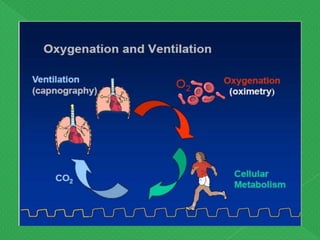
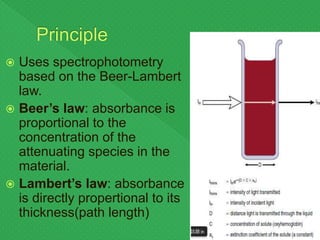
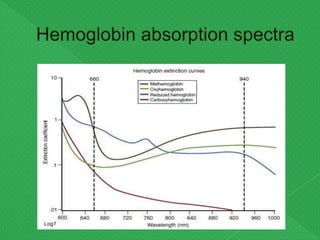
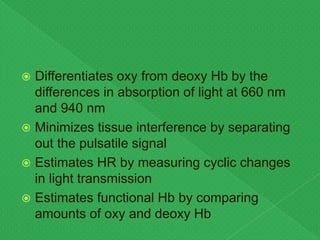
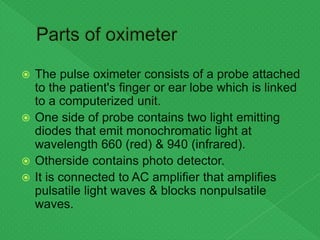
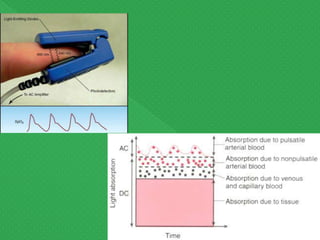
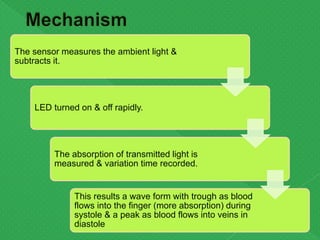
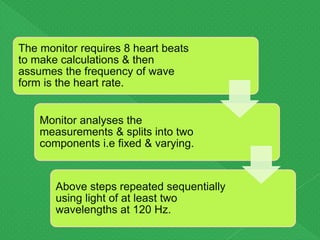
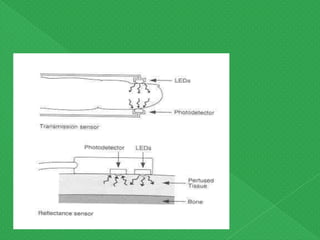
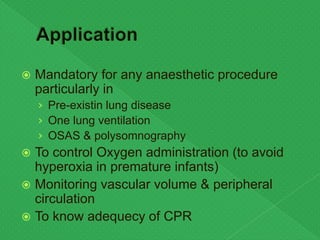
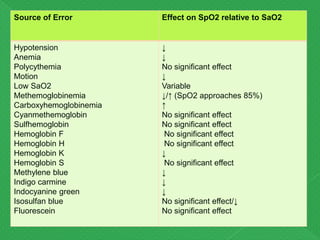
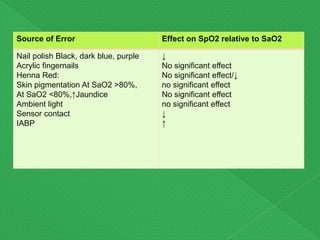
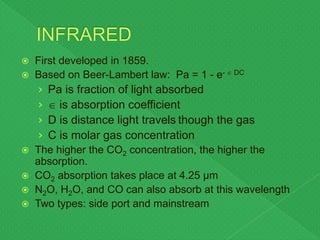
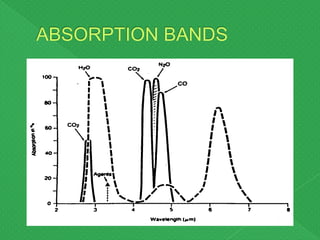
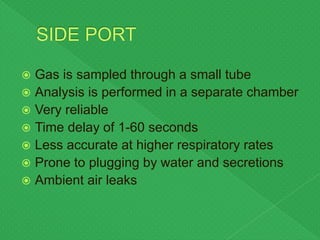
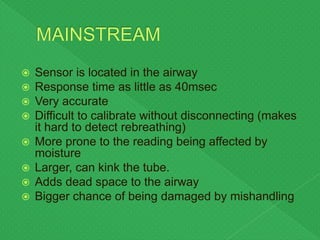
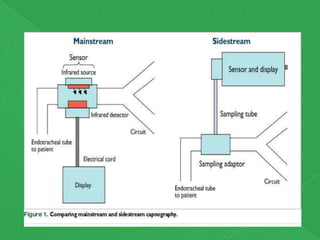
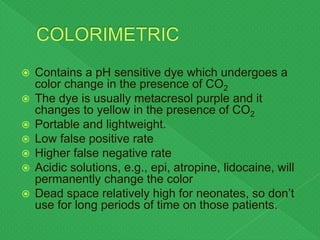
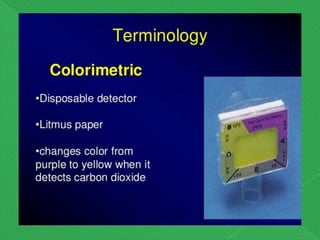
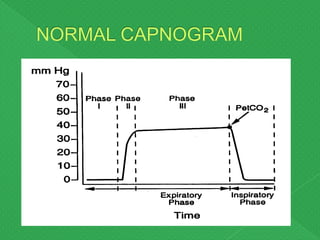
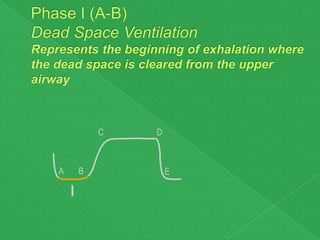
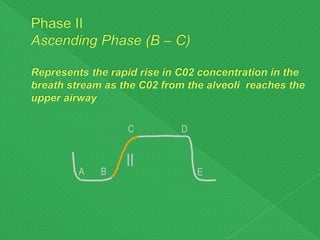
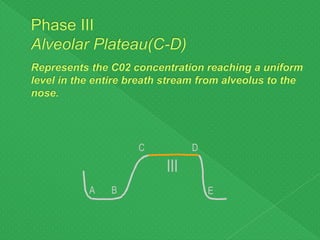
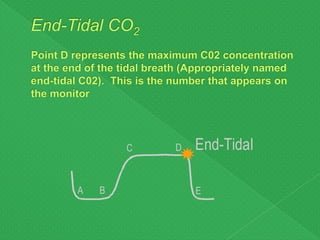
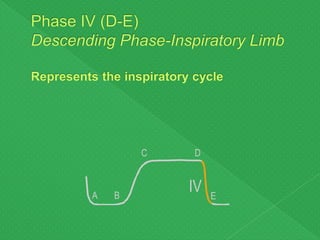
