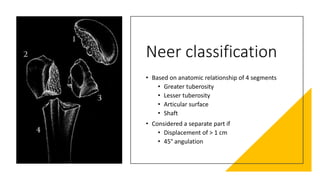
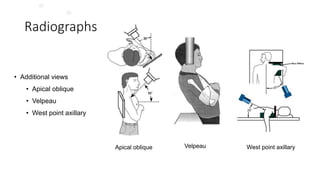
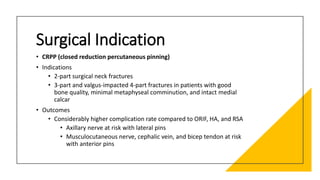
This document discusses classifications and treatment principles for fractures of the upper extremity, including the proximal humerus, clavicle, scapula, and acromioclavicular joint. It outlines the AO, Neer, and other classifications for proximal humerus fractures and describes treatment indications for closed reduction, open reduction internal fixation, arthroplasty, and other approaches. It also discusses classifications for clavicle shaft fractures, distal clavicle fractures, scapular fractures, and acromioclavicular joint injuries and notes surgical indications. Throughout, it emphasizes important radiographic views and parameters for evaluating these injuries.