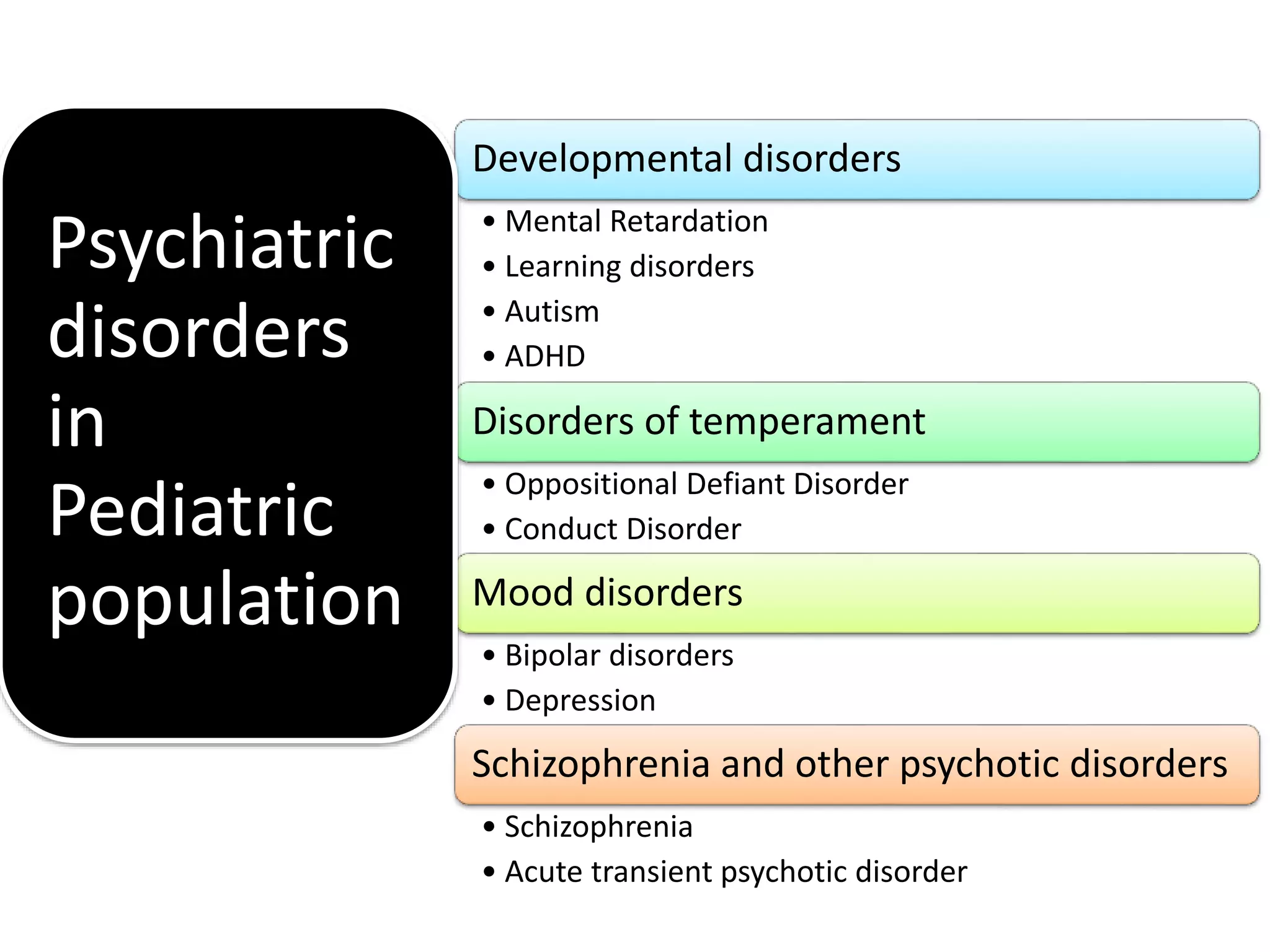
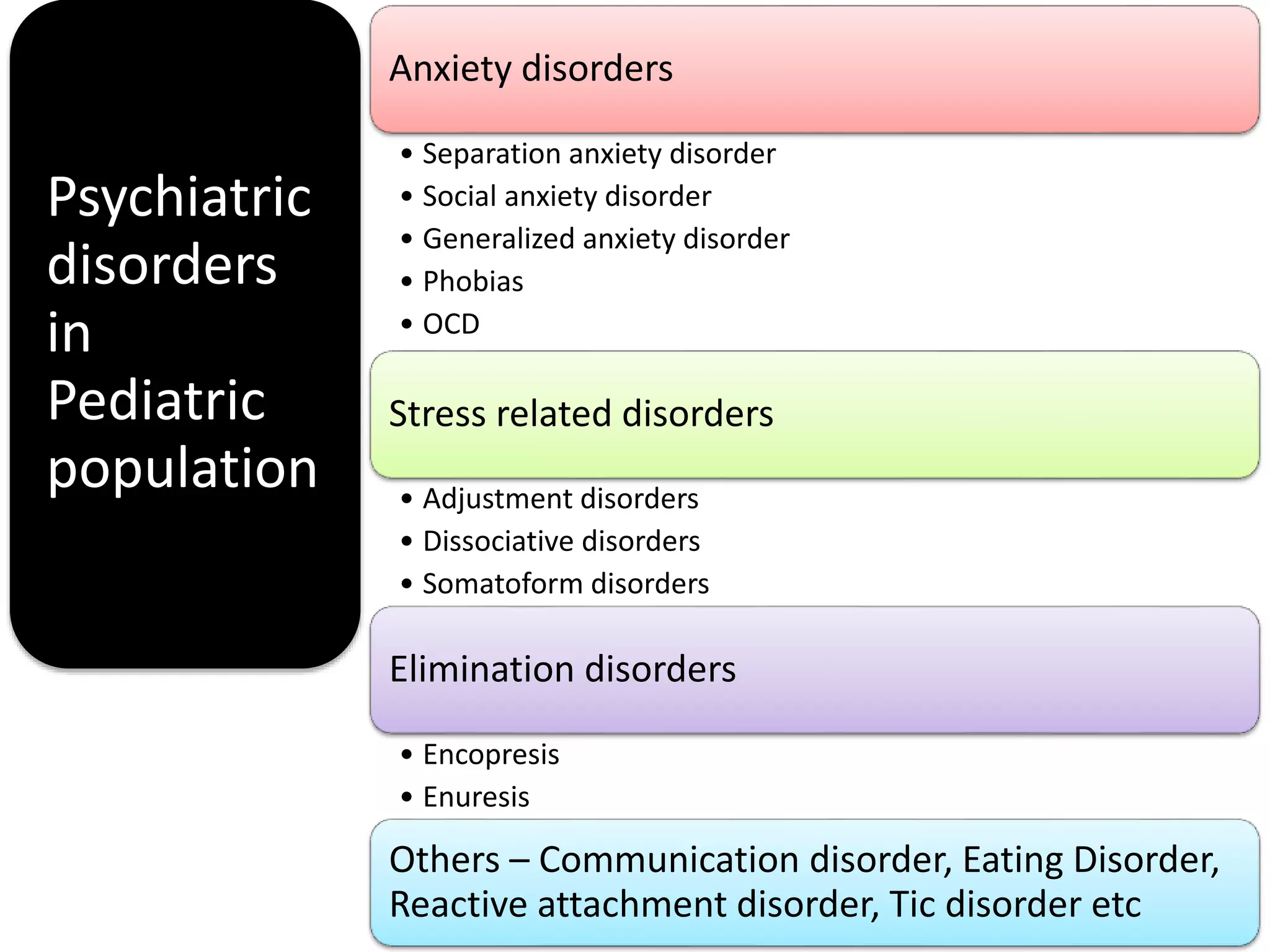
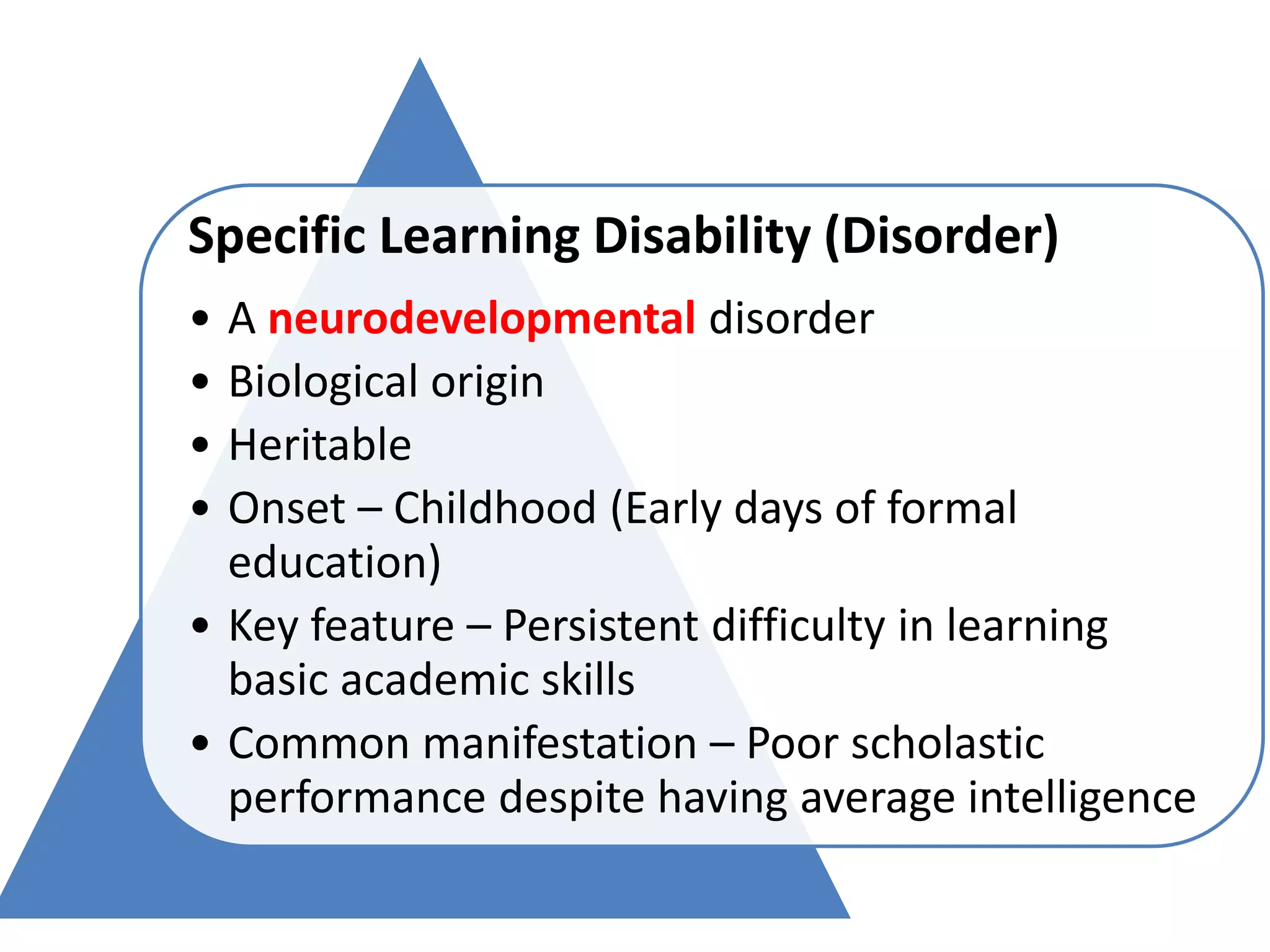
