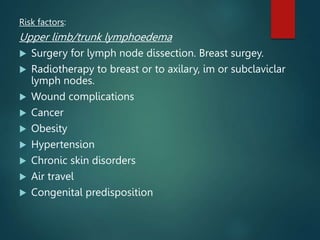
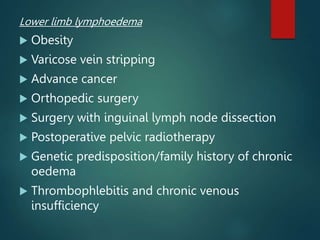
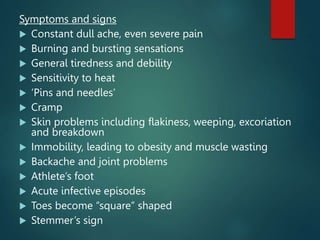
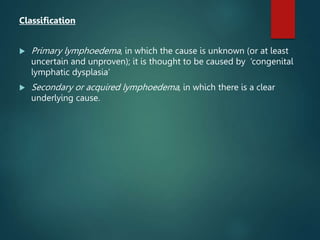
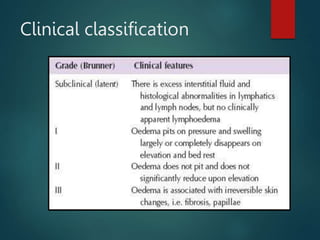
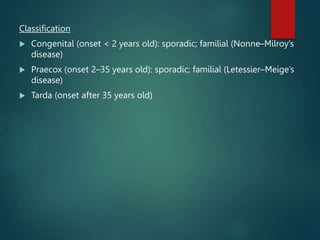
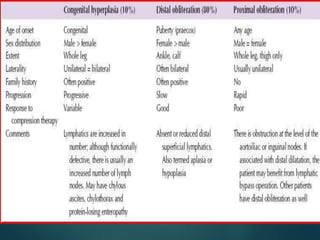
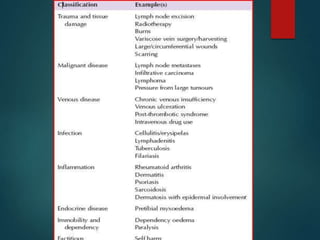
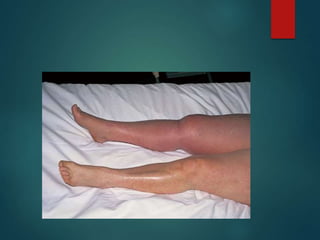
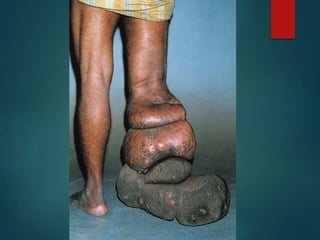
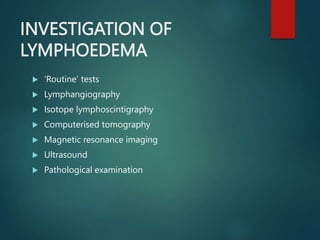
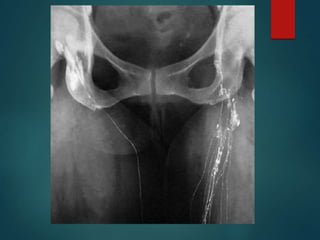
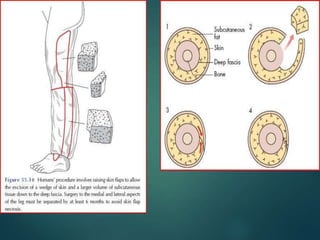
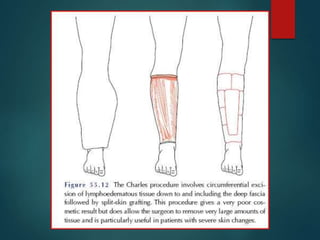
Lymphoedema is characterized by abnormal limb swelling due to high protein interstitial fluid accumulation and defective lymphatic drainage, with various risk factors including surgery, obesity, and cancer. It can be classified into primary lymphoedema, often hereditary, and secondary lymphoedema, arising from identifiable causes like infection or trauma. Management includes decongestive lymphoedema therapy, which consists of skin care, manual drainage, and compression, with surgical options available for a small minority of cases.