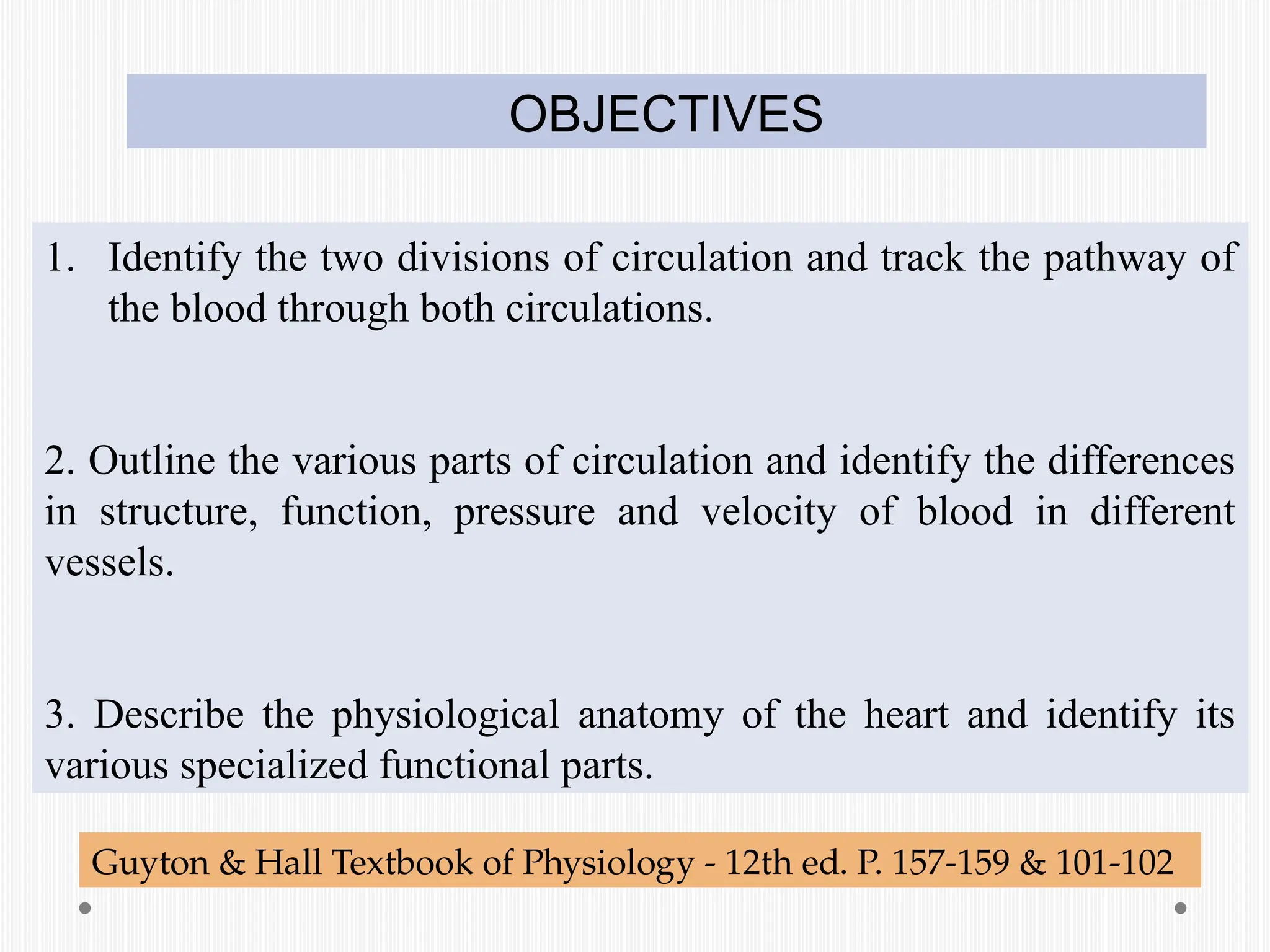
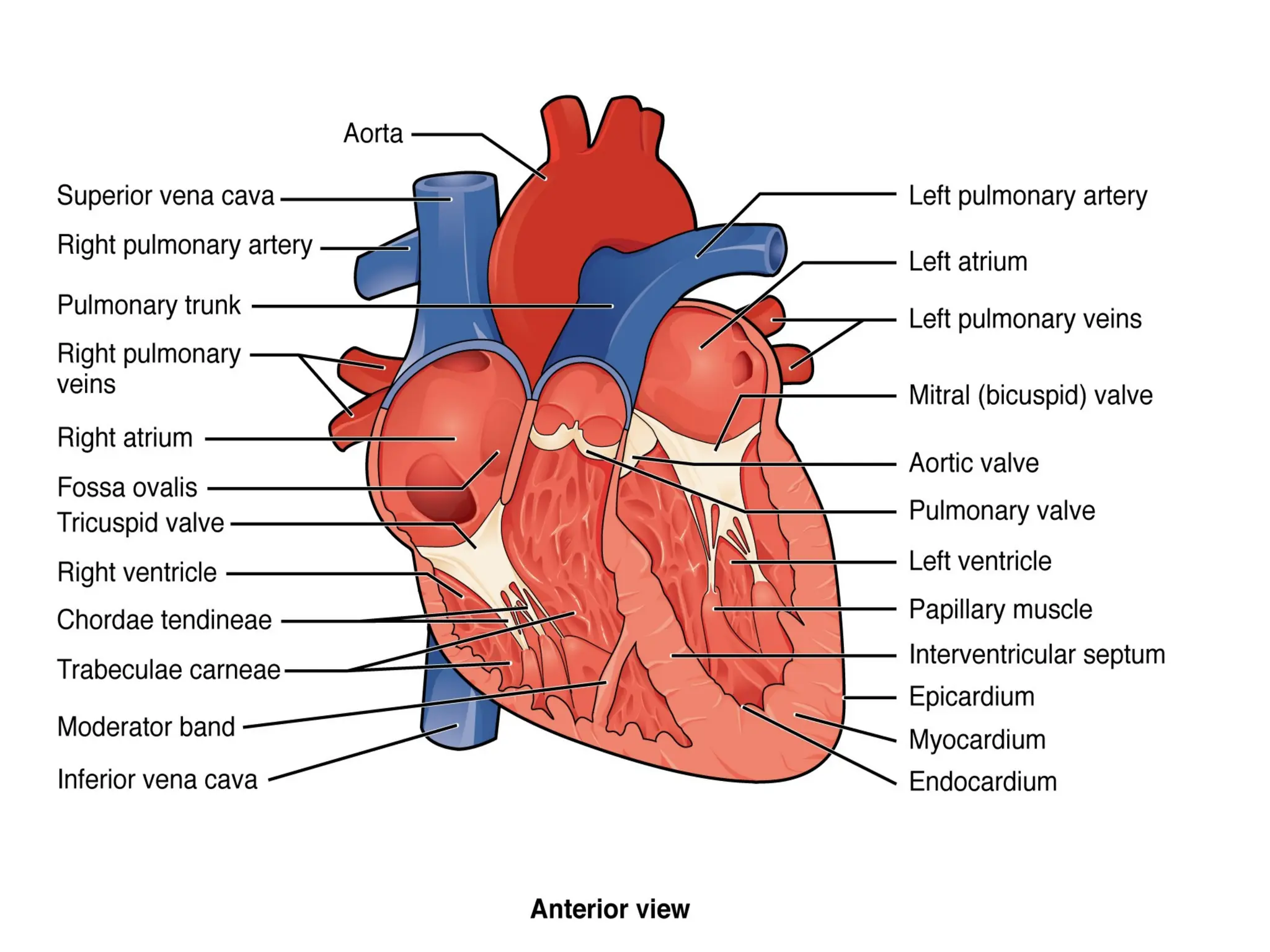
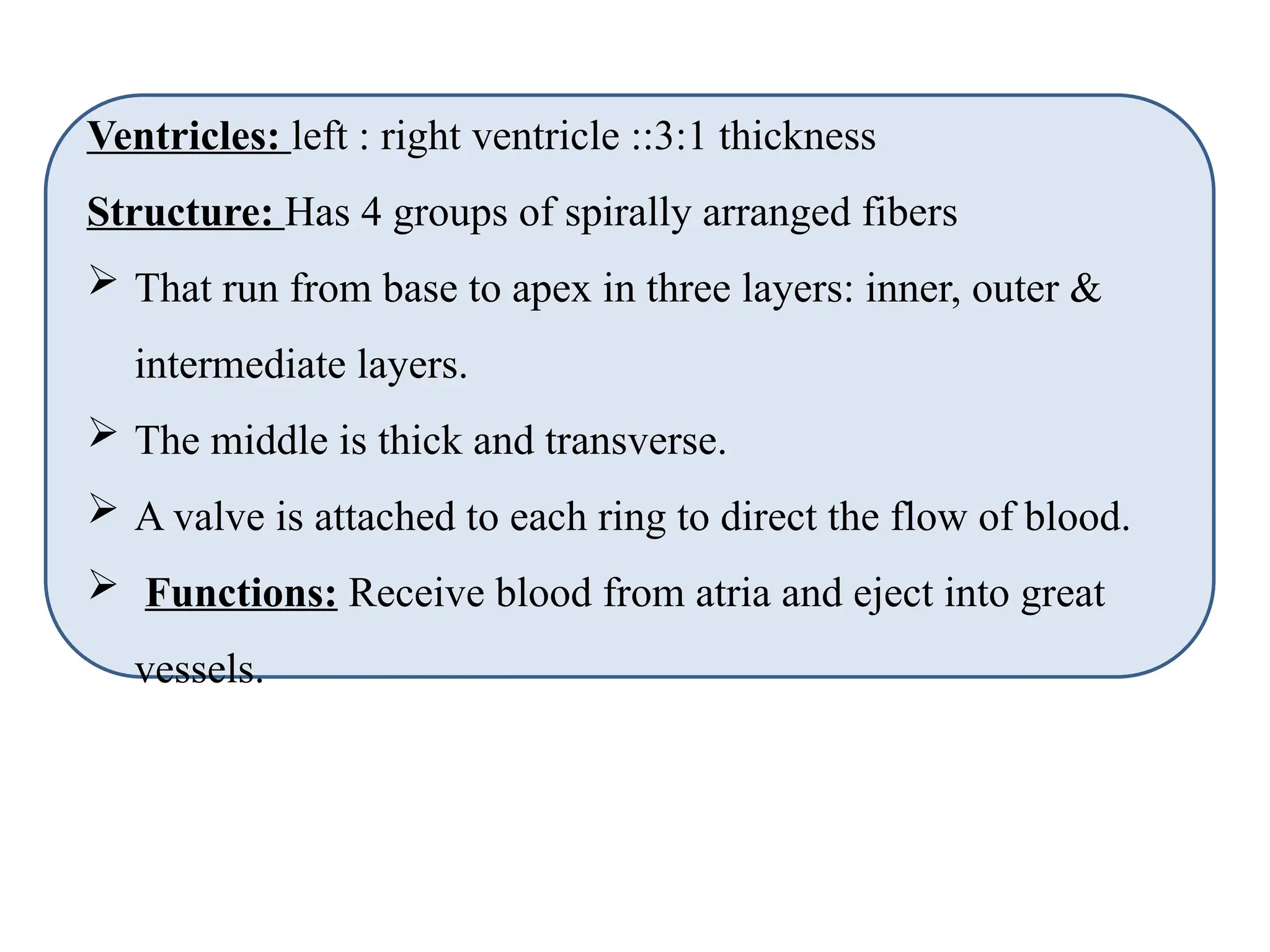
This document provides an