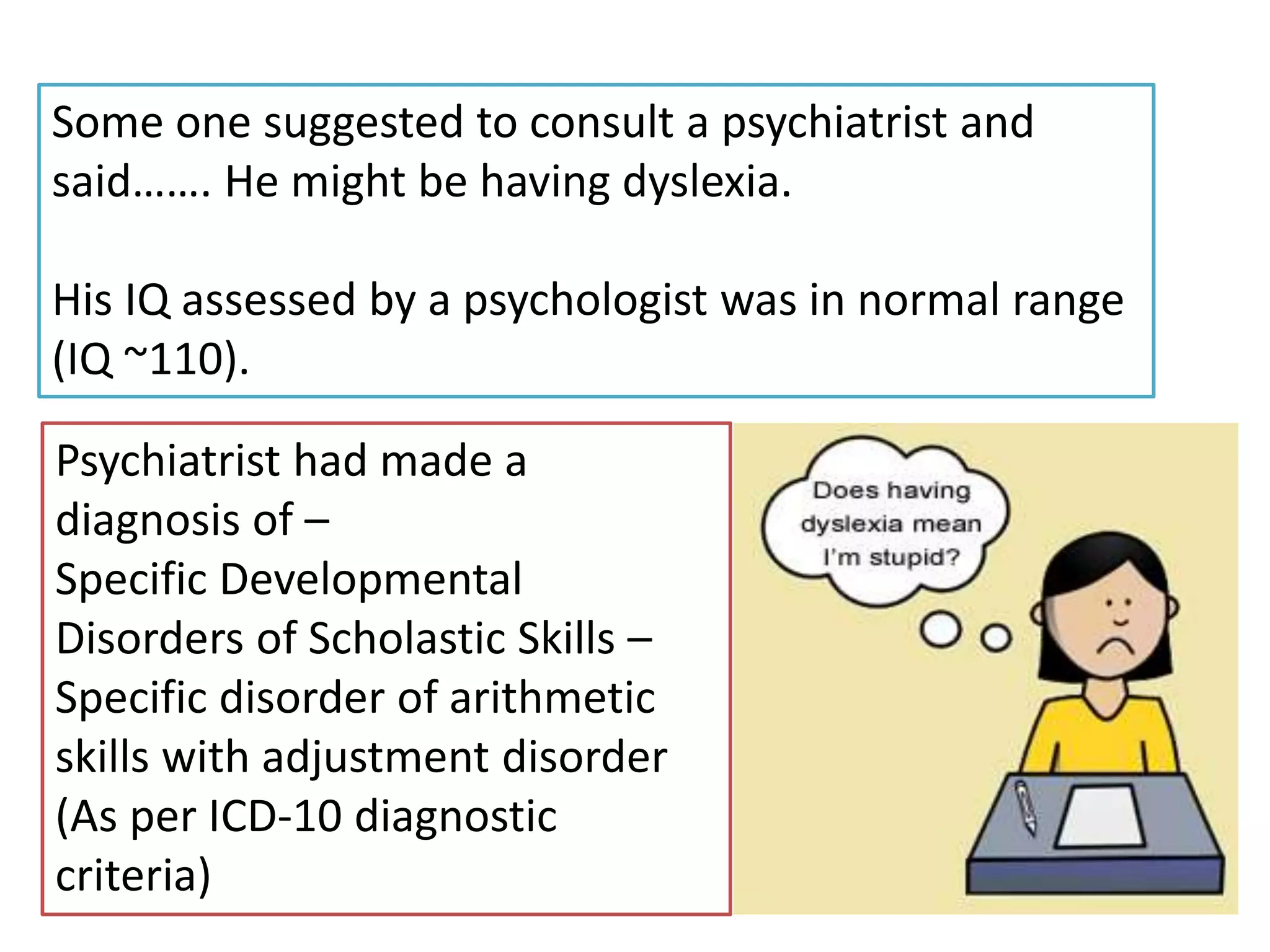
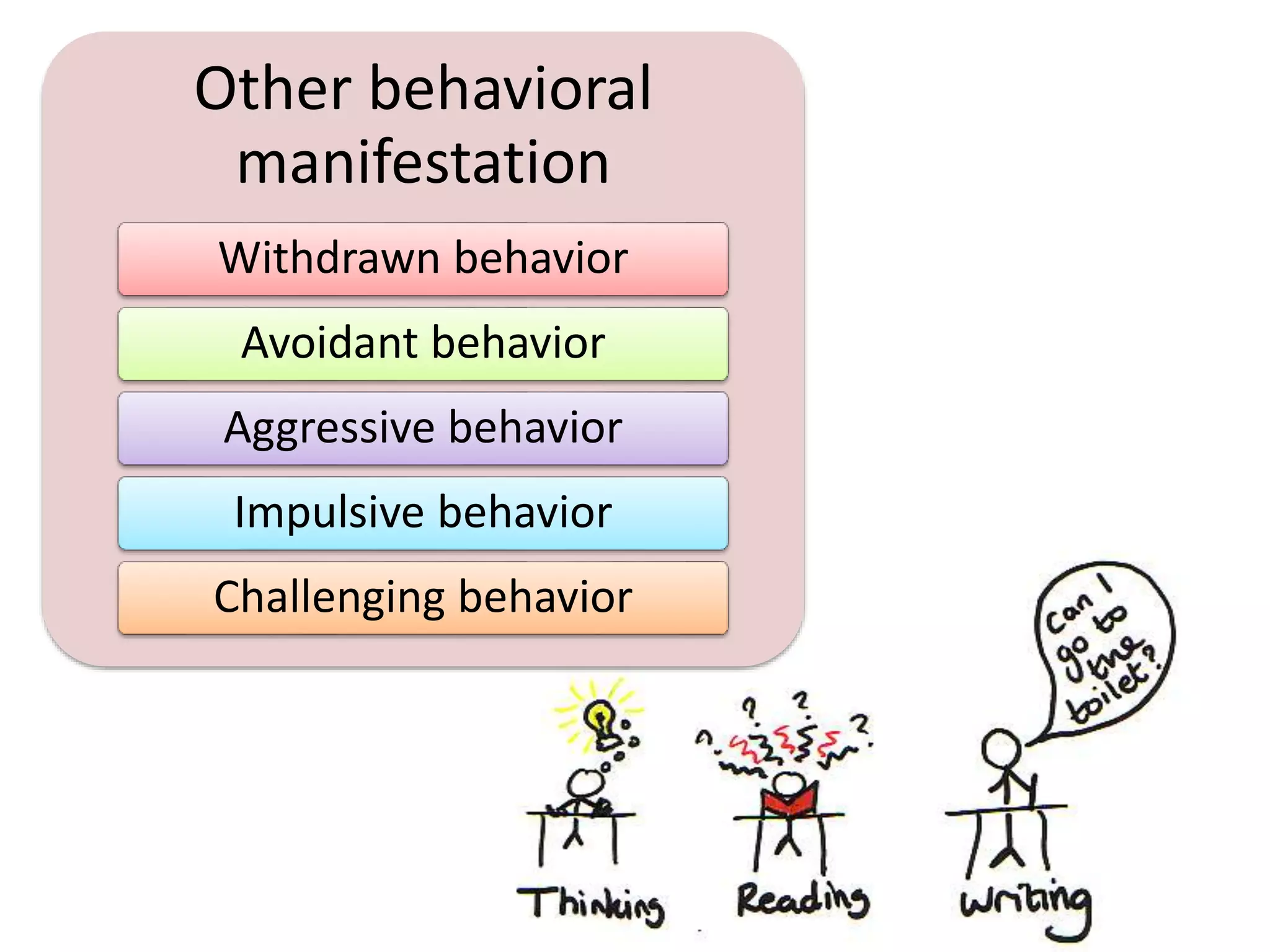
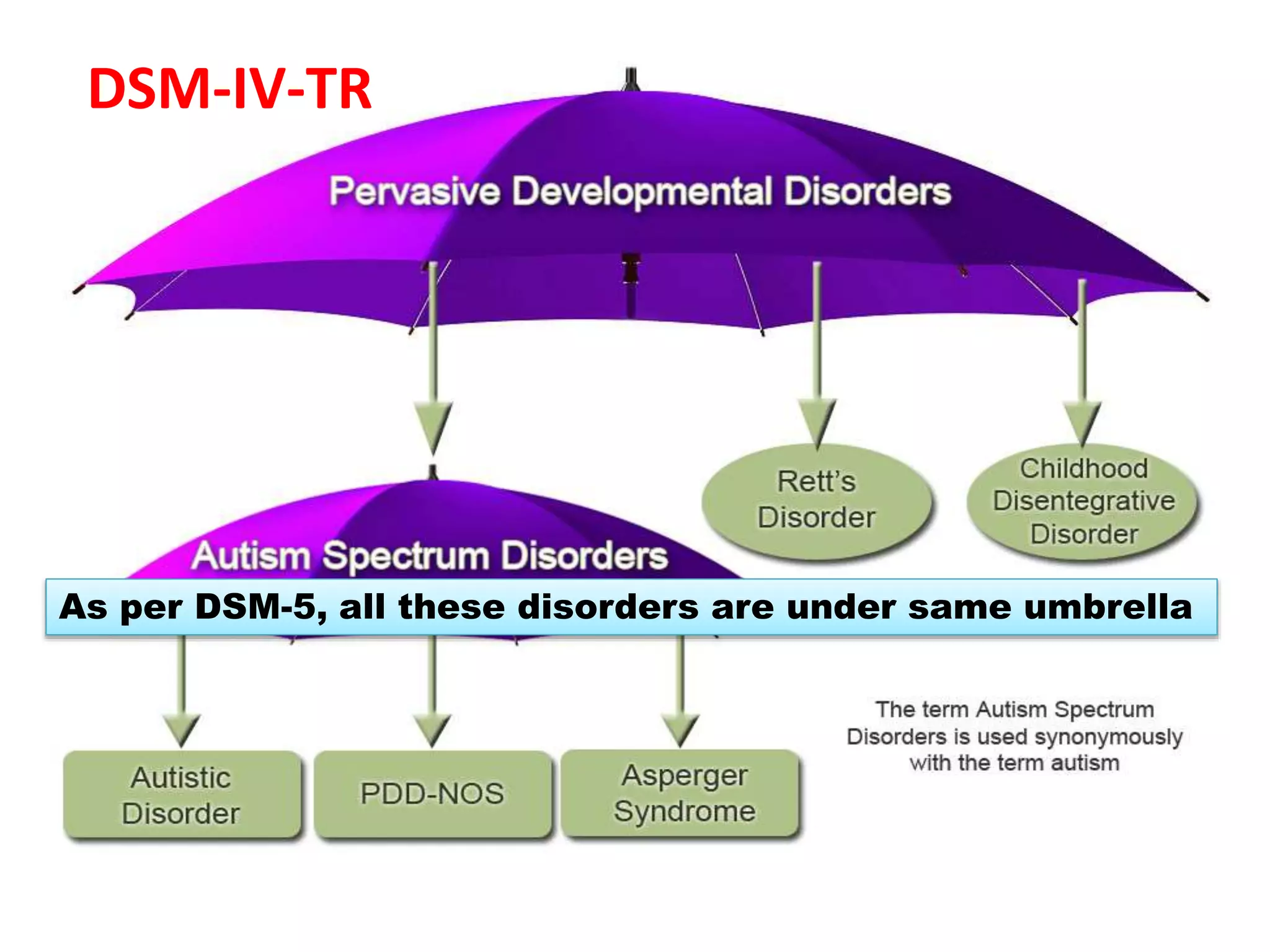