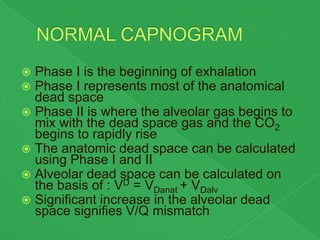
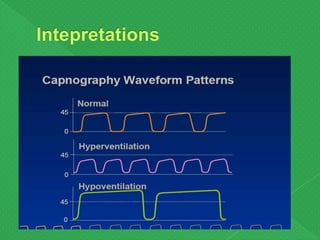
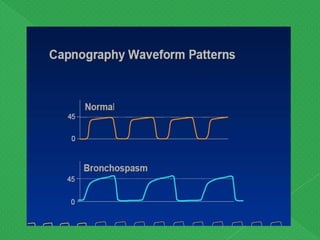
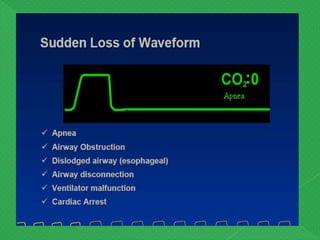
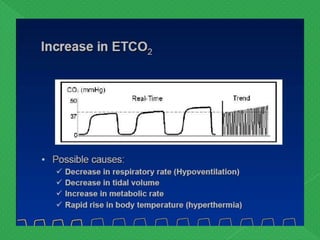
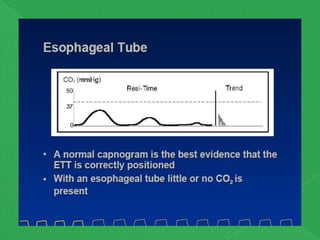
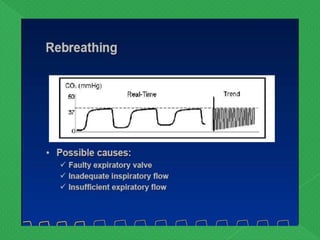
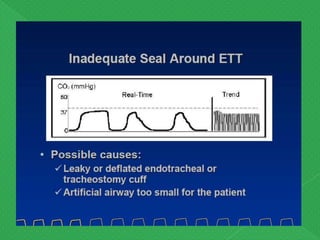
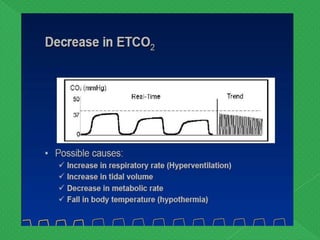
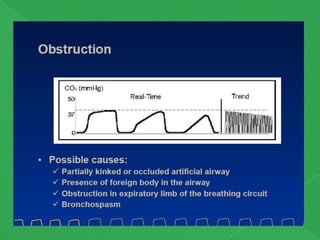
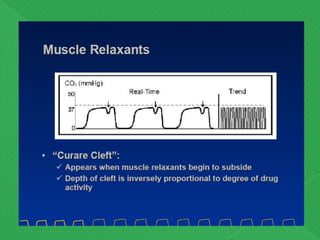
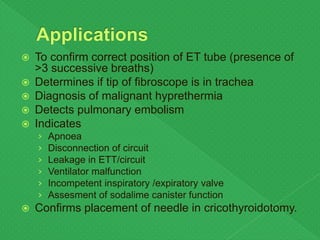
The document discusses pulse oximetry and capnography. Pulse oximetry uses light absorption to non-invasively measure arterial oxygen saturation by comparing absorbed and transmitted light through tissues at red and infrared wavelengths. It can detect hypoxemia but is influenced by other factors like skin pigment. Capnography measures exhaled carbon dioxide concentration using infrared absorption, with the capnogram tracing showing phases that can assess ventilation and oxygenation status. Both are important monitoring tools during medical procedures.