overview of the circulatory system, including its major components such as the heart, blood vessels, and their functions in nutrient and waste transport. It discusses the differences between arteries and veins, the anatomy of the heart, and the specific roles of various types of blood vessels in circulation. Additionally, it covers the structure and function of cardiac muscle and the conduction system that regulates heartbeats.
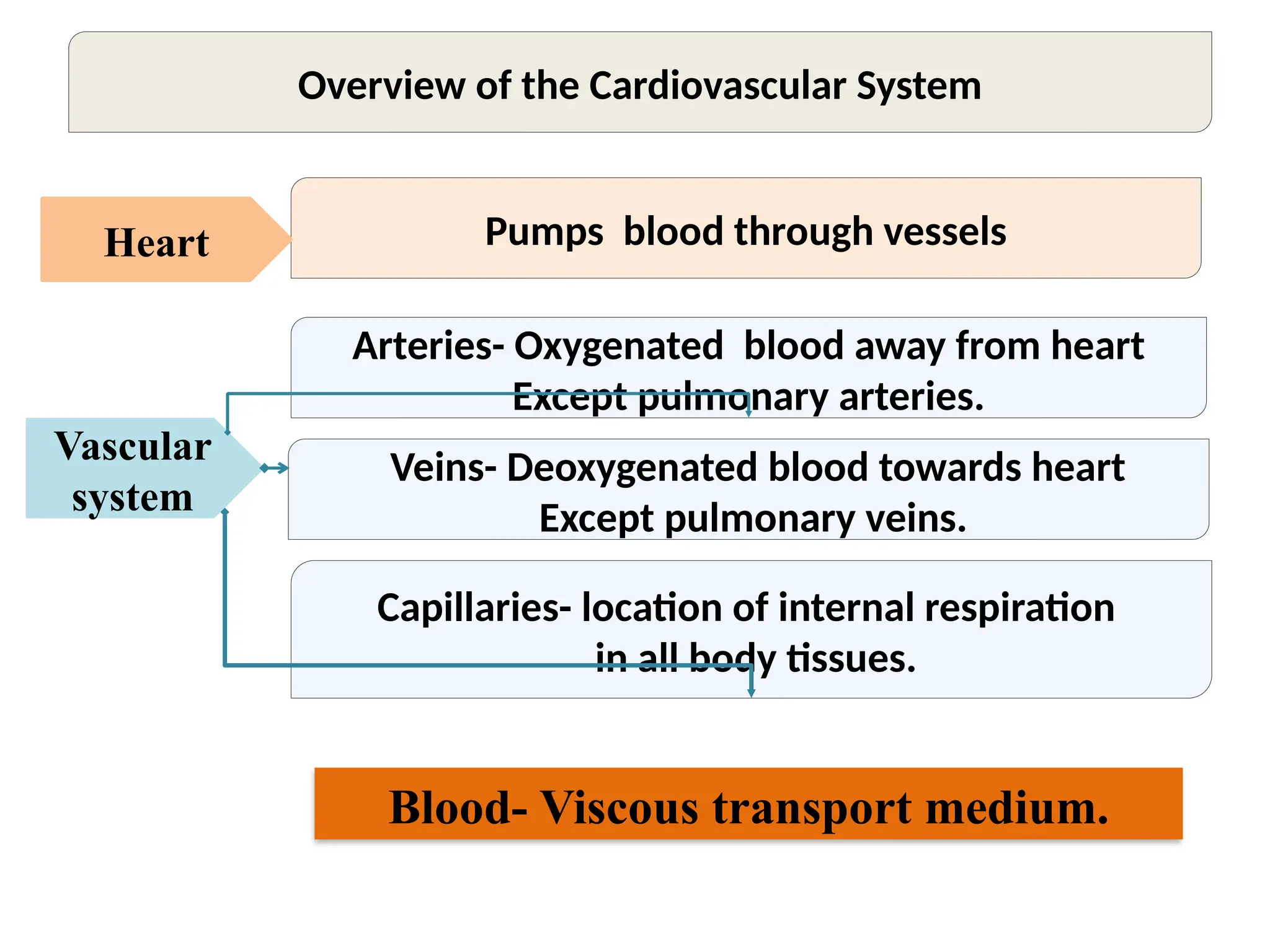