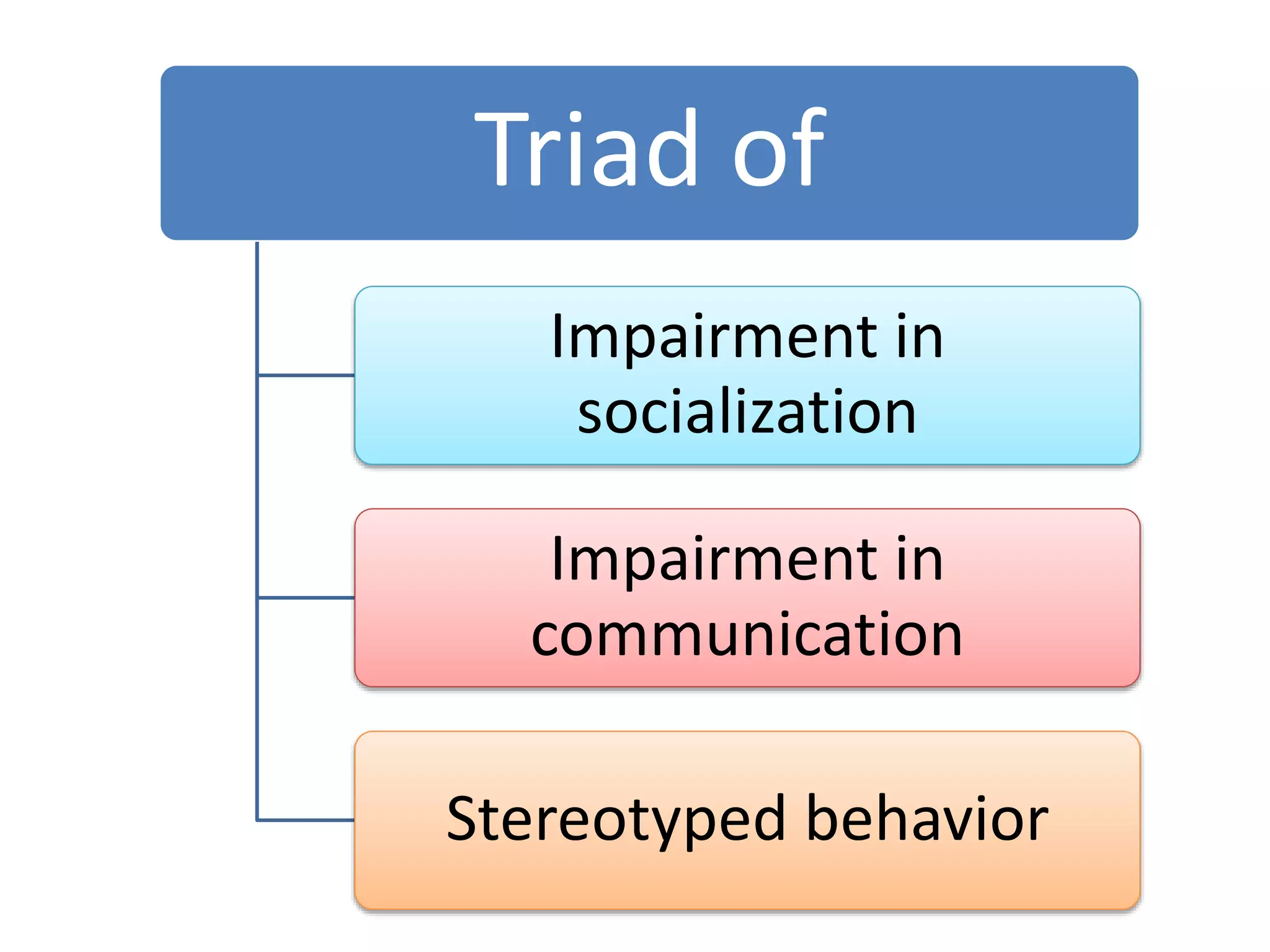
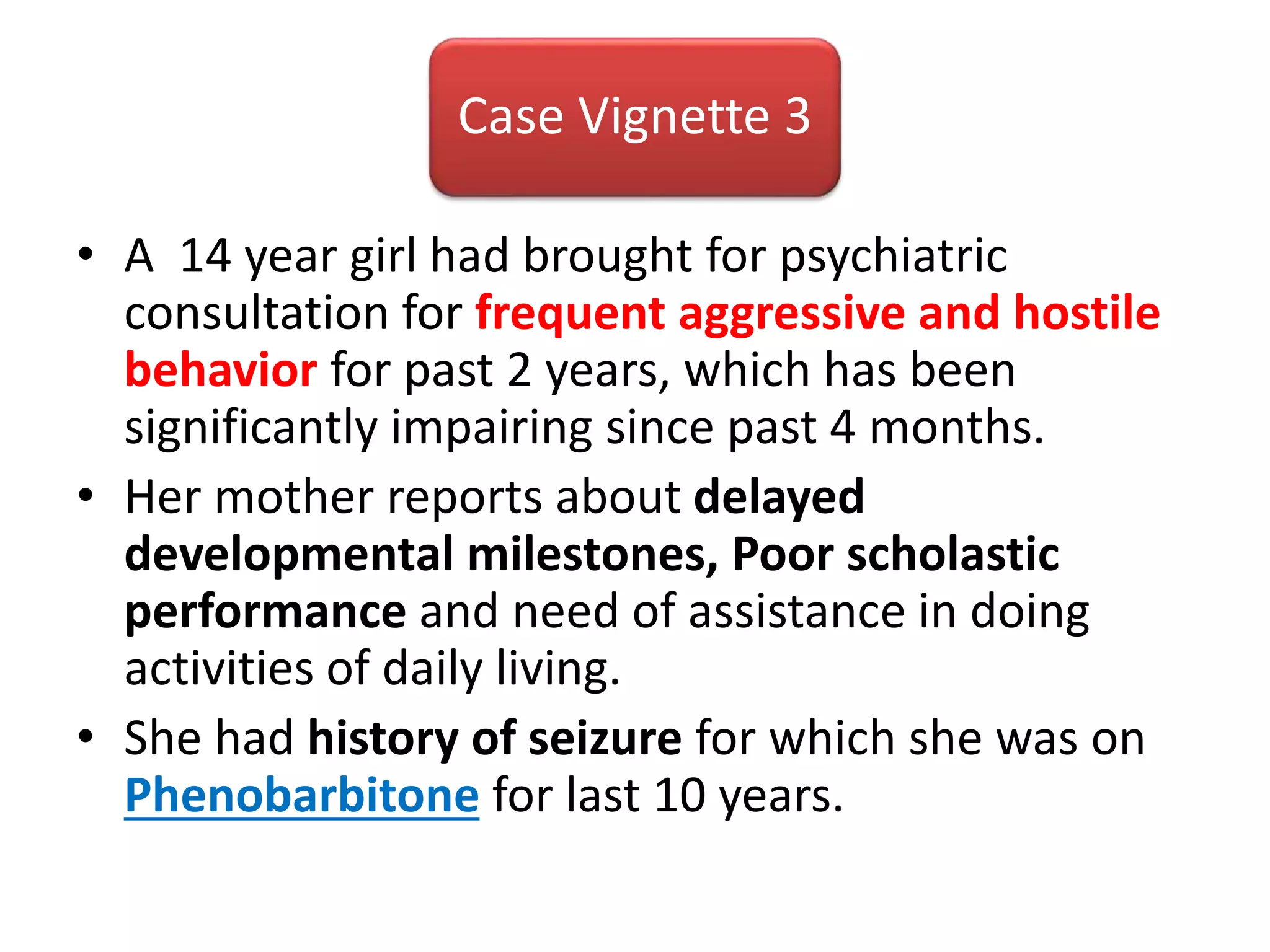
This document provides an overview of psychiatric disorders in pediatric populations. It discusses developmental disorders like intellectual disability, learning disorders, autism and ADHD. It also covers mood disorders, anxiety disorders, elimination disorders and others. The document includes case vignettes demonstrating specific learning disability, OCD with depression and dissociation, Dhat syndrome, intellectual disability with behavioral issues, and adjustment disorder. It discusses topics like parenting styles, early life adversities, and medical conditions that can impact scholastic performance or mimic physical illnesses.