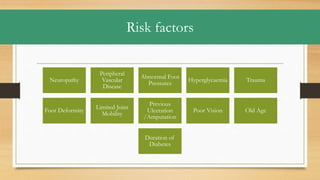
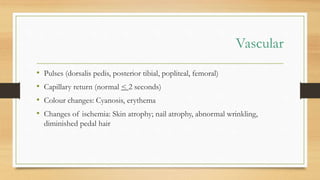
Diabetic foot ulcers are non-healing or poorly healing skin breaks below the ankle in diabetic individuals, caused by factors such as neuropathy and vascular disease. Evaluation includes assessing the ulcer's characteristics, vascular and neurological status, and relevant imaging, while management combines operative and non-operative strategies including debridement, wound care, and infection control. Prevention focuses on education, foot care, and a multidisciplinary approach to minimize risks and complications.