![Functions of Heart
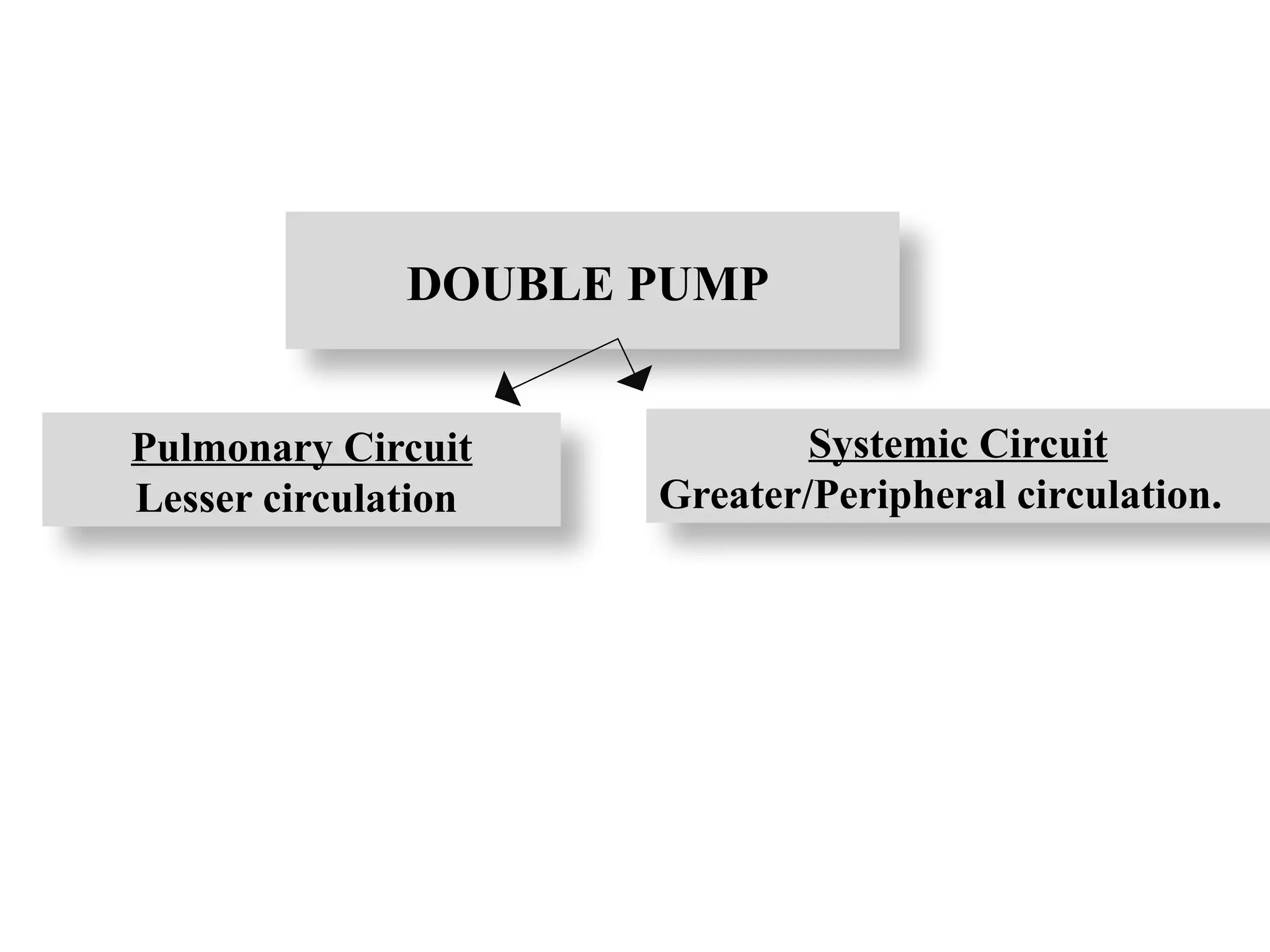
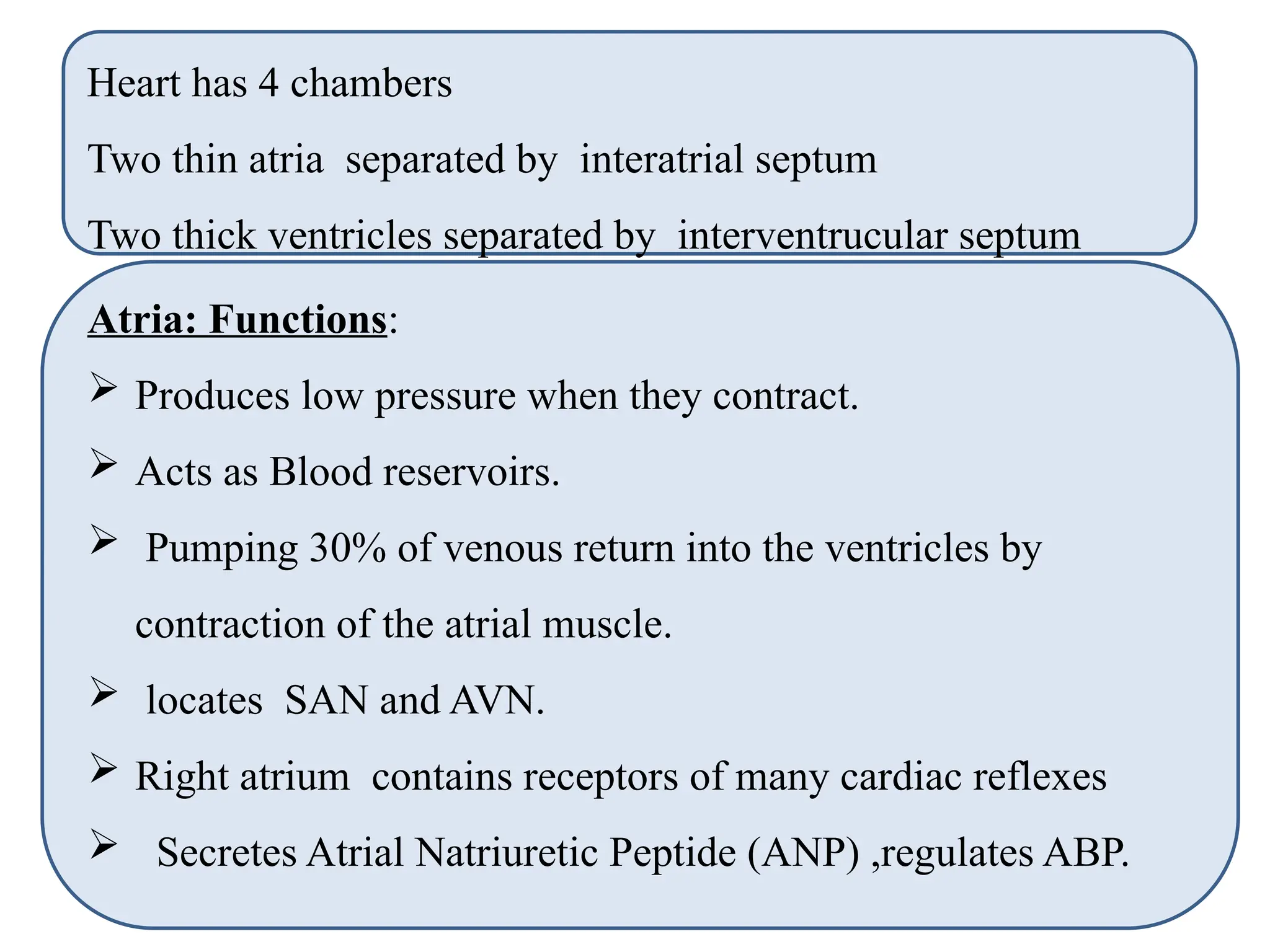
Generating blood pressure.
