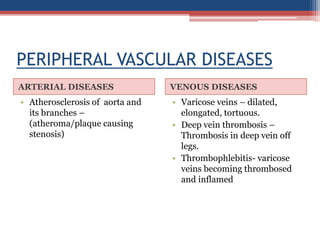
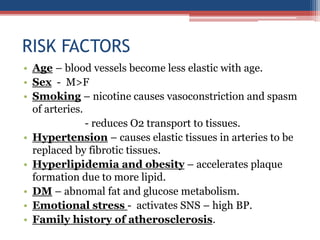
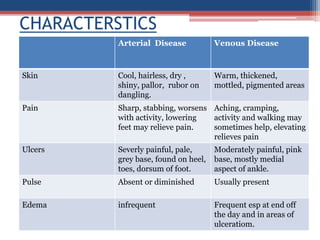
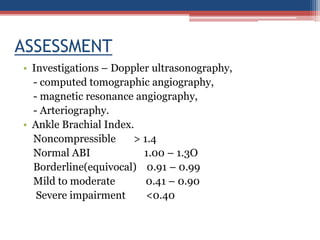
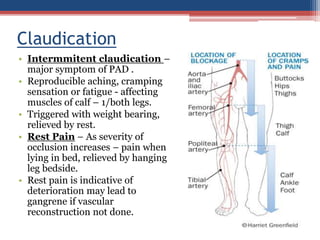
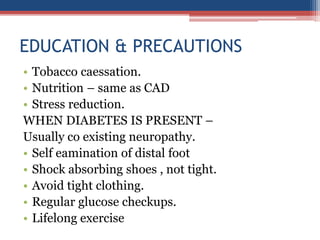
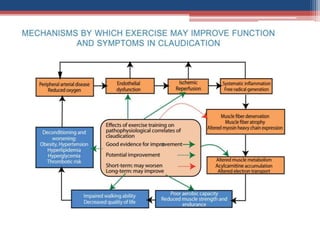
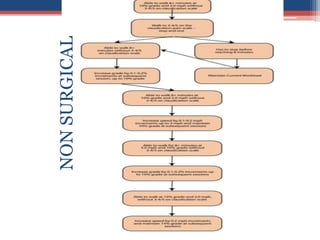
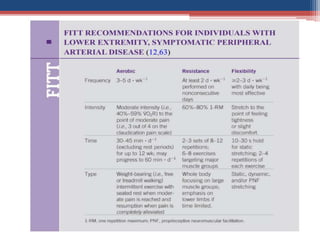
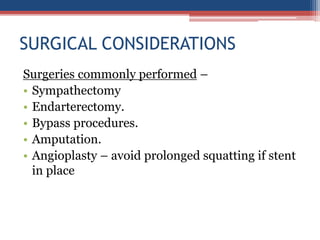
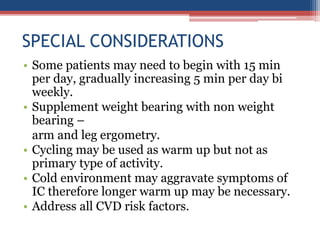
Peripheral vascular disease (PAD) involves reduced blood flow and oxygen through peripheral vessels, potentially leading to ischemia and necrosis. Key risk factors include age, smoking, hypertension, and diabetes, with symptoms differing between arterial and venous diseases. Assessment methods include Doppler ultrasonography and the ankle-brachial index, while treatment options range from lifestyle changes to surgical interventions.