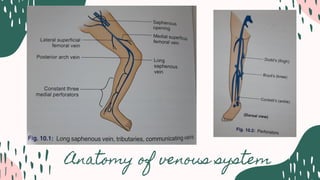
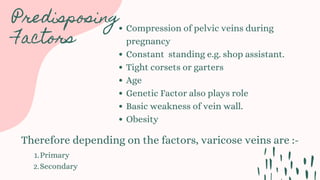
Varicose veins are dilated and tortuous superficial veins caused by incompetent valves, influenced by factors like age, genetics, and obesity. They can be classified as primary, due to congenital issues, or secondary, due to other conditions such as pregnancy or tumors. Management includes conservative treatments like compression and physiotherapy, as well as surgical options for severe cases.