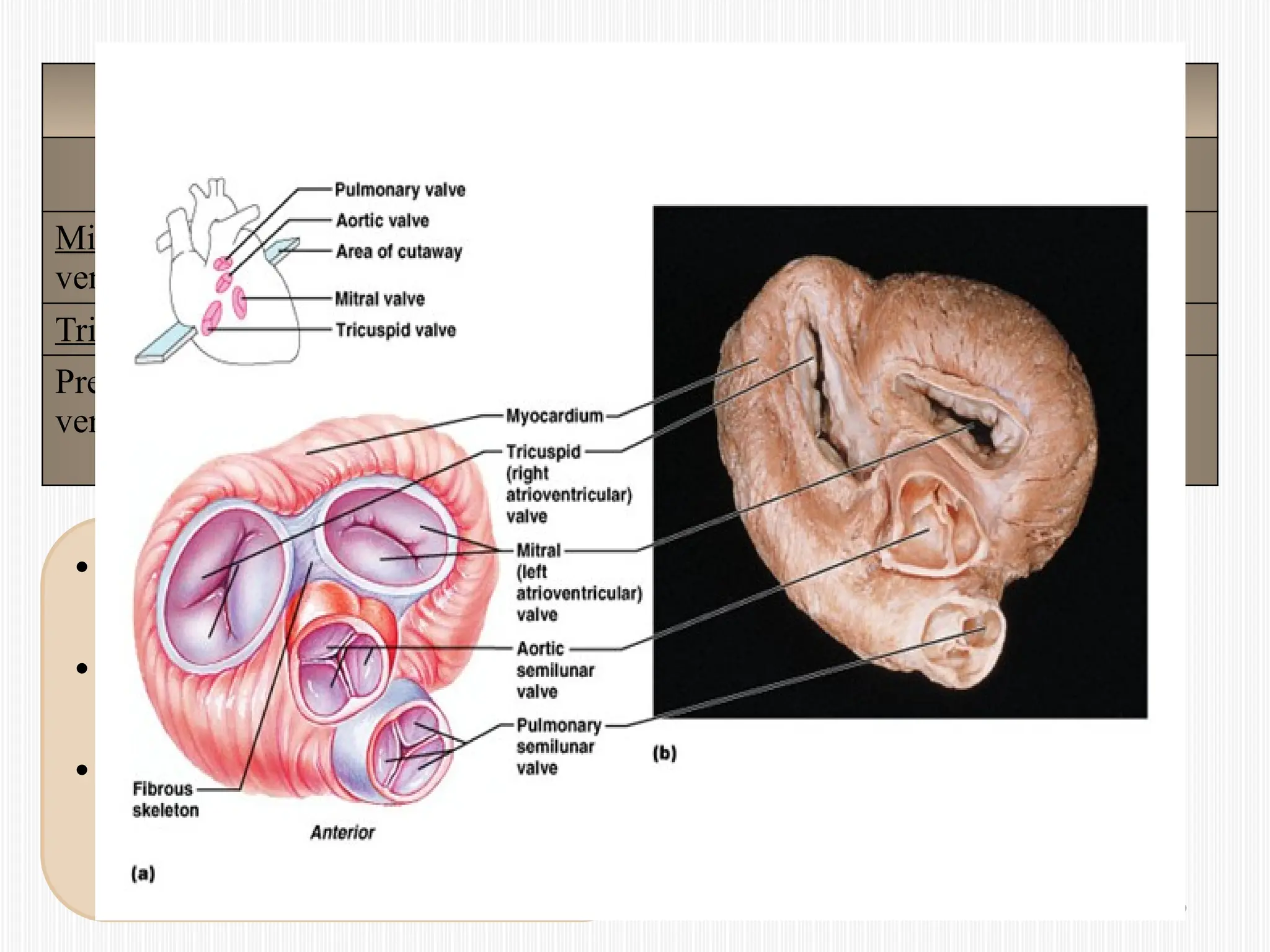
Ensuring one-way blood flow: with help of valves
Routing blood: separates pulmonary and systemic
circulations.
