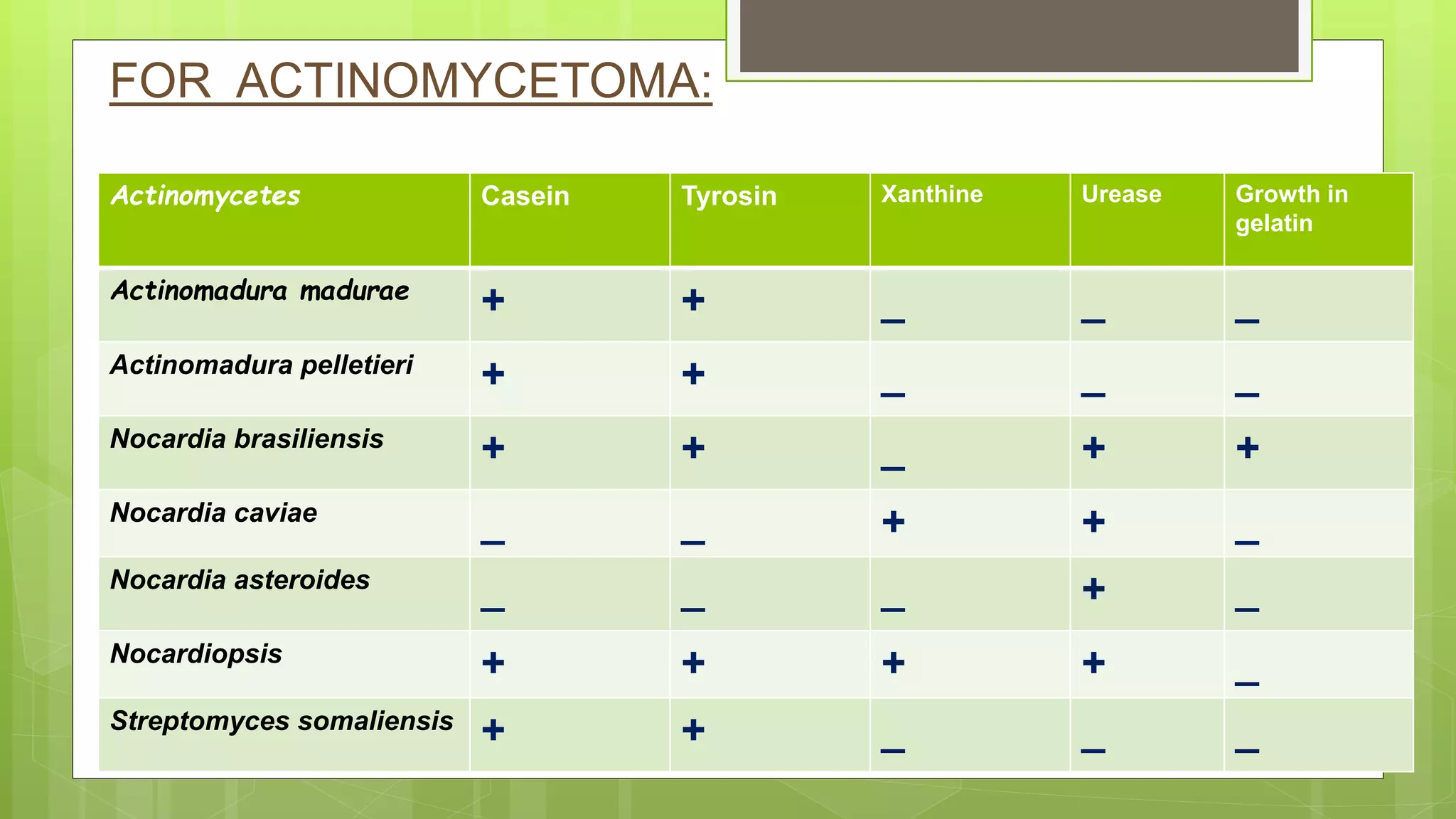
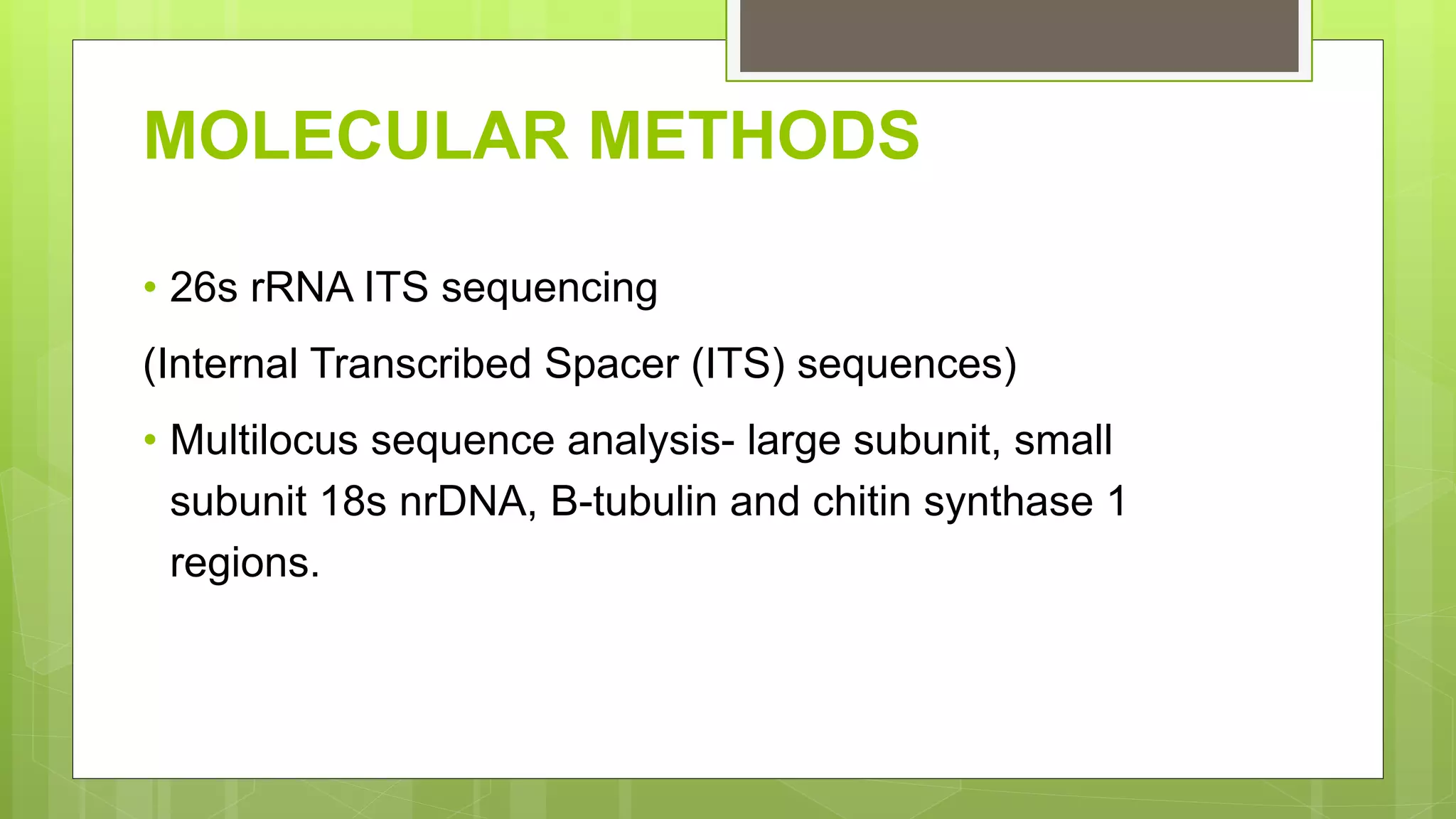
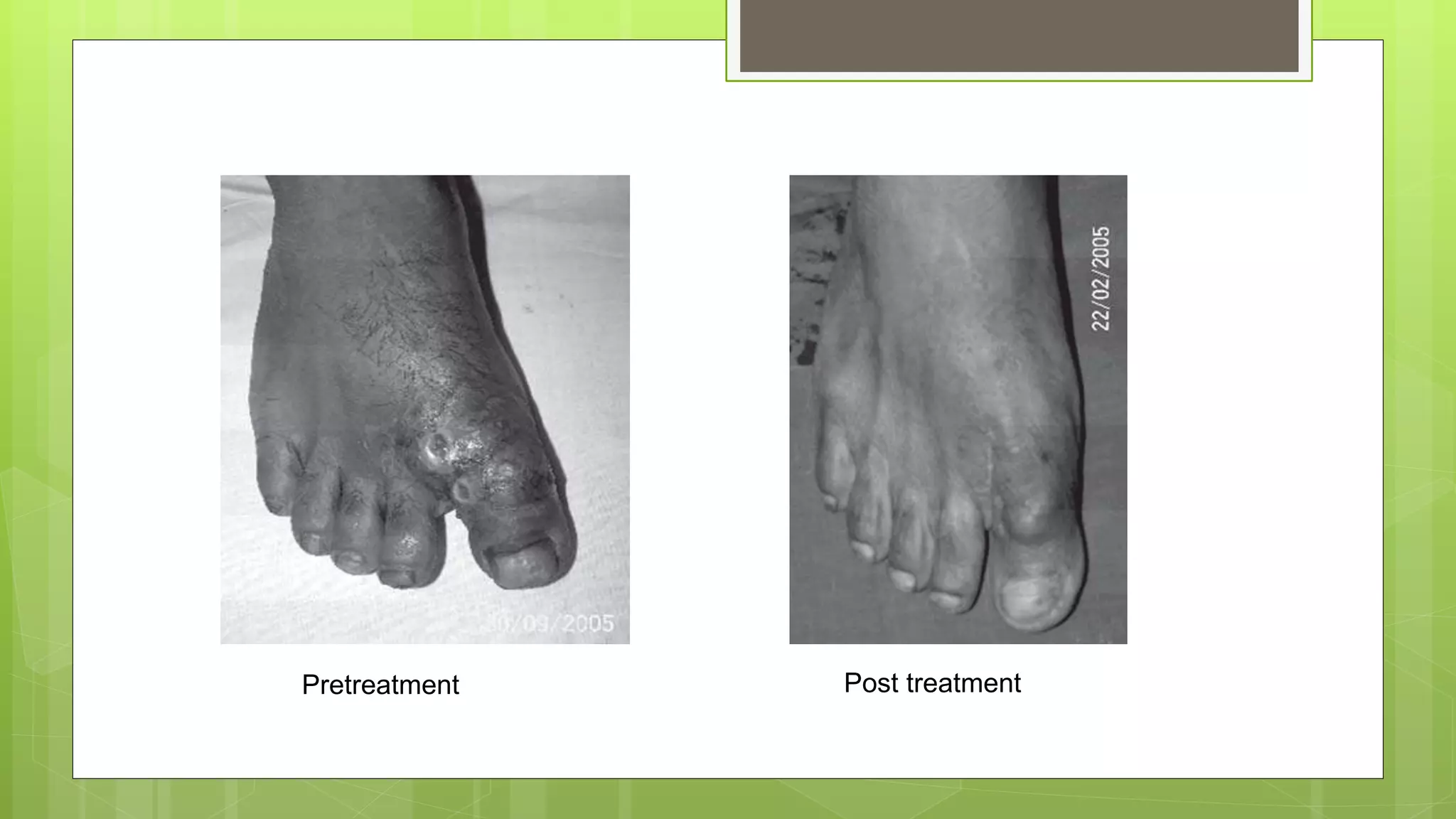
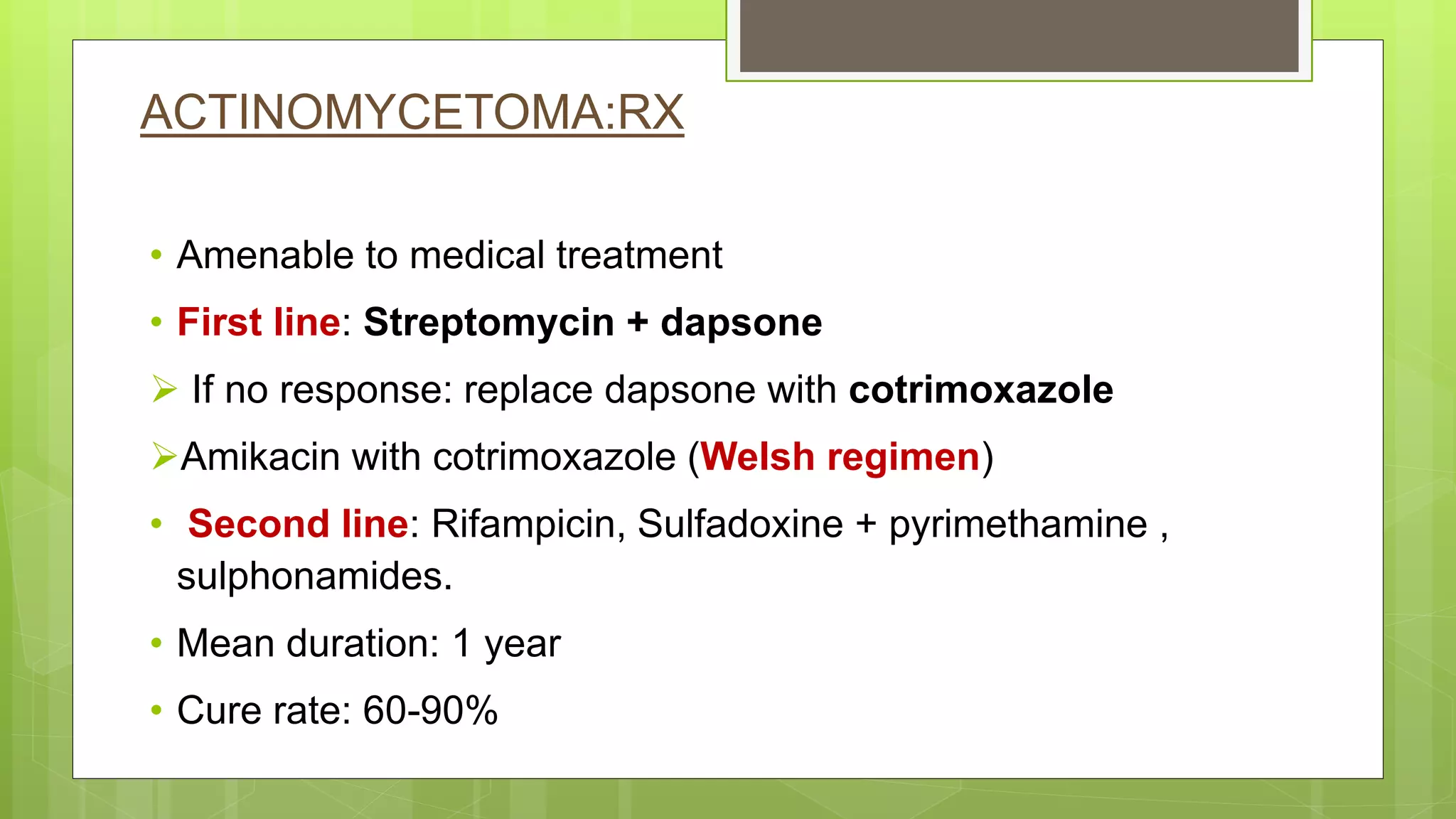
This document provides an overview of mycetoma, including its history, classification, epidemiology, etiology, pathogenesis, clinical manifestation, diagnosis, treatment and prevention. Mycetoma is a localized swelling that contains granulomas and abscesses which drain through sinus tracts, involving skin, subcutaneous tissue, fascia and bone. It is classified into eumycetomas caused by fungi and actinomycetomas caused by actinomycetes. Diagnosis involves microscopic examination of grains from sinus tracts and cultures. Treatment depends on the classification and involves antibiotics, antifungals, surgery or a combination. Prevention focuses on reducing traumatic inoculation and early treatment.