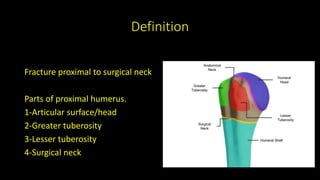
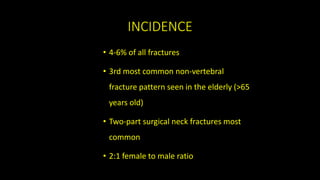
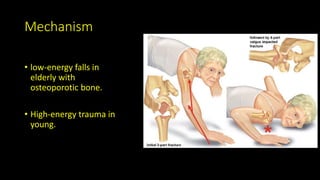
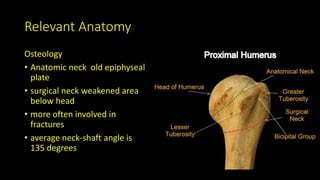
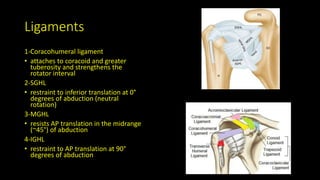
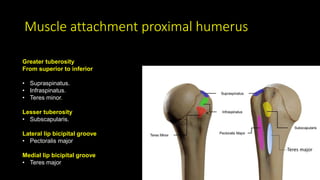
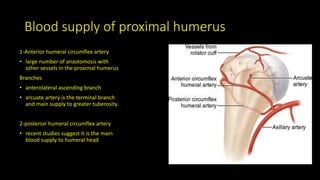
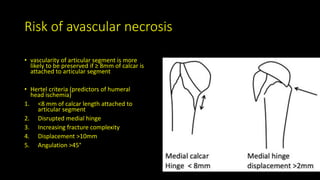
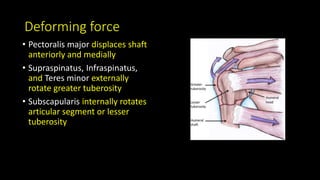
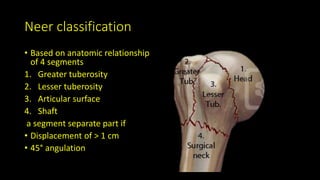
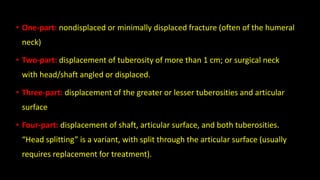
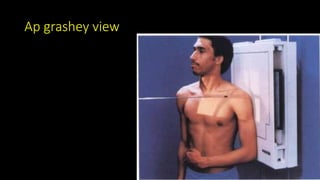
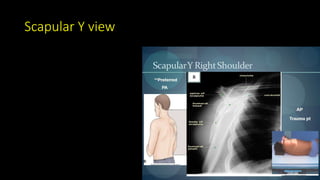
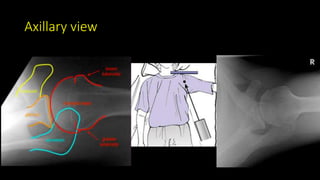
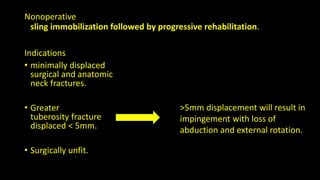
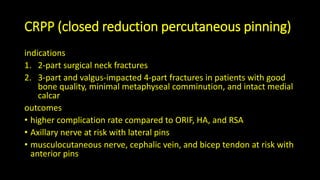
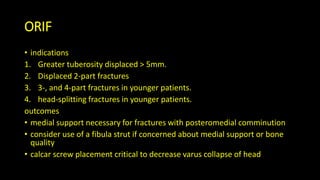
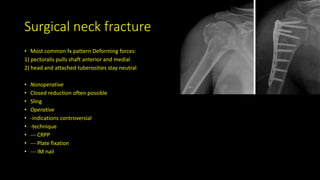
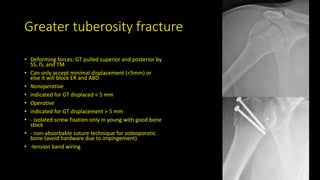
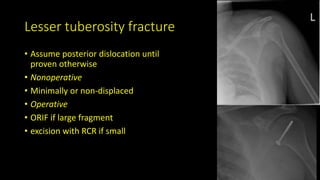
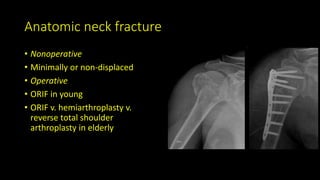
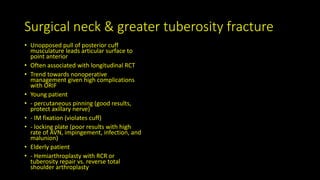
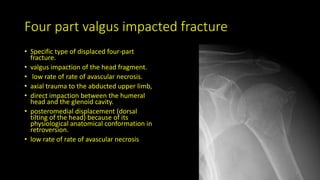
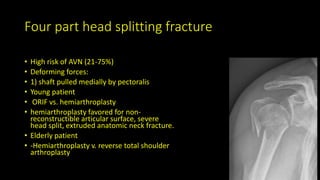
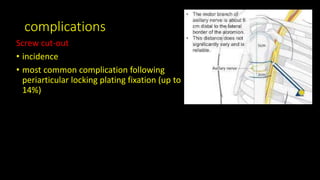
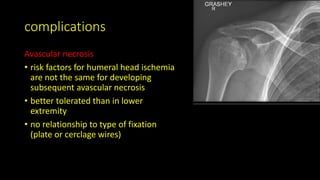
The document discusses proximal humerus fractures, detailing their definition, incidence, risk factors, and relevant anatomy. It covers classification systems like the Neer classification, associated conditions, and surgical management approaches, including nonoperative and operative treatments. Complications and risks, including avascular necrosis and nerve injuries, are outlined, along with the implications for various patient demographics.