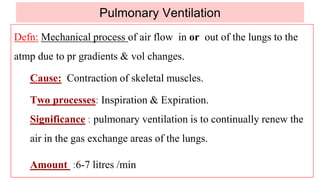
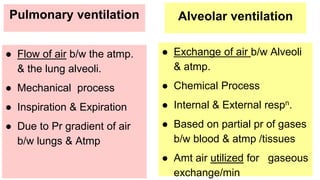
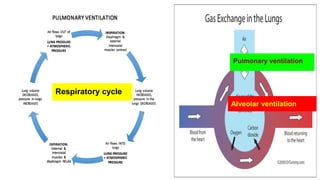
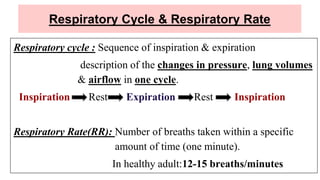
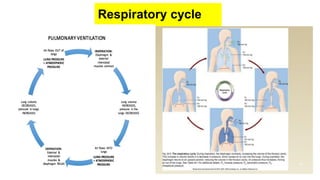
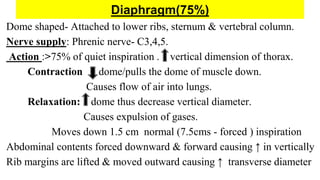
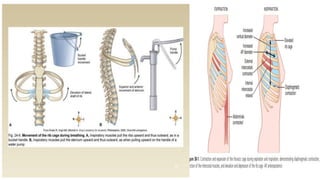
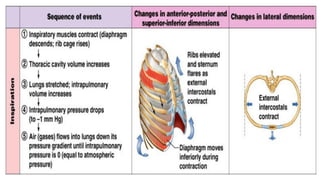
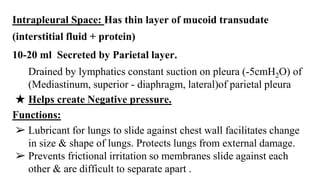
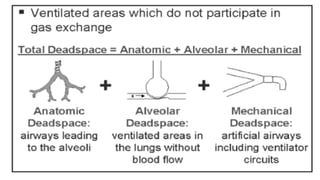
Pulmonary ventilation is the mechanical process of air flowing in and out of the lungs due to pressure gradients and volume changes caused by contraction of respiratory muscles during inspiration and expiration. It serves to continually renew the air in the gas exchange areas of the lungs. In a healthy adult, pulmonary ventilation is approximately 6-7 liters per minute through tidal breathing of 500ml 12 times per minute, resulting in alveolar ventilation of around 4200ml per minute after accounting for the 150ml dead space. Pulmonary ventilation, alveolar ventilation, respiratory cycles, and the mechanics of respiration including respiratory muscles, pleural pressures, and pressure relationships are discussed in detail.