Regulating blood supply according to the need of the
body [increase in exercise & pregnancy..].](https://image.slidesharecdn.com/ultimateintroductionofcvslecture2020-240903185831-5cef914d/75/Lecture-Introduction-of-cardiovascular-system-5-2048.jpg)
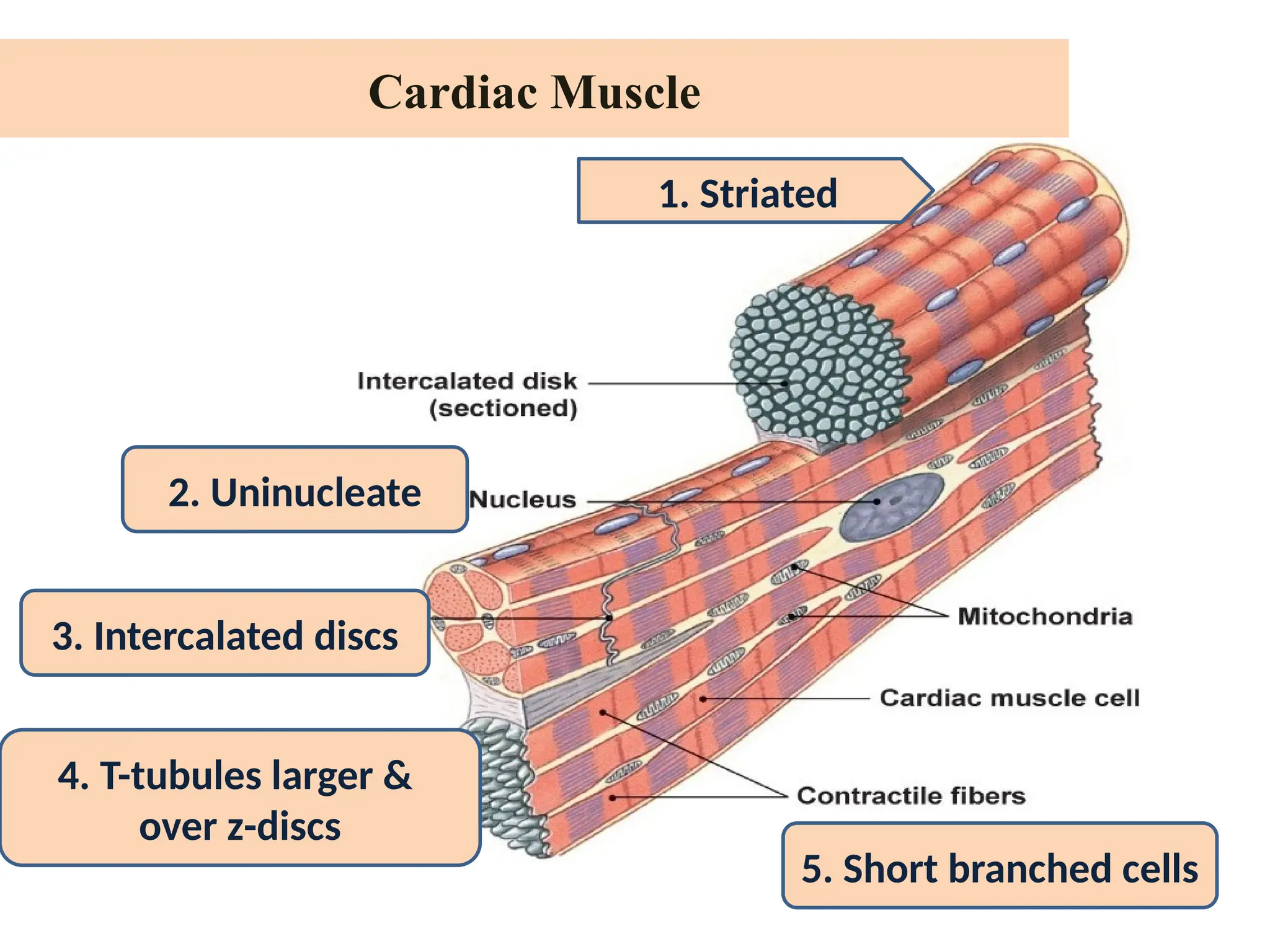
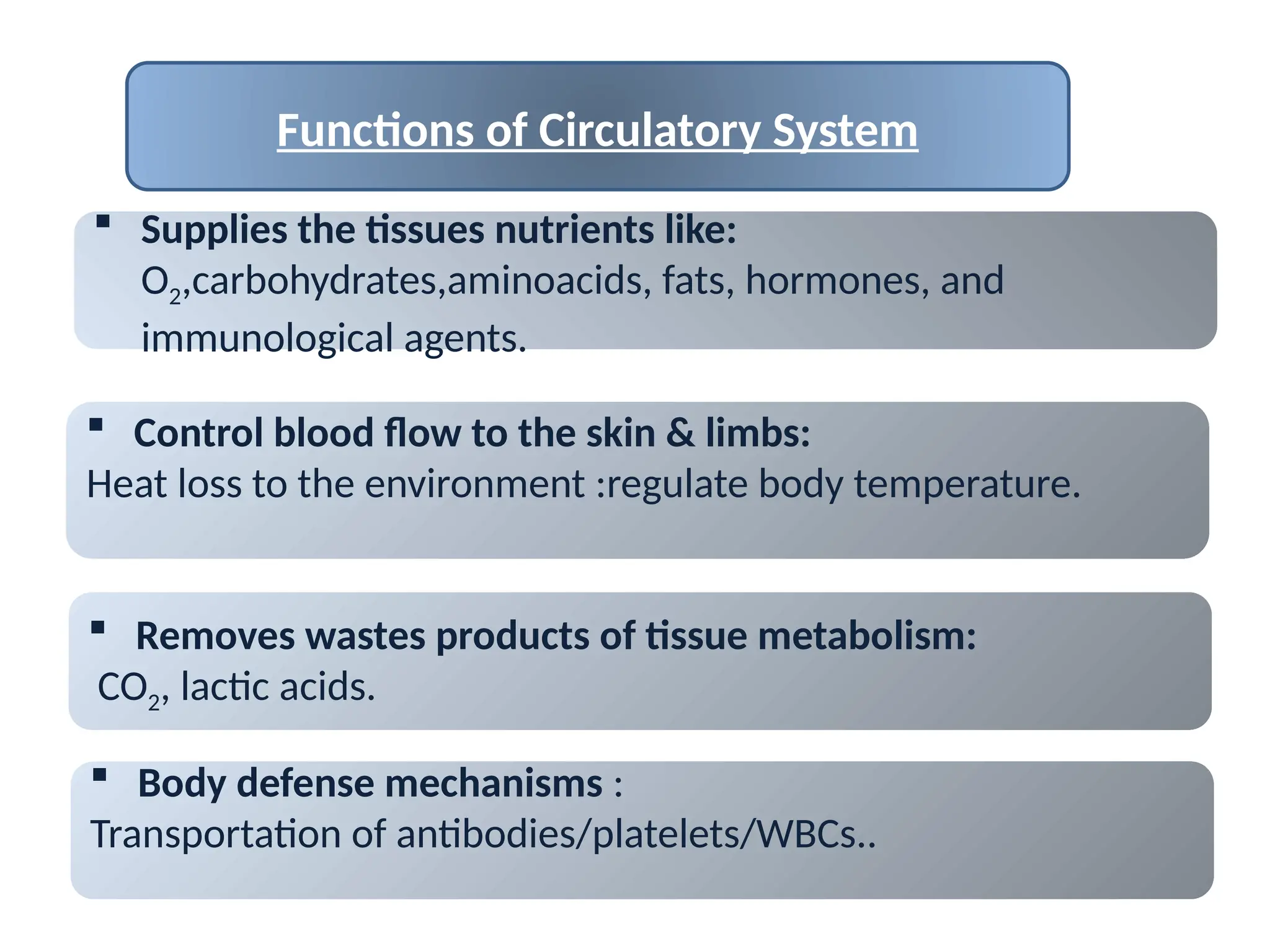
![Intercalated disc: The cell membranes fuse with one another to
form permeable “communicating” junctions (gap junctions).
Function: Allow rapid diffusion of ions.
Cardiac muscle: Syncytium of many heart muscle cells
Function: when one cell gets excited, the action potential rapidly
spreads to all of cardiac cells.
Two syncytiums: Atrial syncytium [the walls of the two atria]
Ventricular syncytium [ two ventricles].
Purpose of syncytiums: Allows the atria to contract a short time
ahead of ventricular contraction, which is important for
effectiveness of heart pumping.](https://image.slidesharecdn.com/ultimateintroductionofcvslecture2020-240903185831-5cef914d/75/Lecture-Introduction-of-cardiovascular-system-22-2048.jpg)